Bibliography
The bibliography lists all references used in the online course.
- Topics:
- 1.1. HCV Epidemiology in the United States
- 1.1.1. HCV Incidence in the United States
- 1.1.2. HCV Prevalence in United States
- 1.1.3. HCV-Related Deaths
- 1.1.4. Risk Factors for Acquiring HCV
- 1.1.5. CDC Case Definitions and Reporting
- 1.2. Recommendations for Hepatitis C Screening
- 1.2.1. Current Hepatitis C Testing Recommendations
- 1.2.2. Rationale for Expanded HCV Screening of All Adults
- 1.2.3. HCV Testing for Infants and Children Exposed to HCV
- 1.3. Hepatitis C Diagnostic Testing
- 1.3.1. HCV Diagnostic Tests
- 1.3.2. HCV Testing Sequence
- 1.3.3. Interpreting and Communicating Test Results
- 1.3.4. Linkage to Care
- 1.3.A. Additional References
- 1.4. Counseling for Prevention of HCV Transmission
- 1.4.2. Sexual Transmission of HCV
- 1.4.3. Injection Drug Use and HCV Transmission
- 1.4.4. Household HCV Transmission
- 1.4.5. Perinatal HCV Transmission
- 1.5. Diagnosis of Acute HCV Infection
- 1.5.1. Definition of Acute HCV
- 1.5.2. Clinical Features of Acute HCV
- 1.5.3. Laboratory Studies Used for the Evaluation of Initial HCV Infection
- 1.5.4. Diagnosis of Acute HCV Infection
- 1.5.A. Additional References
- 2.1. Initial Evaluation of Persons with Chronic HCV
- 2.1.1. Background
- 2.1.2. General Approach to Initial Evaluation
- 2.1.3. Key Aspects of Medical History
- 2.1.4. Key Aspects of Physical Examination
- 2.1.5. Recommended Initial Laboratory Studies
- 2.1.6. Immunizations for Persons with Chronic HCV
- 2.1.7. Screening for other Causes of Liver Disease
- 2.2. Natural History of HCV Infection
- 2.2.1. Spontaneous Clearance versus Chronic Infection
- 2.2.2. Variable Outcomes of Chronic Infection
- 2.2.3. Host Factors that Impact Rate of Fibrosis Progression
- 2.2.A. Additional References
- 2.3. Counseling Persons with Chronic HCV Infection
- 2.3.2. Over-the-Counter Pain Medications
- 2.3.3. Iron and Vitamin Supplements
- 2.3.4. Complementary and Alternative Therapies
- 2.3.5. Coffee, Diet, and Sodium Intake
- 2.3.6. Modifying Obesity
- 2.3.7. Alcohol, Cannabis, and Tobacco
- 2.3.A. Additional References
- 2.4. Evaluation and Staging of Liver Fibrosis
- 2.4.1. Background
- 2.4.2. Indirect Markers for Estimating Hepatic Fibrosis
- 2.4.3. Direct Markers of Fibrosis
- 2.4.4. Radiologic Modalities to Estimate Fibrosis
- 2.4.5. Liver Biopsy and Histologic Assessment of the Liver
- 2.5. Evaluation and Prognosis of Persons with Cirrhosis
- 2.5.1. Background
- 2.5.2. Evaluation of Persons with Cirrhosis
- 2.5.3. Classification Systems for Persons with Cirrhosis
- 2.5.4. Compensated Cirrhosis
- 2.5.5. Decompensated Cirrhosis
- 2.6. Surveillance for Hepatocellular Carcinoma
- 2.6.1. Epidemiology
- 2.6.3. Benefit of HCC Surveillance with HCV Infection
- 2.6.4. Indications for HCC Surveillance
- 2.6.5. Surveillance Testing Methods
- 2.6.6. Guidance for HCC Surveillance
- 2.6.A. Additional References
- 2.7. Extrahepatic Conditions Related to HCV Infection
- 2.7.1. Overview of Extrahepatic Manifestations
- 2.7.2. Cryoglobulinemia
- 2.7.3. Autoimmune Disorders
- 2.7.4. Renal Disorders
- 2.7.5. Dermatologic Manifestations
- 2.7.6. Insulin Resistance and Type 2 Diabetes
- 2.7.7. Lymphomas
- 2.7.8. Cardiovascular Events
- 2.7.A. Additional References
- 3.1. Diagnosis and Management of Ascites
- 3.1.1. Background
- 3.1.2. Evaluation of Ascites
- 3.1.3. Analysis of Ascitic Fluid
- 3.1.4. Basic Management of Ascites
- 3.1.5. Management of Refractory Ascites
- 3.1.6. Complications Associated with Ascites
- 3.1.A. Additional References
- 3.2. Recognition and Management of Spontaneous Bacterial Peritonitis
- 3.2.1. Background
- 3.2.2. Diagnosis of Spontaneous Bacterial Peritonitis
- 3.2.3. Treatment of Spontaneous Bacterial Peritonitis
- 3.2.4. Indications for Spontaneous Bacterial Peritonitis Prophylaxis
- 3.2.5. Regimens for Spontaneous Bacterial Peritonitis Prophylaxis
- 3.2.A. Additional References
- 3.3. Screening for Varices and Prevention of Bleeding
- 3.3.1. Pathophysiology and Portal Dynamics
- 3.3.2. Diagnosing Clinically Significant Portal Hypertension and Predicting Varices
- 3.3.3. Management of Compensated Cirrhosis with Clinically Significant Portal Hypertension
- 3.3.4. Prophylaxis of Variceal Bleeding
- 3.3.5. Treatment of Acute Variceal Bleeding
- 3.3.6. Secondary Prophylaxis of Variceal Bleeding
- 3.4. Diagnosis and Management of Hepatic Encephalopathy
- 3.4.1. Background
- 3.4.2. Clinical Features
- 3.4.3. Diagnosis and Testing
- 3.4.4. Approach to the Management of Hepatic Encephalopathy
- 3.4.5. Medical Therapy for Overt Hepatic Encephalopathy
- 3.5. Referral for Liver Transplantation
- 3.5.1. Background
- 3.5.2. Indications for Liver Transplantation
- 3.5.3. Timing for Cirrhosis-Related Liver Transplantation
- 3.5.4. Contraindications to Liver Transplantation
- 3.5.5. Finding Information About Liver Transplant Centers
- 3.5.6. Transplantation Evaluation
- 4.1. Goals and Benefits with HCV Treatment
- 4.1.1. Background
- 4.1.2. Virologic Cure and Sustained Virologic Response
- 4.1.3. Impact of HCV Treatment on Clinical Outcomes
- 4.1.4. Impact of HCV Treatment on Quality of Life
- 4.1.5. Impact of HCV Treatment on Survival
- 4.1.6. Population-Level Benefits of HCV Elimination
- 4.1.A. Additional References
- 4.2. Making a Decision on When to Initiate HCV Therapy
- 4.2.1. Background
- 4.2.2. Indications for HCV Treatment
- 4.2.3. Contraindications for Treatment
- 4.2.5. Timing of Initiation of Treatment
- 4.2.6. Monitoring and Follow-Up if Not Treated
- 4.2.A. Additional References
- 4.3. Addressing Barriers to HCV Treatment
- 4.3.1. Background
- 4.3.2. The Path to HCV Cure: HCV Care Continuum
- 4.3.3. HCV Testing: Access, Efficiency, and Reimbursement
- 4.3.4. Improving Services for Linkage-to-Care
- 4.3.5. Expanding Medical Provider Capacity
- 4.3.6. Expanding Settings for HCV Clinical Care and Treatment
- 4.3.7. Insurance and Medicaid Restrictions to HCV Treatment Access
- 4.3.A. Additional References
- 5.1. Simplified HCV Treatment for All HCV Genotypes
- 5.1.1. Introduction
- 5.1.2. Eligibility for Simplified HCV Treatment: Initial Assessment
- 5.1.3. Simplified Treatment: Pretreatment Assessment for Patients without Cirrhosis
- 5.1.4. Recommended Simplified Treatment Regimens for Patients without Cirrhosis
- 5.1.5. Monitoring on and after HCV Treatment in Patients without Cirrhosis
- 5.1.6. Simplified Treatment: Pretreatment Assessment for Patients with Compensated Cirrhosis
- 5.1.7. Recommended Simplified Treatment Regimens for Patients with Compensated Cirrhosis
- 5.1.8. Monitoring On and After Treatment for Patients with Compensated Cirrhosis
- 5.1.9. Treatment Interruptions
- 5.1.A. Additional References
- 5.2. Retreatment of Patients with Prior HCV Treatment Experience
- 5.2.1. Introduction
- 5.2.2. Special Considerations with Retreatment
- 5.2.3. Treatment Failure with Sofosbuvir-Containing DAA or Elbasvir-Grazoprevir
- 5.2.4. Treatment Failure with Glecaprevir-Pibrentasvir
- 5.2.5. Treatment Failure with Multiple DAA Regimens
- 5.3. Monitoring During and After HCV Treatment
- 5.3.1. Background
- 5.3.2. Monitoring for Treatment Efficacy
- 5.3.3. Monitoring for Safety at Baseline and During Treatment
- 5.3.4. Hepatitis B Reactivation Associated with HCV DAA Therapy
- 5.3.5. Monitoring After Receiving HCV Therapy
- 5.3.A. Additional References
- 5.4. Treatment of HCV in Persons with Cirrhosis
- 5.4.1. Background
- 5.4.2. Impact of Treating HCV in Persons with Cirrhosis
- 5.4.3. Treating HCV in Persons with Compensated Cirrhosis
- 5.4.4. Treating HCV in Persons with Decompensated Cirrhosis
- 5.4.A. Additional References
- 5.5. Treatment of Acute HCV Infection
- 5.5.1. Background
- 5.5.2. Spontaneous Clearance of HCV Following Acute Infection
- 5.5.4. Acute HCV Treatment Data
- 5.5.5. AASLD-IDSA Guidance for Management of Acute HCV
- 6.1. Treatment of HCV in Persons with HIV Coinfection
- 6.1.1. Background of HIV-HCV Coinfection
- 6.1.2. HCV Treatment Data in Persons with HIV Coinfection
- 6.1.3. Treatment of HCV in Persons with HIV Coinfection
- 6.1.4. Treatment of HIV in Persons with HCV Coinfection
- 6.1.5. Drug Interactions with HIV-HCV Coinfection Treatment
- 6.2. Treatment of HCV in Persons with Renal Impairment
- 6.2.1. Background
- 6.2.2. HCV Treatment Studies in Persons with CKD
- 6.2.3. HCV Treatment in Persons with CKD
- 6.2.4. Treatment of HCV in Setting of Renal Transplantation
- 6.3. Treatment of HCV in Persons with Substance Use
- 6.3.1. Background
- 6.3.2. Approach to HCV Treatment in Persons with Substance Use
- 6.3.3. HCV Treatment in Persons with Opioid Use
- 6.3.4. HCV Treatment in Persons with Stimulant Use
- 6.3.5. HCV Treatment in Persons who Consume Alcohol
- 6.3.6. HCV Treatment in Persons who Use Cannabis
- 6.3.A. Additional References
- 6.4. Treatment of HCV in a Correctional Setting
- 6.4.1. Epidemiology of HCV in Corrections
- 6.4.2. HCV Screening in Correctional Settings
- 6.4.3. Management of HCV in Jails versus Prisons
- 6.4.4. HCV Treatment Eligibility in Corrections
- 6.4.5. Providing HCV Treatment in Correctional Settings
- 6.4.6. Ongoing Care after HCV Treatment
- 6.4.7. Public Health Opportunity
- 6.4.A. Additional References
- 6.5. Management of Health Care Personnel Exposed to HCV
- 6.5.1. Background
- 6.5.2. Risk of HCV Following Occupational Exposure
- 6.5.3. Approach to Managing Occupational Exposures to HCV
- 6.5.4. Monitoring Health Care Personnel after Occupational Exposure
- 6.5.5. Management of Persons who Seroconvert to HCV
- 6.5.A. Additional References
- 6.6. Perinatal HCV Transmission
- 6.6.1. Background
- 6.6.2. HCV Screening During Pregnancy
- 6.6.3. Factors Associated with HCV Perinatal Transmission
- 6.6.4. Impact of Chronic HCV Infection on Pregnancy
- 6.6.5. Effect of Pregnancy on Chronic HCV
- 6.6.6. Interventions to Prevent Mother-to-Child Transmission of HCV
- 6.6.7. Safety of HCV Treatment During Pregnancy and Breastfeeding
- 6.6.8. Monitoring of Pregnant Women with HCV
- 6.6.9. Management of Infants and Children Born to Mothers with HCV Infection
- 6.6.A. Additional References
Module 1. Screening and Diagnosis of Hepatitis C Infection
Lesson 1. HCV Epidemiology in the United States
HCV Incidence in the United States
Alter MJ, Gerety RJ, Smallwood LA, et al. Sporadic non-A, non-B hepatitis: frequency and epidemiology in an urban U.S. population. J Infect Dis. 1982;145:886-93.
PubMed Abstract»Alter MJ, Kruszon-Moran D, Nainan OV, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999;341:556-62.
PubMed Abstract»Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med. 2006;144:705-14.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). 2019 Viral Hepatitis Surveillance Report—Hepatitis C. Published May 2021.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2023. Published April 2025.
CDC»Centers for Disease Control and Prevention (CDC). National Notifiable Diseases Surveillance System (NNDSS). Hepatitis C, Acute: 2020 Case Definition.
CDC and NNDSS»Centers for Disease Control and Prevention (CDC). Viral Hepatitis Statistics and Surveillance. Table 1.1 Hepatitis C Outbreaks by Setting ― United States, 2015
CDC Viral Hepatitis Surveillance»Centers for Disease Control and Prevention (CDC). Viral Hepatitis Statistics and Surveillance—United States, 2016.
CDC Viral Hepatitis Surveillance»Chak E, Talal AH, Sherman KE, Schiff ER, Saab S. Hepatitis C virus infection in USA: an estimate of true prevalence. Liver Int. 2011;31:1090-101.
PubMed Abstract»Denniston MM, Jiles RB, Drobeniuc J, Klevens RM, Ward JW, McQuillan GM, Holmberg SD. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med. 2014;160:293-300.
PubMed Abstract»Denniston MM, Klevens RM, McQuillan GM, Jiles RB. Awareness of infection, knowledge of hepatitis C, and medical follow-up among individuals testing positive for hepatitis C: National Health and Nutrition Examination Survey 2001-2008. Hepatology. 2012;55:1652-61.
PubMed Abstract»Ditah I, Ditah F, Devaki P, et al. The changing epidemiology of hepatitis C virus infection in the United States: National Health and Nutrition Examination Survey 2001 through 2010. J Hepatol. 2013;60:691-8.
PubMed Abstract»Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015;62:1353-63.
PubMed Abstract»Gish RG, Cohen CA, Block JM, et al. Data supporting updating estimates of the prevalence of chronic hepatitis B and C in the United States. Hepatology. 2015;62:1339-41.
PubMed Abstract»Hagan H, Campbell J, Thiede H, et al. Self-reported hepatitis C virus antibody status and risk behavior in young injectors. Public Health Rep. 2006;121:710-9.
PubMed Abstract»Klevens RM, Liu S, Roberts H, Jiles RB, Holmberg SD. Estimating acute viral hepatitis infections from nationally reported cases. Am J Public Health. 2014;104:482-7.
PubMed Abstract»Manos MM, Shvachko VA, Murphy RC, Arduino JM, Shire NJ. Distribution of hepatitis C virus genotypes in a diverse US integrated health care population. J Med Virol. 2012;84:1744-50.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012;61:1-32.
PubMed Abstract»Spradling PR, Rupp L, Moorman AC, et al. Hepatitis B and C Virus Infection Among 1.2 Million Persons With Access to Care: Factors Associated With Testing and Infection Prevalence. Clin Infect Dis. 2012;55:1047-55.
PubMed Abstract»Suryaprasad AG, White JZ, Xu F, et al. Emerging epidemic of hepatitis C virus infections among young nonurban persons who inject drugs in the United States, 2006-2012. Clin Infect Dis. 2014;59:1411-9.
PubMed Abstract»Zibbell JE, Asher AK, Patel RC, et al. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am J Public Health. 2018;108:175-181.
PubMed Abstract»Zibbell JE, Hart-Malloy R, Barry J, Fan L, Flanigan C. Risk factors for HCV infection among young adults in rural New York who inject prescription opioid analgesics. Am J Public Health. 2014;104:2226-32.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»HCV Prevalence in United States
Alter MJ, Kruszon-Moran D, Nainan OV, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999;341:556-62.
PubMed Abstract»Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med. 2006;144:705-14.
PubMed Abstract»Bradley H, Hall EW, Rosenthal EM, Sullivan PS, Ryerson AB, Rosenberg ES. Hepatitis C Virus Prevalence in 50 U.S. States and D.C. by Sex, Birth Cohort, and Race: 2013-2016. Hepatol Commun. 2020;4:355-70.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). 2019 Viral Hepatitis Surveillance Report—Hepatitis C. Published May 2021.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2023. Published April 2025.
CDC»Centers for Disease Control and Prevention (CDC). Viral Hepatitis Statistics and Surveillance—United States, 2016.
CDC Viral Hepatitis Surveillance»Chak E, Talal AH, Sherman KE, Schiff ER, Saab S. Hepatitis C virus infection in USA: an estimate of true prevalence. Liver Int. 2011;31:1090-101.
PubMed Abstract»Denniston MM, Jiles RB, Drobeniuc J, Klevens RM, Ward JW, McQuillan GM, Holmberg SD. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med. 2014;160:293-300.
PubMed Abstract»Denniston MM, Klevens RM, McQuillan GM, Jiles RB. Awareness of infection, knowledge of hepatitis C, and medical follow-up among individuals testing positive for hepatitis C: National Health and Nutrition Examination Survey 2001-2008. Hepatology. 2012;55:1652-61.
PubMed Abstract»Ditah I, Ditah F, Devaki P, et al. The changing epidemiology of hepatitis C virus infection in the United States: National Health and Nutrition Examination Survey 2001 through 2010. J Hepatol. 2013;60:691-8.
PubMed Abstract»Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015;62:1353-63.
PubMed Abstract»Germer JJ, Mandrekar JN, Bendel JL, Mitchell PS, Yao JD. Hepatitis C virus genotypes in clinical specimens tested at a national reference testing laboratory in the United States. J Clin Microbiol. 2011;49:3040-3.
PubMed Abstract»Guss D, Sherigar J, Rosen P, Mohanty SR. Diagnosis and Management of Hepatitis C Infection in Primary Care Settings. J Gen Intern Med. 2018;33:551-7.
PubMed Abstract»Hagan H, Campbell J, Thiede H, et al. Self-reported hepatitis C virus antibody status and risk behavior in young injectors. Public Health Rep. 2006;121:710-9.
PubMed Abstract»Hofmeister MG, Rosenthal EM, Barker LK, et al. Estimating Prevalence of Hepatitis C Virus Infection in the United States, 2013-2016. Hepatology. 2019;69:1020-31.
PubMed Abstract»Kim HS, Yang JD, El-Serag HB, Kanwal F. Awareness of chronic viral hepatitis in the United States: An update from the National Health and Nutrition Examination Survey. J Viral Hepat. 2019;26:596-602.
PubMed Abstract»Lewis KC, Barker LK, Jiles RB, Gupta N. Estimated Prevalence and Awareness of Hepatitis C Virus Infection Among US Adults: National Health and Nutrition Examination Survey, January 2017-March 2020. Clin Infect Dis. 2023;77:1413-5.
PubMed Abstract»Manos MM, Shvachko VA, Murphy RC, Arduino JM, Shire NJ. Distribution of hepatitis C virus genotypes in a diverse US integrated health care population. J Med Virol. 2012;84:1744-50.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012;61:1-32.
PubMed Abstract»Spradling PR, Rupp L, Moorman AC, et al. Hepatitis B and C Virus Infection Among 1.2 Million Persons With Access to Care: Factors Associated With Testing and Infection Prevalence. Clin Infect Dis. 2012;55:1047-55.
PubMed Abstract»HCV-Related Deaths
Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2023. Published April 2025.
CDC»Centers for Disease Control and Prevention (CDC). Viral Hepatitis Statistics and Surveillance—United States, 2016.
CDC Viral Hepatitis Surveillance»Chhatwal J, Wang X, Ayer T, et al. Hepatitis C Disease Burden in the United States in the era of oral direct-acting antivirals. Hepatology. 2016;64:1442-1450.
PubMed Abstract»Davis GL, Albright JE, Cook SF, Rosenberg DM. Projecting future complications of chronic hepatitis C in the United States. Liver Transpl. 2003;9:331-8.
PubMed Abstract»Davis GL, Alter MJ, El-Serag H, Poynard T, Jennings LW. Aging of hepatitis C virus (HCV)-infected persons in the United States: a multiple cohort model of HCV prevalence and disease progression. Gastroenterology. 2010;138:513-21, 521.e1-6.
PubMed Abstract»Davis KL, Mitra D, Medjedovic J, Beam C, Rustgi V. Direct economic burden of chronic hepatitis C virus in a United States managed care population. J Clin Gastroenterol. 2011;45:e17-24.
PubMed Abstract»Deuffic-Burban S, Poynard T, Sulkowski MS, Wong JB. Estimating the future health burden of chronic hepatitis C and human immunodeficiency virus infections in the United States. J Viral Hepat. 2007;14:107-15.
PubMed Abstract»Durham DP, Skrip LA, Bruce RD, et al. The Impact of Enhanced Screening and Treatment on Hepatitis C in the United States. Clin Infect Dis. 2015;62:298-304.
PubMed Abstract»El-Kamary SS, Jhaveri R, Shardell MD. All-cause, liver-related, and non-liver-related mortality among HCV-infected individuals in the general US population. Clin Infect Dis. 2011;53:150-7.
PubMed Abstract»Ioannou GN, Green PK, Berry K. HCV eradication induced by direct-acting antiviral agents reduces the risk of hepatocellular carcinoma. J Hepatol. 2017. pii: S0168-8278(17)32273-0.
PubMed Abstract»Ly KN, Hughes EM, Jiles RB, Holmberg SD. Rising Mortality Associated With Hepatitis C Virus in the United States, 2003-2013. Clin Infect Dis. 2016;62:1287-8.
PubMed Abstract»Ly KN, Xing J, Klevens RM, Jiles RB, Ward JW, Holmberg SD. The increasing burden of mortality from viral hepatitis in the United States between 1999 and 2007. Ann Intern Med. 2012;156:271-8.
PubMed Abstract»Mahajan R, Xing J, Liu SJ, et al. Mortality among persons in care with hepatitis C virus infection: the Chronic Hepatitis Cohort Study (CHeCS), 2006-2010. Clin Infect Dis. 2014;58:1055-61.
PubMed Abstract»Rein DB, Wittenborn JS, Weinbaum CM, Sabin M, Smith BD, Lesesne SB. Forecasting the morbidity and mortality associated with prevalent cases of pre-cirrhotic chronic hepatitis C in the United States. Dig Liver Dis. 2011;43:66-72.
PubMed Abstract»Singer AW, Reddy KR, Telep LE, et al. Direct-acting antiviral treatment for hepatitis C virus infection and risk of incident liver cancer: a retrospective cohort study. Aliment Pharmacol Ther. 2018;47:1278-1287.
PubMed Abstract»Su J, Brook RA, Kleinman NL, Corey-Lisle P. The impact of hepatitis C virus infection on work absence, productivity, and healthcare benefit costs. Hepatology. 2010;52:436-42.
PubMed Abstract»Wise M, Bialek S, Finelli L, Bell BP, Sorvillo F. Changing trends in hepatitis C-related mortality in the United States, 1995-2004. Hepatology. 2008;47:1128-35.
PubMed Abstract»Risk Factors for Acquiring HCV
Ackerman Z, Ackerman E, Paltiel O. Intrafamilial transmission of hepatitis C virus: a systematic review. J Viral Hepat. 2000;7:93-103.
PubMed Abstract»Alter HJ, Houghton M. Clinical Medical Research Award. Hepatitis C virus and eliminating post-transfusion hepatitis. Nat Med. 2000;6:1082-6.
PubMed Abstract»Alter MJ, Gerety RJ, Smallwood LA, et al. Sporadic non-A, non-B hepatitis: frequency and epidemiology in an urban U.S. population. J Infect Dis. 1982;145:886-93.
PubMed Abstract»Benova L, Mohamoud YA, Calvert C, Abu-Raddad LJ. Vertical transmission of hepatitis C virus: systematic review and meta-analysis. Clin Infect Dis. 2014;59:765-73.
PubMed Abstract»Bjøro K, Frøland SS, Yun Z, Samdal HH, Haaland T. Hepatitis C infection in patients with primary hypogammaglobulinemia after treatment with contaminated immune globulin. N Engl J Med. 1994;331:1607-11.
PubMed Abstract»Bresee JS, Mast EE, Coleman PJ, et al. Hepatitis C virus infection associated with administration of intravenous immune globulin. A cohort study. JAMA. 1996;276:1563-7.
PubMed Abstract»Busch MP. Transfusion-transmitted viral infections: building bridges to transfusion medicine to reduce risks and understand epidemiology and pathogenesis. Transfusion. 2006;46:1624-40.
PubMed Abstract»Carney K, Dhalla S, Aytaman A, Tenner CT, Francois F. Association of tattooing and hepatitis C virus infection: a multicenter case-control study. Hepatology. 2013;57:2117-23.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C virus infection among adolescents and young adults: Massachusetts, 2002-2009. MMWR Morb Mortal Wkly Rep. 2011;60:537-41.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Hepatitis C virus transmission at an outpatient hemodialysis unit--New York, 2001-2008. MMWR Morb Mortal Wkly Rep. 2009;58:189-94.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Notes from the field: hepatitis C virus infections among young adults--rural Wisconsin, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:358.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Outbreak of hepatitis C associated with intravenous immunoglobulin administration--United States, October 1993-June 1994. MMWR Morb Mortal Wkly Rep. 1994;43:505-9.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Recommendations for preventing transmission of infections among chronic hemodialysis patients. MMWR Recomm Rep. 2001;50:1-43.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Sexual transmission of hepatitis C virus among HIV-infected men who have sex with men--New York City, 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60:945-50.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Transmission of hepatitis C virus through transplanted organs and tissue--Kentucky and Massachusetts, 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1697-700.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Use of enhanced surveillance for hepatitis C virus infection to detect a cluster among young injection-drug users--New York, November 2004-April 2007. MMWR Morb Mortal Wkly Rep. 2008;57:517-21.
PubMed Abstract»Diago M, Zapater R, Tuset C, et al. Intrafamily transmission of hepatitis C virus: sexual and non-sexual contacts. J Hepatol. 1996;25:125-8.
PubMed Abstract»Ditah I, Ditah F, Devaki P, et al. The changing epidemiology of hepatitis C virus infection in the United States: National Health and Nutrition Examination Survey 2001 through 2010. J Hepatol. 2013;60:691-8.
PubMed Abstract»Donahue JG, Muñoz A, Ness PM, et al. The declining risk of post-transfusion hepatitis C virus infection. N Engl J Med. 1992;327:369-73.
PubMed Abstract»Garg S, Taylor LE, Grasso C, Mayer KH. Prevalent and incident hepatitis C virus infection among HIV-infected men who have sex with men engaged in primary care in a Boston community health center. Clin Infect Dis. 2013;56:1480-7.
PubMed Abstract»Gorgos L. Sexual transmission of viral hepatitis. Infect Dis Clin North Am. 2013;27:811-36.
PubMed Abstract»Guss D, Sherigar J, Rosen P, Mohanty SR. Diagnosis and Management of Hepatitis C Infection in Primary Care Settings. J Gen Intern Med. 2018;33:551-7.
PubMed Abstract»Hagan H, Pouget ER, Des Jarlais DC, Lelutiu-Weinberger C. Meta-regression of hepatitis C virus infection in relation to time since onset of illicit drug injection: the influence of time and place. Am J Epidemiol. 2008;168:1099-109.
PubMed Abstract»Hagan H, Thiede H, Weiss NS, Hopkins SG, Duchin JS, Alexander ER. Sharing of drug preparation equipment as a risk factor for hepatitis C. Am J Public Health. 2001;91:42-6.
PubMed Abstract»Handanagic S, Finlayson T, Burnett JC, Broz D, Wejnert C. HIV Infection and HIV-Associated Behaviors Among Persons Who Inject Drugs - 23 Metropolitan Statistical Areas, United States, 2018. MMWR Morb Mortal Wkly Rep. 2021;70:1459-65.
PubMed Abstract»Holtzman D, Barry V, Ouellet LJ, et al. The influence of needle exchange programs on injection risk behaviors and infection with hepatitis C virus among young injection drug users in select cities in the United States, 1994-2004. Prev Med. 2009;49:68-73.
PubMed Abstract»Hoornenborg E, Achterbergh RCA, Schim van der Loeff MF, et al. MSM starting preexposure prophylaxis are at risk of hepatitis C virus infection. AIDS. 2017;31:1603-1610.
PubMed Abstract»Jin F, Matthews GV, Grulich AE. Sexual transmission of hepatitis C virus among gay and bisexual men: a systematic review. Sex Health. 2017;14:28-41.
PubMed Abstract»Kao JH, Liu CJ, Chen PJ, Chen W, Lai MY, Chen DS. Low incidence of hepatitis C virus transmission between spouses: a prospective study. J Gastroenterol Hepatol. 2000;15:391-5.
PubMed Abstract»Klevens RM, Hu DJ, Jiles R, Holmberg SD. Evolving epidemiology of hepatitis C virus in the United States. Clin Infect Dis. 2012;55 Suppl 1:S3-9.
PubMed Abstract»Koneru A, Nelson N, Hariri S, et al. Increased Hepatitis C Virus (HCV) Detection in Women of Childbearing Age and Potential Risk for Vertical Transmission - United States and Kentucky, 2011-2014. MMWR Morb Mortal Wkly Rep. 2016;65:705-10.
PubMed Abstract»Ly KN, Jiles RB, Teshale EH, Foster MA, Pesano RL, Holmberg SD. Hepatitis C Virus Infection Among Reproductive-Aged Women and Children in the United States, 2006 to 2014. Ann Intern Med. 2017;166:775-782.
PubMed Abstract»Muleta D, Kainer MA, Moore-Moravian L, et al. Notes from the Field: Hepatitis C Outbreak in a Dialysis Clinic--Tennessee, 2014. MMWR Morb Mortal Wkly Rep. 2016;64:1386-7.
PubMed Abstract»Murphy EL, Bryzman SM, Glynn SA, et al. Risk factors for hepatitis C virus infection in United States blood donors. NHLBI Retrovirus Epidemiology Donor Study (REDS). Hepatology. 2000;31:756-62.
PubMed Abstract»Nguyen DB, Gutowski J, Ghiselli M, et al. A Large Outbreak of Hepatitis C Virus Infections in a Hemodialysis Clinic. Infect Control Hosp Epidemiol. 2016;37:125-33.
PubMed Abstract»Page CM, Hughes BL, Rhee EHJ, Kuller JA. Hepatitis C in Pregnancy: Review of Current Knowledge and Updated Recommendations for Management. Obstet Gynecol Surv. 2017;72:347-355.
PubMed Abstract»Panagiotakopoulos L, Sandul AL, Conners EE, Foster MA, Nelson NP, Wester C. CDC Recommendations for Hepatitis C Testing Among Perinatally Exposed Infants and Children - United States, 2023. MMWR Recomm Rep. 2023;72:1-21.
PubMed Abstract»Patel PR, Thompson ND, Kallen AJ, Arduino MJ. Epidemiology, surveillance, and prevention of hepatitis C virus infections in hemodialysis patients. Am J Kidney Dis. 2010;56:371-8.
PubMed Abstract»Perkins HA, Busch MP. Transfusion-associated infections: 50 years of relentless challenges and remarkable progress. Transfusion. 2010;50:2080-99.
PubMed Abstract»Piazza M. Immunoglobulin transmits hepatitis C. True or false? Hepatology. 1999;29:299-300.
PubMed Abstract»Post JJ. Update on hepatitis C and implications for pregnancy. Obstet Med. 2017;10:157-160.
PubMed Abstract»Pouget ER, Hagan H, Des Jarlais DC. Meta-analysis of hepatitis C seroconversion in relation to shared syringes and drug preparation equipment. Addiction. 2012;107:1057-65.
PubMed Abstract»Scheinmann R, Hagan H, Lelutiu-Weinberger C, Stern R, Des Jarlais DC, Flom PL, Strauss S.
Non-injection drug use and hepatitis C virus: a systematic review. Drug Alcohol Depend. 2007;89:1-12.
PubMed Abstract»Seem DL, Lee I, Umscheid CA, Kuehnert MJ. PHS guideline for reducing human immunodeficiency virus, hepatitis B virus, and hepatitis C virus transmission through organ transplantation. Public Health Rep. 2013;128:247-343.
PubMed Abstract»Shimokura G, Chai F, Weber DJ, et al. Patient-care practices associated with an increased prevalence of hepatitis C virus infection among chronic hemodialysis patients. Infect Control Hosp Epidemiol. 2011;32:415-24.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012;61:1-32.
PubMed Abstract»Stramer SL. Current risks of transfusion-transmitted agents: a review. Arch Pathol Lab Med. 2007;131:702-7.
PubMed Abstract»Suryaprasad AG, White JZ, Xu F, et al. Emerging epidemic of hepatitis C virus infections among young nonurban persons who inject drugs in the United States, 2006-2012. Clin Infect Dis. 2014;59:1411-9.
PubMed Abstract»Tahan V, Karaca C, Yildirim B, et al. Sexual transmission of HCV between spouses. Am J Gastroenterol. 2005;100:821-4.
PubMed Abstract»Terrault NA, Dodge JL, Murphy EL, Tavis JE, Kiss A, Levin TR, Gish RG, Busch MP, Reingold AL, Alter MJ. Sexual transmission of hepatitis C virus among monogamous heterosexual couples: the HCV partners study. Hepatology. 2013;57:881-9.
PubMed Abstract»Terrault NA. Sexual activity as a risk factor for hepatitis C. Hepatology. 2002;36(5 Suppl 1):S99-105.
PubMed Abstract»Thompson ND, Novak RT, Datta D, et al. Hepatitis C virus transmission in hemodialysis units: importance of infection control practices and aseptic technique. Infect Control Hosp Epidemiol. 2009;30:900-3.
PubMed Abstract»Tohme RA, Holmberg SD. Is sexual contact a major mode of hepatitis C virus transmission? Hepatology. 2010;52:1497-505.
PubMed Abstract»Tohme RA, Holmberg SD. Transmission of hepatitis C virus infection through tattooing and piercing: a critical review. Clin Infect Dis. 2012;54:1167-78.
PubMed Abstract»Troisi CL, Hollinger FB, Hoots WK, et al. A multicenter study of viral hepatitis in a United States hemophilic population. Blood. 1993;81:412-8.
PubMed Abstract»Tugwell BD, Patel PR, Williams IT, et al. Transmission of hepatitis C virus to several organ and tissue recipients from an antibody-negative donor. Ann Intern Med. 2005;143:648-54.
PubMed Abstract»Urbanus AT, Van De Laar TJ, Geskus R, et al. Trends in hepatitis C virus infections among MSM attending a sexually transmitted infection clinic; 1995-2010. AIDS. 2014;28:781-90.
PubMed Abstract»Vandelli C, Renzo F, Romanò L, et al. Lack of evidence of sexual transmission of hepatitis C among monogamous couples: results of a 10-year prospective follow-up study. Am J Gastroenterol. 2004;99:855-9.
PubMed Abstract»Williams I. Epidemiology of hepatitis C in the United States. Am J Med. 1999;107(6B):2S-9S.
PubMed Abstract»Williams IT, Bell BP, Kuhnert W, Alter MJ. Incidence and transmission patterns of acute hepatitis C in the United States, 1982-2006. Arch Intern Med. 2011;171:242-8.
PubMed Abstract»Witkop ML, Peerlinck K, Luxon BA. Medical co-morbidities of patients with haemophilia: pain, obesity and hepatitis C. Haemophilia. 2016;22 Suppl 5:47-53.
PubMed Abstract»Zibbell JE, Asher AK, Patel RC, et al. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am J Public Health. 2018;108:175-181.
PubMed Abstract»Zibbell JE, Hart-Malloy R, Barry J, Fan L, Flanigan C. Risk factors for HCV infection among young adults in rural New York who inject prescription opioid analgesics. Am J Public Health. 2014;104:2226-32.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»Zoulim F, Bailly F. New approaches to the management of hepatitis C in haemophilia in 2012. Haemophilia. 2012;18 Suppl 4:28-33.
PubMed Abstract»CDC Case Definitions and Reporting
Centers for Disease Control and Prevention (CDC). National Notifiable Diseases Surveillance System (NNDSS). Hepatitis C, acute: 2016 case definition.
CDC and NNDSS»Centers for Disease Control and Prevention (CDC). National Notifiable Diseases Surveillance System (NNDSS). Hepatitis C, Acute: 2020 Case Definition.
CDC and NNDSS»Centers for Disease Control and Prevention (CDC). National Notifiable Diseases Surveillance System (NNDSS). Hepatitis C, Chronic: 2020 Case Definition.
CDC and NNDSS»Centers for Disease Control and Prevention (CDC). National Notifiable Diseases Surveillance System (NNDSS). Hepatitis C, Perinatal Infection: 2018 Case Definition.
CDC and NNDSS»Binka M, Paintsil E, Patel A, Lindenbach BD, Heimer R. Survival of Hepatitis C Virus in Syringes Is Dependent on the Design of the Syringe-Needle and Dead Space Volume. PLoS One. 2015;10:e0139737.
PubMed Abstract»Paintsil E, Binka M, Patel A, Lindenbach BD, Heimer R. Hepatitis C virus maintains infectivity for weeks after drying on inanimate surfaces at room temperature: implications for risks of transmission. J Infect Dis. 2014;209:1205-11.
PubMed Abstract»Rosenberg ES, Rosenthal EM, Hall EW, et al. Prevalence of Hepatitis C Virus Infection in US States and the District of Columbia, 2013 to 2016. JAMA Netw Open. 2018;1:e186371.
PubMed Abstract»Wyles D, Weiland O, Yao B, et al. Retreatment of patients who failed glecaprevir/pibrentasvir treatment for hepatitis C virus infection. J Hepatol. 2019;70:1019-23.
PubMed Abstract»Lesson 2. Recommendations for Hepatitis C Screening
Current Hepatitis C Testing Recommendations
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»Centers for Disease Control and Prevention. CDC Recommendations for Hepatitis C Screening Among Adults [DRAFT Recommendations].
CDC»Chou R, Cottrell EB, Wasson N, Rahman B, Guise JM. Screening for hepatitis C virus infection in adults: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;158:101-8.
PubMed Abstract»Chou R, Dana T, Fu R, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2020;323:1318.
PubMed Abstract»Moyer VA; U.S. Preventive Services Task Force. Screening for hepatitis C virus infection in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:51-60.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012;61:1-32.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Ward JW. Hepatitis C virus testing of persons born during 1945-1965: recommendations from the Centers for Disease Control and Prevention. Ann Intern Med. 2012;157:817-22.
PubMed Abstract»U.S. Preventive Services Task Force. Final Recommendation Statement. Hepatitis C: Screening. March 2, 2020.
USPSTF»U.S. Preventive Services Task Force. Screening for hepatitis C virus infection in adults: recommendation statement. Ann Intern Med. 2004;140:462-4.
Ann Intern Med»US Preventive Services Task Force, Owens DK, Davidson KW, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;323:970-5.
PubMed Abstract»Rationale for Expanded HCV Screening of All Adults
Alkhouri N, Lawitz E, Poordad F. Novel treatments for chronic hepatitis C: closing the remaining gaps. Curr Opin Pharmacol. 2017;37:107-11.
PubMed Abstract»Barocas JA, Tasillo A, Eftekhari Yazdi G, et al. Population-level Outcomes and Cost-Effectiveness of Expanding the Recommendation for Age-based Hepatitis C Testing in the United States. Clin Infect Dis. 2018;67:549-56.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). 2019 Viral Hepatitis Surveillance Report—Hepatitis C. Published May 2021.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Chou R, Dana T, Fu R, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2020;323:1318.
PubMed Abstract»Coffin PO, Scott JD, Golden MR, Sullivan SD. Cost-effectiveness and population outcomes of general population screening for hepatitis C. Clin Infect Dis. 2012;54:1259-71.
PubMed Abstract»Cui F, Blach S, Manzengo Mingiedi C, et al. Global reporting of progress towards elimination of hepatitis B and hepatitis C. Lancet Gastroenterol Hepatol. 2023;8:332-42.
PubMed Abstract»Durham DP, Skrip LA, Bruce RD, et al. The Impact of Enhanced Screening and Treatment on Hepatitis C in the United States. Clin Infect Dis. 2015;62:298-304.
PubMed Abstract»Fraser H, Martin NK, Brummer-Korvenkontio H, et al. Model projections on the impact of HCV treatment in the prevention of HCV transmission among people who inject drugs in Europe. J Hepatol. 2018;68:402-11.
PubMed Abstract»Graham CS, Trooskin S. Universal Screening for Hepatitis C Virus Infection: A Step Toward Elimination. JAMA. 2020 Mar 2. [Epub ahead of print]
PubMed Abstract»Heffernan A, Cooke GS, Nayagam S, Thursz M, Hallett TB. Scaling up prevention and treatment towards the elimination of hepatitis C: a global mathematical model. Lancet. 2019;393:1319-29.
PubMed Abstract»Kabiri M, Jazwinski AB, Roberts MS, Schaefer AJ, Chhatwal J. The changing burden of hepatitis C virus infection in the United States: model-based predictions. Ann Intern Med. 2014;161:170-80.
PubMed Abstract»Ogawa E, Chien N, Kam L, et al. Association of Direct-Acting Antiviral Therapy With Liver and Nonliver Complications and Long-term Mortality in Patients With Chronic Hepatitis C. JAMA Intern Med. 2023;183:97-105.
PubMed Abstract»Olafsson S, Tyrfingsson T, Runarsdottir V, et al. Treatment as Prevention for Hepatitis C (TraP Hep C) - a nationwide elimination programme in Iceland using direct-acting antiviral agents. J Intern Med. 2018;283:500-7.
PubMed Abstract»Parikh ND, Mehta N, Hoteit MA, et al. Association between sustained virological response and clinical outcomes in patients with hepatitis C infection and hepatocellular carcinoma. Cancer. 2022;128:3470-78.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»van Santen DK, Sacks-Davis R, Stewart A, et al. Treatment as prevention effect of direct-acting antivirals on primary hepatitis C virus incidence: Findings from a multinational cohort between 2010 and 2019. EClinicalMedicine. 2023;56:101810.
PubMed Abstract»Zelenev A, Li J, Mazhnaya A, Basu S, Altice FL. Hepatitis C virus treatment as prevention in an extended network of people who inject drugs in the USA: a modelling study. Lancet Infect Dis. 2018;18:215-24.
PubMed Abstract»Zibbell JE, Asher AK, Patel RC, et al. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am J Public Health. 2018;108:175-181.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»HCV Testing for Infants and Children Exposed to HCV
Centers for Disease Control and Prevention (CDC). Locations and reasons for initial testing for hepatitis C infection - chronic hepatitis cohort study, United States, 2006-2010. MMWR Morb Mortal Wkly Rep. 2013;62:645-8.
CDC and MMWR»Centers for Disease Control and Prevention. Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. Centers for Disease Control and Prevention. MMWR Recomm Rep. 1998;47(RR-19):1-39.
CDC and MMWR»Chou R, Clark EC, Helfand M; U.S. Preventive Services Task Force. Screening for hepatitis C virus infection: a review of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140:465-79.
PubMed Abstract»Denniston MM, Klevens RM, McQuillan GM, Jiles RB. Awareness of infection, knowledge of hepatitis C, and medical follow-up among individuals testing positive for hepatitis C: National Health and Nutrition Examination Survey 2001-2008. Hepatology. 2012;55:1652-61.
PubMed Abstract»Ely DM, Gregory ECW. Trends and Characteristics in Maternal Hepatitis C Virus Infection Rates During Pregnancy: United States, 2016–2021. National Vital Statistics Reports. 2023:72(3).
CDC Stacks»Moyer VA; U.S. Preventive Services Task Force. Screening for hepatitis C virus infection in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:51-60.
PubMed Abstract»NIH Consensus Statement on Management of Hepatitis C: 2002. NIH Consens State Sci Statements. 2002;19:1-46.
PubMed Abstract»Panagiotakopoulos L, Sandul AL, Conners EE, Foster MA, Nelson NP, Wester C. CDC Recommendations for Hepatitis C Testing Among Perinatally Exposed Infants and Children - United States, 2023. MMWR Recomm Rep. 2023;72:1-21.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012;61:1-32.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Ward JW. Hepatitis C virus testing of persons born during 1945-1965: recommendations from the Centers for Disease Control and Prevention. Ann Intern Med. 2012;157:817-22.
PubMed Abstract»U.S. Preventive Services Task Force. Screening for hepatitis C virus infection in adults: recommendation statement. Ann Intern Med. 2004;140:462-4.
Ann Intern Med»Ward JW. The epidemiology of chronic hepatitis C and one-time hepatitis C virus testing of persons born during 1945 to 1965 in the United States. Clin Liver Dis. 2013;17:1-11.
PubMed Abstract»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection: treatment-naive genotype 4 with compensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection: treatment-naive genotype 4 without cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection.
AASLD-IDSA Hepatitis C Guidance»Abergel A, Metivier S, Samuel D, et al. Ledipasvir plus sofosbuvir for 12 weeks in patients with hepatitis C genotype 4 infection. Hepatology. 2016;64:1049-56.
PubMed Abstract»Al-Ali J, Siddique I, Varghese R, Hasan F. Pegylated interferon-alpha2b plus ribavirin for the treatment of chronic hepatitis C virus genotype 4 infection in patients with normal serum ALT. Ann Hepatol. 2012;11:186-93.
PubMed Abstract»Allam WR, Barakat A, Zakaria Z, et al. Schistosomiasis does not affect the outcome of HCV infection in genotype 4-infected patients. Am J Trop Med Hyg. 2014;90:823-9.
PubMed Abstract»Asselah T, Bourlière M. Hepatitis C Virus: Current and Evolving Treatments for Genotype 4. Gastroenterol Clin North Am. 2015;44:859-70.
PubMed Abstract»Asselah T, Esmat G, Sanai FM, et al. Simple Predictive Model for Identifying Patients with Chronic Hepatitis C and Hepatitis C Virus Genotype 4 Infection with a High Probability of Sustained Virologic Response with Peginterferon Alfa-2a/Ribavirin: Pooled Analysis of Data from Two Large, International Cohort Studies. Adv Ther. 2016;33:1797-1813.
PubMed Abstract»Asselah T, Kowdley KV, Zadeikis N, et al. Efficacy of Glecaprevir/Pibrentasvir for 8 or 12 Weeks in Patients With Hepatitis C Virus Genotype 2, 4, 5, or 6 Infection Without Cirrhosis. Clin Gastroenterol Hepatol. 2018;16:417-26.
PubMed Abstract»Asselah T, Reesink HW, Gerstoft J, et al. High Efficacy of Elbasvir and Grazoprevir with or Without Ribavirin in 103 Treatment-Naive and Experienced Patients with HCV Genotype 4 infection: A Pooled Analysis. Presented at the 66th Annual Meeting of the American Association for the Study of Liver Diseases. San Francisco, CA. November 13-17, 2015. Abstract 251.
NATAP»Brady JE, Liffmann DK, Yartel A, et al. Uptake of hepatitis C screening, characteristics of patients tested, and intervention costs in the BEST-C study. Hepatology. 2017;65:44-53.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»De Nicola S, Aghemo A, Rumi MG, et al. Interleukin 28B polymorphism predicts pegylated interferon plus ribavirin treatment outcome in chronic hepatitis C genotype 4. Hepatology. 2012;55:336-42.
PubMed Abstract»Diago M, Hassanein T, Rodés J, Ackrill AM, Sedarati F. Optimized virologic response in hepatitis C virus genotype 4 with peginterferon-alpha2a and ribavirin. Ann Intern Med. 2004;140:72-3.
PubMed Abstract»Doss W, Shiha G, Hassany M, et al. Sofosbuvir plus ribavirin for treating Egyptian patients with hepatitis C genotype 4. J Hepatol. 2015;63:581-5.
PubMed Abstract»Durham DP, Skrip LA, Bruce RD, et al. The Impact of Enhanced Screening and Treatment on Hepatitis C in the United States. Clin Infect Dis. 2015;62:298-304.
PubMed Abstract»El Kassas M, Elbaz T, Abd El Latif Y, Esmat G. Elbasvir and grazoprevir for chronic hepatitis C genotypes 1 and 4. Expert Rev Clin Pharmacol. 2016;9:1413-21.
PubMed Abstract»Eletreby R, Elakel W, El Raziky M, Esmat G. Response to Real life Egyptian experience of efficacy / safety of Simeprevir\ Sofosbuvir in HCV genotype IV. Liver Int. 2017;37:766.
PubMed Abstract»Eletreby R, Elakel W, Said M, et al. Real life Egyptian experience of efficacy and safety of Simeprevir/Sofosbuvir therapy in 6211 chronic HCV genotype IV infected patients. Liver Int. 2017;37:534-541.
PubMed Abstract»Elsharkawy A, Eletreby R, Fouad R, et al. Impact of different sofosbuvir based treatment regimens on the biochemical profile of chronic hepatitis C genotype 4 patients. Expert Rev Gastroenterol Hepatol. 2017;11:773-8.
PubMed Abstract»Elsharkawy A, Fouad R, El Akel W, et al. Sofosbuvir-based treatment regimens: real life results of 14 409 chronic HCV genotype 4 patients in Egypt. Aliment Pharmacol Ther. 2017;45:681-687.
PubMed Abstract»Esmat G, El Raziky M, El Kassas M, Hassany M, Gamil ME. The future for the treatment of genotype 4 chronic hepatitis C. Liver Int. 2012;32 Suppl 1:146-50.
PubMed Abstract»European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C: Final update of the series☆. J Hepatol. 2020:S0168-8278(20)30548-1.
EASL»Federman AD, Kil N, Kannry J, et al. An Electronic Health Record-based Intervention to Promote Hepatitis C Virus Testing Among Adults Born Between 1945 and 1965: A Cluster-randomized Trial. Med Care. 2017;55:590-7.
PubMed Abstract»Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599-607.
PubMed Abstract»Forns X, Lee SS, Valdes J, et al. Glecaprevir plus pibrentasvir for chronic hepatitis C virus genotype 1, 2, 4, 5, or 6 infection in adults with compensated cirrhosis (EXPEDITION-1): a single-arm, open-label, multicentre phase 3 trial. Lancet Infect Dis. 2017;17:1062-1068.
PubMed Abstract»Hézode C, Asselah T, Reddy KR, et al. Ombitasvir plus paritaprevir plus ritonavir with or without ribavirin in treatment-naive and treatment-experienced patients with genotype 4 chronic hepatitis C virus infection (PEARL-I): a randomised, open-label trial. Lancet. 2015;385:2502-9.
PubMed Abstract»Hézode C, Hirschfield GM, Ghesquiere W, et al. Daclatasvir plus peginterferon alfa and ribavirin for treatment-naive chronic hepatitis C genotype 1 or 4 infection: a randomised study. Gut. 2014;64:948-56.
PubMed Abstract»Jacobson IM, Lawitz E, Gane EJ, et al. Efficacy of 8 Weeks of Sofosbuvir, Velpatasvir, and Voxilaprevir in Patients With Chronic HCV Infection: 2 Phase 3 Randomized Trials. Gastroenterology. 2017;153:113-22.
PubMed Abstract»Kamal SM. Hepatitis C genotype 4 therapy: increasing options and improving outcomes. Liver Int. 2009;29 Suppl 1:39-48.
PubMed Abstract»Kamal SM. Hepatitis C virus genotype 4 therapy: progress and challenges. Liver Int. 2011;31 Suppl 1:45-52.
PubMed Abstract»Kohli A, Kapoor R, Sims Z, et al. Ledipasvir and sofosbuvir for hepatitis C genotype 4: a proof-of-concept, single-centre, open-label phase 2a cohort study. Lancet Infect Dis. 2015;15:1049-54.
PubMed Abstract»Konerman MA, Thomson M, Gray K, et al. Impact of an electronic health record alert in primary care on increasing hepatitis c screening and curative treatment for baby boomers. Hepatology. 2017;66:1805-1813.
PubMed Abstract»Kruger DL, Rein DB, Kil N, et al. Implementation of Birth-Cohort Testing for Hepatitis C Virus. Health Promot Pract. 2017;18:283-289.
PubMed Abstract»Kwo PY, Poordad F, Asatryan A, et al. Glecaprevir and pibrentasvir yield high response rates in patients with HCV genotype 1-6 without cirrhosis. J Hepatol. 2017;67:263-271.
PubMed Abstract»Lawitz E, Mangia A, Wyles D, et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med. 2013;368:1878-87.
PubMed Abstract»Lenz O, Vijgen L, Berke JM, et al. Virologic response and characterisation of HCV genotype 2-6 in patients receiving TMC435 monotherapy (study TMC435-C202). J Hepatol. 2013;58:445-51.
PubMed Abstract»Mahajan R, Liu SJ, Klevens RM, Holmberg SD. Indications for testing among reported cases of HCV infection from enhanced hepatitis surveillance sites in the United States, 2004-2010. Am J Public Health. 2013;103:1445-9.
PubMed Abstract»Moreno C, Hezode C, Marcellin P, et al. Efficacy and safety of simeprevir with PegIFN/ribavirin in naïve or experienced patients infected with chronic HCV genotype 4. J Hepatol. 2015;62:1047-55.
PubMed Abstract»Panagiotakopoulos L, Sandul AL, Conners EE, Foster MA, Nelson NP, Wester C. CDC Recommendations for Hepatitis C Testing Among Perinatally Exposed Infants and Children - United States, 2023. MMWR Recomm Rep. 2023;72:1-21.
PubMed Abstract»Rossignol JF, Elfert A, El-Gohary Y, Keeffe EB. Improved virologic response in chronic hepatitis C genotype 4 treated with nitazoxanide, peginterferon, and ribavirin. Gastroenterology. 2009;136:856-62.
PubMed Abstract»Ruane PJ, Ain D, Stryker R, et al. Sofosbuvir plus ribavirin for the treatment of chronic genotype 4 hepatitis C virus infection in patients of Egyptian ancestry. J Hepatol. 2015;62:1040-6.
PubMed Abstract»Ryerson AB, Schillie S, Barker LK, Kupronis BA, Wester C. Vital Signs: Newly Reported Acute and Chronic Hepatitis C Cases - United States, 2009-2018. MMWR Morb Mortal Wkly Rep. 2020;69:399-404.
PubMed Abstract»Shiha G, Esmat G, Hassany M, et al. Ledipasvir/sofosbuvir with or without ribavirin for 8 or 12 weeks for the treatment of HCV genotype 4 infection: results from a randomised phase III study in Egypt. Gut. 2019;68:721-8.
PubMed Abstract»Smith BD, Beckett GA, Yartel A, Holtzman D, Patel N, Ward JW. Previous exposure to HCV among persons born during 1945-1965: prevalence and predictors, United States, 1999-2008. Am J Public Health. 2014;104:474-81.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012;61:1-32.
PubMed Abstract»Trapero-Marugan M, Moreno-Monteagudo JA, Garcia-Buey L, Borque MJ, Medina J, Garcia-Sanchez A, Moreno-Otero R. Clinical and pathological characteristics and response to combination therapy of genotype 4 chronic hepatitis C patients: experience from a spanish center. J Chemother. 2007;19:423-7.
PubMed Abstract»Waked I, Esmat G, Elsharkawy A, et al. Screening and Treatment Program to Eliminate Hepatitis C in Egypt. N Engl J Med. 2020;382:1166-74.
PubMed Abstract»Waked I, Shiha G, Qaqish RB, et al. Ombitasvir, paritaprevir, and ritonavir plus ribavirin for chronic hepatitis C virus genotype 4 infection in Egyptian patients with or without compensated cirrhosis (AGATE-II): a multicentre, phase 3, partly randomised open-label trial. Lancet Gastroenterol Hepatol. 2016;1:36-44.
PubMed Abstract»Yartel AK, Rein DB, Brown KA, et al. Hepatitis C virus testing for case identification in persons born during 1945-1965: Results from three randomized controlled trials. Hepatology. 2018;67:524-533.
PubMed Abstract»Zeuzem S, Ghalib R, Reddy KR, et al. Grazoprevir-Elbasvir Combination Therapy for Treatment-Naive Cirrhotic and Noncirrhotic Patients With Chronic Hepatitis C Virus Genotype 1, 4, or 6 Infection: A Randomized Trial. Ann Intern Med. 2015;163:1-13.
PubMed Abstract»Zibbell JE, Asher AK, Patel RC, et al. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am J Public Health. 2018;108:175-181.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»Lesson 3. Hepatitis C Diagnostic Testing
HCV Diagnostic Tests
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»Abdel-Hamid M, El-Daly M, El-Kafrawy S, Mikhail N, Strickland GT, Fix AD. Comparison of second- and third-generation enzyme immunoassays for detecting antibodies to hepatitis C virus. J Clin Microbiol. 2002;40:1656-9.
PubMed Abstract»Alter MJ, Kuhnert WL, Finelli L. Guidelines for laboratory testing and result reporting of antibody to hepatitis C virus. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2003;52:1-13, 15.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Testing for HCV infection: an update of guidance for clinicians and laboratorians. MMWR Morb Mortal Wkly Rep. 2013;62:362-5.
PubMed Abstract»Cloherty G, Talal A, Coller K, et al. Role of Serologic and Molecular Diagnostic Assays in Identification and Management of Hepatitis C Virus Infection. J Clin Microbiol. 2016;54:265-73.
PubMed Abstract»Colin C, Lanoir D, Touzet S, Meyaud-Kraemer L, Bailly F, Trepo C. Sensitivity and specificity of third-generation hepatitis C virus antibody detection assays: an analysis of the literature. J Viral Hepat. 2001;8:87-95.
PubMed Abstract»Dufour DR, Talastas M, Fernandez MD, Harris B. Chemiluminescence assay improves specificity of hepatitis C antibody detection. Clin Chem. 2003;49:940-4.
PubMed Abstract»Freiman JM, Tran TM, Schumacher SG, et al. Hepatitis C Core Antigen Testing for Diagnosis of Hepatitis C Virus Infection: A Systematic Review and Meta-analysis. Ann Intern Med. 2016;165:345-55.
PubMed Abstract»Glynn SA, Wright DJ, Kleinman SH, et al. Dynamics of viremia in early hepatitis C virus infection. Transfusion. 2005;45:994-1002.
PubMed Abstract»Gretch DR. Diagnostic tests for hepatitis C. Hepatology. 1997;26(3 Suppl 1):43S-47S.
PubMed Abstract»Gretch DR. Use and interpretation of HCV diagnostic tests in the clinical setting. Clin Liver Dis. 1997;1:543-57.
PubMed Abstract»Hullegie SJ, GeurtsvanKessel CH, van der Eijk AA, Ramakers C, Rijnders BJA. HCV antigen instead of RNA testing to diagnose acute HCV in patients treated in the Dutch Acute HCV in HIV Study. J Int AIDS Soc. 2017;20:21621.
PubMed Abstract»Jewett A, Smith BD, Garfein RS, Cuevas-Mota J, Teshale EH, Weinbaum CM. Field-based performance of three pre-market rapid hepatitis C virus antibody assays in STAHR (Study to Assess Hepatitis C Risk) among young adults who inject drugs in San Diego, CA. J Clin Virol. 2012;54:213-7.
PubMed Abstract»Kamili S, Drobeniuc J, Araujo AC, Hayden TM. Laboratory diagnostics for hepatitis C virus infection. Clin Infect Dis. 2012;55 Suppl 1:S43-8.
PubMed Abstract»Kao JH, Lai MY, Hwang YT, et al. Chronic hepatitis C without anti-hepatitis C antibodies by second-generation assay. A clinicopathologic study and demonstration of the usefulness of a third-generation assay. Dig Dis Sci. 1996;41:161-5.
PubMed Abstract»Khan H, Hill A, Main J, Brown A, Cooke G. Can Hepatitis C Virus Antigen Testing Replace Ribonucleic Acid Polymearse Chain Reaction Analysis for Detecting Hepatitis C Virus? A Systematic Review. Open Forum Infect Dis. 2017;4:ofw252.
PubMed Abstract»Laperche S, Nübling CM, Stramer SL, et al. Sensitivity of hepatitis C virus core antigen and antibody combination assays in a global panel of window period samples. Transfusion. 2015;55:2489-98.
PubMed Abstract»Lee SR, Kardos KW, Schiff E, et al. Evaluation of a new, rapid test for detecting HCV infection, suitable for use with blood or oral fluid. J Virol Methods. 2011;172:27-31.
PubMed Abstract»Lee SR, Yearwood GD, Guillon GB, et al. Evaluation of a rapid, point-of-care test device for the diagnosis of hepatitis C infection. J Clin Virol. 2010;48:15-7.
PubMed Abstract»Majid AM, Gretch DR. Current and future hepatitis C virus diagnostic testing: problems and advancements. Microbes Infect. 2002;4:1227-36.
PubMed Abstract»Pawlotsky JM. Use and interpretation of hepatitis C virus diagnostic assays. Clin Liver Dis. 2003;7:127-37.
PubMed Abstract»Peeling RW, Boeras DI, Marinucci F, Easterbrook P. The future of viral hepatitis testing: innovations in testing technologies and approaches. BMC Infect Dis. 2017;17:699.
PubMed Abstract»Richter SS. Laboratory assays for diagnosis and management of hepatitis C virus infection. J Clin Microbiol. 2002;40:4407-12.
PubMed Abstract»Scott JD, Gretch DR. Molecular diagnostics of hepatitis C virus infection: a systematic review. JAMA. 2007;297:724-32.
PubMed Abstract»Shivkumar S, Peeling R, Jafari Y, Joseph L, Pant Pai N. Accuracy of rapid and point-of-care screening tests for hepatitis C: a systematic review and meta-analysis. Ann Intern Med. 2012;157:558-66.
PubMed Abstract»Smith BD, Drobeniuc J, Jewett A, et al. Evaluation of three rapid screening assays for detection of antibodies to hepatitis C virus. J Infect Dis. 2011;204:825-31.
PubMed Abstract»Smith BD, Teshale E, Jewett A, et al. Performance of premarket rapid hepatitis C virus antibody assays in 4 national human immunodeficiency virus behavioral surveillance system sites. Clin Infect Dis. 2011;53:780-6.
PubMed Abstract»U.S. Food and Drug Administration. FDA Permits Marketing of First Point-of-Care Hepatitis C RNA Test. June 27,2024
U.S. Food and Drug Administration.»HCV Testing Sequence
Alter MJ, Kuhnert WL, Finelli L. Guidelines for laboratory testing and result reporting of antibody to hepatitis C virus. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2003;52:1-13, 15.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Testing for HCV infection: an update of guidance for clinicians and laboratorians. MMWR Morb Mortal Wkly Rep. 2013;62:362-5.
PubMed Abstract»Centers for Disease Control and Prevention. Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. Centers for Disease Control and Prevention. MMWR Recomm Rep. 1998;47(RR-19):1-39.
CDC and MMWR»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012;61:1-32.
PubMed Abstract»Ward JW, Lok AS, Thomas DL, El-Serag HB, Kim WR. Report on a single-topic conference on "Chronic viral hepatitis--strategies to improve effectiveness of screening and treatment". Hepatology. 2012;55:307-15.
PubMed Abstract»Interpreting and Communicating Test Results
Bate JP, Colman AJ, Frost PJ, Shaw DR, Harley HA. High prevalence of late relapse and reinfection in prisoners treated for chronic hepatitis C. J Gastroenterol Hepatol. 2010;25:1276-80.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Testing for HCV infection: an update of guidance for clinicians and laboratorians. MMWR Morb Mortal Wkly Rep. 2013;62:362-5.
PubMed Abstract»Falade-Nwulia O, Sulkowski MS, Merkow A, Latkin C, Mehta SH. Understanding and addressing hepatitis C reinfection in the oral direct-acting antiviral era. J Viral Hepat. 2018;25:220-227.
PubMed Abstract»Sarrazin C, Isakov V, Svarovskaia ES, et al. Late Relapse Versus Hepatitis C Virus Reinfection in Patients With Sustained Virologic Response After Sofosbuvir-Based Therapies. Clin Infect Dis. 2017;64:44-52.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012;61:1-32.
PubMed Abstract»Linkage to Care
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, managing, and treating hepatitis C.
AASLD-IDSA Hepatitis C Guidance»Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364:2199-207.
PubMed Abstract»Gardner LI, Metsch LR, Anderson-Mahoney P, et al. Efficacy of a brief case management intervention to link recently diagnosed HIV-infected persons to care. AIDS. 2005;19:423-31.
PubMed Abstract»Guss D, Sherigar J, Rosen P, Mohanty SR. Diagnosis and Management of Hepatitis C Infection in Primary Care Settings. J Gen Intern Med. 2018;33:551-7.
PubMed Abstract»Holmberg SD, Spradling PR, Moorman AC, Denniston MM. Hepatitis C in the United States. N Engl J Med. 2013;368:1859-61.
PubMed Abstract»Horstmann E, Brown J, Islam F, Buck J, Agins BD. Retaining HIV-infected patients in care: where are we? Where do we go from here? Clin Infect Dis 2010;50:752–61.
PubMed Abstract»Kattakuzhy S, Gross C, Emmanuel B, et al. Expansion of Treatment for Hepatitis C Virus Infection by Task Shifting to Community-Based Nonspecialist Providers: A Nonrandomized Clinical Trial. Ann Intern Med. 2017;167:311-318.
PubMed Abstract»Mayer KH. Introduction: linkage, engagement, and retention in HIV care—essential for optimal individual- and community-level outcomes in the era of highly active antiretroviral therapy. Clin Infect Dis 2011;
52(Suppl 2):S205–7.
PubMed Abstract»Ngo BV, James JR, Blalock KL, Jackson SL, Chew LD, Tsui JI. Hepatitis C treatment outcomes among patients treated in co-located primary care and addiction treatment settings. J Subst Abuse Treat. 2021;131:108438.
PubMed Abstract»Oru E, Trickey A, Shirali R, Kanters S, Easterbrook P. Decentralisation, integration, and task-shifting in hepatitis C virus infection testing and treatment: a global systematic review and meta-analysis. Lancet Glob Health. 2021;9:e431-e445.
PubMed Abstract»Ramirez G, Cabral R, Patterson M, et al. Early Identification and Linkage to Care for People with Chronic HBV and HCV Infection: The HepTLC Initiative. Public Health Rep. 2016;131 Suppl 2:5-11.
PubMed Abstract»Rhea S, Seña AC, Hilton A, Hurt CB, Wohl D, Fleischauer A. Integrated Hepatitis C Testing and Linkage to Care at a Local Health Department Sexually Transmitted Disease Clinic: Determining Essential Resources and Evaluating Outcomes. Sex Transm Dis. 2018;45:229-232.
PubMed Abstract»Seña AC, Willis SJ, Hilton A, et al. Efforts at the Frontlines: Implementing a Hepatitis C Testing and Linkage-to-Care Program at the Local Public Health Level. Public Health Rep. 2016;131 Suppl 2:57-64.
PubMed Abstract»Shehab TM, Sonnad SS, Lok AS. Management of hepatitis C patients by primary care physicians in the USA: results of a national survey. J Viral Hepat. 2001;8:377-83.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012;61:1-32.
PubMed Abstract»Tohme RA, Xing J, Liao Y, Holmberg SD. Hepatitis C testing, infection, and linkage to care among racial and ethnic minorities in the United States, 2009-2010. Am J Public Health. 2013;103:112-9.
PubMed Abstract»World Health Organization. Updated recommendations on simplified service delivery and diagnostics for hepatitis C infection. Policy Brief. Geneva: World Health Organization; 2022.
WHO»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»Butt AA, Yan P, Shaikh OS, Chung RT, Sherman KE. Treatment adherence and virological response rates in hepatitis C virus infected persons treated with sofosbuvir-based regimens: results from ERCHIVES. Liver Int. 2016;36:1275-83.
PubMed Abstract»Chevaliez S, Rodriguez C, Pawlotsky JM. New virologic tools for management of chronic hepatitis B and C. Gastroenterology. 2012;142:1303-1313.e1.
PubMed Abstract»Chevaliez S, Soulier A, Poiteau L, Bouvier-Alias M, Pawlotsky JM. Clinical utility of hepatitis C virus core antigen quantification in patients with chronic hepatitis C. J Clin Virol. 2014;61:145-8.
PubMed Abstract»Dawson GJ. The potential role of HCV core antigen testing in diagnosing HCV infection. Antivir Ther. 2012;17:1431-5.
PubMed Abstract»Gordon SC, Yoshida EM, Lawitz EJ, et al. Adherence to assigned dosing regimen and sustained virological response among chronic hepatitis C genotype 1 patients treated with boceprevir plus peginterferon alfa-2b/ribavirin. Aliment Pharmacol Ther. 2013;38:16-27.
PubMed Abstract»Guss D, Sherigar J, Rosen P, Mohanty SR. Diagnosis and Management of Hepatitis C Infection in Primary Care Settings. J Gen Intern Med. 2018;33:551-7.
PubMed Abstract»Litwin AH , Agyemang L, Akiyama M, Norton B, Ning Y, Heo M, Umanski G, Arnsten JH. The PREVAIL Study: Intensive models of HCV care for people who inject drugs. J Hepatol 2017; 66 [Supplement]:S72.
Journal of Hepatology»Lo Re V, 3rd, Amorosa VK, Localio AR, et al. Adherence to hepatitis C virus therapy and early virologic outcomes. Clin Infect Dis. 2009;48:186-93.
PubMed Abstract»Lo Re V, 3rd, Teal V, Localio AR, Amorosa VK, Kaplan DE, Gross R. Adherence to hepatitis C virus therapy in HIV/hepatitis C-coinfected patients. AIDS Behav. 2013;17:94-103.
PubMed Abstract»Lo Re V, 3rd, Teal V, Localio AR, Amorosa VK, Kaplan DE, Gross R. Relationship between adherence to hepatitis C virus therapy and virologic outcomes: a cohort study. Ann Intern Med. 2011;155:353-60.
PubMed Abstract»Lok AS, Sulkowski MS, Kort JJ, et al. Efficacy of Glecaprevir and Pibrentasvir in Patients With Genotype 1 Hepatitis C Virus Infection With Treatment Failure After NS5A Inhibitor Plus Sofosbuvir Therapy. Gastroenterology. 2019;157:1506-17.
PubMed Abstract»Manns MP, Buti M, Gane E, et al. Hepatitis C virus infection. Nat Rev Dis Primers. 2017;3:17006.
PubMed Abstract»Martinello M, Hajarizadeh B, Grebely J, Dore GJ, Matthews GV. HCV Cure and Reinfection Among People With HIV/HCV Coinfection and People Who Inject Drugs. Curr HIV/AIDS Rep. 2017;14:110-121.
PubMed Abstract»McHutchison JG, Manns M, Patel K, et al. Adherence to combination therapy enhances sustained response in genotype-1-infected patients with chronic hepatitis C. Gastroenterology. 2002;123:1061-9.
PubMed Abstract»Ottiger C, Gygli N, Huber AR. Detection limit of architect hepatitis C core antigen assay in correlation with HCV RNA, and renewed confirmation algorithm for reactive anti-HCV samples. J Clin Virol. 2013;58:535-40.
PubMed Abstract»Panagiotakopoulos L, Sandul AL, Conners EE, Foster MA, Nelson NP, Wester C. CDC Recommendations for Hepatitis C Testing Among Perinatally Exposed Infants and Children - United States, 2023. MMWR Recomm Rep. 2023;72:1-21.
PubMed Abstract»Petersen T, Townsend K, Gordon LA, et al. High adherence to all-oral directly acting antiviral HCV therapy among an inner-city patient population in a phase 2a study. Hepatol Int. 2016;10:310-9.
PubMed Abstract»Raptopoulou M, Tsantoulas D, Vafiadi I, et al. The effect of adherence to therapy on sustained response in daily or three times a week interferon alpha-2b plus ribavirin treatment of naive and nonresponder chronic hepatitis C patients. J Viral Hepat. 2005;12:91-5.
PubMed Abstract»Reddy KR, Shiffman ML, Morgan TR, et al. Impact of ribavirin dose reductions in hepatitis C virus genotype 1 patients completing peginterferon alfa-2a/ribavirin treatment. Clin Gastroenterol Hepatol. 2007;5:124-9.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Shiffman ML, Di Bisceglie AM, Lindsay KL, et al. Peginterferon alfa-2a and ribavirin in patients with chronic hepatitis C who have failed prior treatment. Gastroenterology. 2004;126:1015-23.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012;61:1-32.
PubMed Abstract»Tillmann HL. Hepatitis C virus core antigen testing: role in diagnosis, disease monitoring and treatment. World J Gastroenterol. 2014;20:6701-6.
PubMed Abstract»Weber NC, Klepser ME, Akers JM, Klepser DG, Adams AJ. Use of CLIA-waived point-of-care tests for infectious diseases in community pharmacies in the United States. Expert Rev Mol Diagn. 2016;16:253-64.
PubMed Abstract»Lesson 4. Counseling for Prevention of HCV Transmission
Sexual Transmission of HCV
Bradshaw D1, Matthews G, Danta M. Sexually transmitted hepatitis C infection: the new epidemic in MSM? Curr Opin Infect Dis. 2013;26:66-72.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Sexual transmission of hepatitis C virus among HIV-infected men who have sex with men--New York City, 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60:945-50.
PubMed Abstract»Gorgos L. Sexual transmission of viral hepatitis. Infect Dis Clin North Am. 2013;27:811-36.
PubMed Abstract»Hoornenborg E, Achterbergh RCA, Schim van der Loeff MF, et al. MSM starting preexposure prophylaxis are at risk of hepatitis C virus infection. AIDS. 2017;31:1603-1610.
PubMed Abstract»Ingiliz P, Martin TC, Rodger A, et al. HCV reinfection incidence and spontaneous clearance rates in HIV-positive men who have sex with men in Western Europe. J Hepatol. 2017;66:282-287.
PubMed Abstract»Jin F, Dore GJ, Matthews G, et al. Prevalence and incidence of hepatitis C virus infection in men who have sex with men: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:39-56.
PubMed Abstract»Jin F, Matthews GV, Grulich AE. Sexual transmission of hepatitis C virus among gay and bisexual men: a systematic review. Sex Health. 2017;14:28-41.
PubMed Abstract»Kao JH, Liu CJ, Chen PJ, Chen W, Lai MY, Chen DS. Low incidence of hepatitis C virus transmission between spouses: a prospective study. J Gastroenterol Hepatol. 2000;15:391-5.
PubMed Abstract»Martin TC, Martin NK, Hickman M, et al. Hepatitis C virus reinfection incidence and treatment outcome among HIV-positive MSM. AIDS. 2013;27:2551-7.
PubMed Abstract»Newsum AM, Matser A, Schinkel J, et al. Incidence of HCV reinfection among HIV-positive MSM and its association with sexual risk behavior: a longitudinal analysis. Clin Infect Dis. 2020 May 27. Online ahead of print.
PubMed Abstract»Ramière C, Charre C, Miailhes P, et al. Patterns of Hepatitis C Virus Transmission in Human Immunodeficiency Virus (HIV)-infected and HIV-negative Men Who Have Sex With Men. Clin Infect Dis. 2019;69:2127-35.
PubMed Abstract»Recommendations for the prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. Centers for Disease Control. MMWR Recomm Rep. 1998;47(RR-19):1-39.
CDC and MMWR»Tahan V, Karaca C, Yildirim B, et al. Sexual transmission of HCV between spouses. Am J Gastroenterol. 2005;100:821-4.
PubMed Abstract»Terrault NA, Dodge JL, Murphy EL, Tavis JE, Kiss A, Levin TR, Gish RG, Busch MP, Reingold AL, Alter MJ. Sexual transmission of hepatitis C virus among monogamous heterosexual couples: the HCV partners study. Hepatology. 2013;57:881-9.
PubMed Abstract»Terrault NA. Sexual activity as a risk factor for hepatitis C. Hepatology. 2002;36(5 Suppl 1):S99-105.
PubMed Abstract»Tohme RA, Holmberg SD. Is sexual contact a major mode of hepatitis C virus transmission? Hepatology. 2010;52:1497-505.
PubMed Abstract»Urbanus AT, Van De Laar TJ, Geskus R, et al. Trends in hepatitis C virus infections among MSM attending a sexually transmitted infection clinic; 1995-2010. AIDS. 2014;28:781-90.
PubMed Abstract»van de Laar TJ, Matthews GV, Prins M, Danta M. Acute hepatitis C in HIV-infected men who have sex with men: an emerging sexually transmitted infection. AIDS. 2010;24:1799-812.
PubMed Abstract»van der Helm JJ, Prins M, del Amo J, et al. The hepatitis C epidemic among HIV-positive MSM: incidence estimates from 1990 to 2007. AIDS. 2011;25:1083-91.
PubMed Abstract»Vandelli C, Renzo F, Romanò L, et al. Lack of evidence of sexual transmission of hepatitis C among monogamous couples: results of a 10-year prospective follow-up study. Am J Gastroenterol. 2004;99:855-9.
PubMed Abstract»Wandeler G, Gsponer T, Bregenzer A, et al. Hepatitis C virus infections in the Swiss HIV Cohort Study: a rapidly evolving epidemic. Clin Infect Dis. 2012;55:1408-16.
PubMed Abstract»Young J, Rossi C, Gill J, et al. Risk Factors for Hepatitis C Virus Reinfection After Sustained Virologic Response in Patients Coinfected With HIV. Clin Infect Dis. 2017;64:1154-1162.
PubMed Abstract»Injection Drug Use and HCV Transmission
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Key populations: identification and management of HCV in people who inject drugs.
AASLD/IDSA Hepatitis C Guidance»Alter MJ. Prevention of spread of hepatitis C. Hepatology. 2002;36(5 Suppl 1):S93-8.
PubMed Abstract»Amon JJ, Garfein RS, Ahdieh-Grant L, et al. Prevalence of hepatitis C virus infection among injection drug users in the United States, 1994-2004. Clin Infect Dis. 2008;46:1852-8.
PubMed Abstract»Binka M, Paintsil E, Patel A, Lindenbach BD, Heimer R. Survival of Hepatitis C Virus in Syringes Is Dependent on the Design of the Syringe-Needle and Dead Space Volume. PLoS One. 2015;10:e0139737.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). 2019 Viral Hepatitis Surveillance Report—Hepatitis C. Published May 2021.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Centers for Disease Control and Prevention (CDC). Viral Hepatitis Statistics and Surveillance—United States, 2016.
CDC Viral Hepatitis Surveillance»Corcorran MA, Tsui JI, Scott JD, Dombrowski JC, Glick SN. Age and gender-specific hepatitis C continuum of care and predictors of direct acting antiviral treatment among persons who inject drugs in Seattle, Washington. Drug Alcohol Depend. 2021;220:108525.
PubMed Abstract»Doerrbecker J, Friesland M, Ciesek S, et al. Inactivation and survival of hepatitis C virus on inanimate surfaces. J Infect Dis. 2011;204:1830-8.
PubMed Abstract»Falade-Nwulia O, Sulkowski MS, Merkow A, Latkin C, Mehta SH. Understanding and addressing hepatitis C reinfection in the oral direct-acting antiviral era. J Viral Hepat. 2018;25:220-227.
PubMed Abstract»Grady BP, Schinkel J, Thomas XV, Dalgard O. Hepatitis C virus reinfection following treatment among people who use drugs. Clin Infect Dis. 2013;57 Suppl 2:S105-10.
PubMed Abstract»Hagan H, Pouget ER, Des Jarlais DC, Lelutiu-Weinberger C. Meta-regression of hepatitis C virus infection in relation to time since onset of illicit drug injection: the influence of time and place. Am J Epidemiol. 2008;168:1099-109.
PubMed Abstract»Hagan H, Pouget ER, Des Jarlais DC. A systematic review and meta-analysis of interventions to prevent hepatitis C virus infection in people who inject drugs. J Infect Dis. 2011;204:74-83.
PubMed Abstract»Hagan H, Pouget ER, Williams IT, et al. Attribution of hepatitis C virus seroconversion risk in young injection drug users in 5 US cities. J Infect Dis. 2010;201:378-85.
PubMed Abstract»Hahn JA, Page-Shafer K, Lum PJ, et al. Hepatitis C virus seroconversion among young injection drug users: relationships and risks. J Infect Dis. 2002;186:1558-64.
PubMed Abstract»Hajarizadeh B, Cunningham EB, Valerio H, et al. Hepatitis C reinfection after successful antiviral treatment among people who inject drugs: A meta-analysis. J Hepatol. 2020;72:643-57.
PubMed Abstract»Martinello M, Hajarizadeh B, Grebely J, Dore GJ, Matthews GV. HCV Cure and Reinfection Among People With HIV/HCV Coinfection and People Who Inject Drugs. Curr HIV/AIDS Rep. 2017;14:110-121.
PubMed Abstract»Muller A, Vlahov D, Akiyama MJ, Kurth A. Hepatitis C Reinfection in People Who Inject Drugs in Resource-Limited Countries: A Systematic Review and Analysis. Int J Environ Res Public Health. 2020;17:4951.
PubMed Abstract»Nelson PK, Mathers BM, Cowie B, et al. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews. Lancet. 2011;378:571-83.
PubMed Abstract»Nolan S, Dias Lima V, Fairbairn N, et al. The impact of methadone maintenance therapy on hepatitis C incidence among illicit drug users. Addiction. 2014;109:2053-9.
PubMed Abstract»Ozga JE, Syvertsen JL, Pollini RA. Hepatitis C antibody prevalence, correlates and barriers to care among people who inject drugs in Central California. J Viral Hepat. 2022;29:518-28.
PubMed Abstract»Page K, Hahn JA, Evans J, et al. Acute hepatitis C virus infection in young adult injection drug users: a prospective study of incident infection, resolution, and reinfection. J Infect Dis. 2009;200:1216-26.
PubMed Abstract»Paintsil E, Binka M, Patel A, Lindenbach BD, Heimer R. Hepatitis C virus maintains infectivity for weeks after drying on inanimate surfaces at room temperature: implications for risks of transmission. J Infect Dis. 2014;209:1205-11.
PubMed Abstract»Paintsil E, He H, Peters C, Lindenbach BD, Heimer R. Survival of hepatitis C virus in syringes: implication for transmission among injection drug users. J Infect Dis. 2010;202:984-90.
PubMed Abstract»Platt L, Minozzi S, Reed J, et al. Needle syringe programmes and opioid substitution therapy for preventing hepatitis C transmission in people who inject drugs. Cochrane Database Syst Rev. 2017;9:CD012021.
PubMed Abstract»Recommendations for the prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. Centers for Disease Control. MMWR Recomm Rep. 1998;47(RR-19):1-39.
CDC and MMWR»Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of Late Relapse or Reinfection With Hepatitis C Virus After Achieving a Sustained Virological Response: A Systematic Review and Meta-analysis. Clin Infect Dis. 2016;62:683-94.
PubMed Abstract»Song H, Li J, Shi S, Yan L, Zhuang H, Li K. Thermal stability and inactivation of hepatitis C virus grown in cell culture. Virol J. 2010;7:40.
PubMed Abstract»Suryaprasad AG, White JZ, Xu F, et al. Emerging epidemic of hepatitis C virus infections among young nonurban persons who inject drugs in the United States, 2006-2012. Clin Infect Dis. 2014;59:1411-9.
PubMed Abstract»Tsui JI, Evans JL, Lum PJ, Hahn JA, Page K. Association of opioid agonist therapy with lower incidence of hepatitis C virus infection in young adult injection drug users. JAMA Intern Med. 2014;174:1974-81.
PubMed Abstract»Turner KM, Hutchinson S, Vickerman P, et al. The impact of needle and syringe provision and opiate substitution therapy on the incidence of hepatitis C virus in injecting drug users: pooling of UK evidence. Addiction. 2011;106:1978-88.
PubMed Abstract»Zibbell JE, Asher AK, Patel RC, et al. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am J Public Health. 2018;108:175-181.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»Zule WA, Pande PG, Otiashvili D, et al. Options for reducing HIV transmission related to the dead space in needles and syringes. Harm Reduct J. 2018;15:3.
PubMed Abstract»Household HCV Transmission
Ackerman Z, Ackerman E, Paltiel O. Intrafamilial transmission of hepatitis C virus: a systematic review. J Viral Hepat. 2000;7:93-103.
PubMed Abstract»Alter MJ. Prevention of spread of hepatitis C. Hepatology. 2002;36(5 Suppl 1):S93-8.
PubMed Abstract»Brackmann SA, Gerritzen A, Oldenburg J, Brackmann HH, Schneweis KE. Search for intrafamilial transmission of hepatitis C virus in hemophilia patients. Blood. 1993;81:1077-82.
PubMed Abstract»Diago M, Zapater R, Tuset C, et al. Intrafamily transmission of hepatitis C virus: sexual and non-sexual contacts. J Hepatol. 1996;25:125-8.
PubMed Abstract»Honda M, Kaneko S, Unoura M, Kobayashi K, Murakami S. Risk of hepatitis C virus infections through household contact with chronic carriers: analysis of nucleotide sequences. Hepatology. 1993;17:971-6.
PubMed Abstract»Indolfi G, Nesi A, Resti M. Intrafamilial transmission of hepatitis C virus. J Med Virol. 2013;85:608-14.
PubMed Abstract»Omar MZ, Metwally MA, El-Feky HM, Ahmed IA, Ismail MA, Idris A. Role of intrafamilial transmission in high prevalence of hepatitis C virus in Egypt. Hepat Med. 2017;9:27-33.
PubMed Abstract»Recommendations for the prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. Centers for Disease Control. MMWR Recomm Rep. 1998;47(RR-19):1-39.
CDC and MMWR»Perinatal HCV Transmission
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: HCV in pregnancy
AASLD/IDSA Hepatitis C Guidance»Ades AE, Gordon F, Scott K, et al. Overall Vertical Transmission of Hepatitis C Virus, Transmission Net of Clearance, and Timing of Transmission. Clin Infect Dis. 2023;76:905-12.
PubMed Abstract»Benova L, Mohamoud YA, Calvert C, Abu-Raddad LJ. Vertical transmission of hepatitis C virus: systematic review and meta-analysis. Clin Infect Dis. 2014;59:765-73.
PubMed Abstract»Ceci O, Margiotta M, Marello F, et al. Vertical transmission of hepatitis C virus in a cohort of 2,447 HIV-seronegative pregnant women: a 24-month prospective study. J Pediatr Gastroenterol Nutr. 2001;33:570-5.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). National Notifiable Diseases Surveillance System (NNDSS). Hepatitis C, Perinatal Infection: 2018 Case Definition.
CDC and NNDSS»Centers for Disease Control and Prevention (CDC). Sexual transmission of hepatitis C virus among HIV-infected men who have sex with men--New York City, 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60:945-50.
PubMed Abstract»Cottrell EB, Chou R, Wasson N, Rahman B, Guise JM. Reducing risk for mother-to-infant transmission of hepatitis C virus: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;158:109-13.
PubMed Abstract»European Paediatric Hepatitis C Virus Network. A significant sex--but not elective cesarean section--effect on mother-to-child transmission of hepatitis C virus infection. J Infect Dis. 2005;192:1872-9.
PubMed Abstract»Ghany MG, Strader DB, Thomas DL, Seeff LB; American Association for the Study of Liver Diseases. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335-74.
AASLD Practice Guidelines»Hashem M, Jhaveri R, Saleh DA, et al. Spontaneous Viral Load Decline and Subsequent Clearance of Chronic Hepatitis C Virus in Postpartum Women Correlates With Favorable Interleukin-28B Gene Allele. Clin Infect Dis. 2017;65:999-1005.
PubMed Abstract»Hattori Y, Orito E, Ohno T, et al. Loss of hepatitis C virus RNA after parturition in female patients with chronic HCV infection. J Med Virol. 2003;71:205-11.
PubMed Abstract»Indolfi G, Resti M. Perinatal transmission of hepatitis C virus infection. J Med Virol. 2009;81:836-43.
PubMed Abstract»Koneru A, Nelson N, Hariri S, et al. Increased Hepatitis C Virus (HCV) Detection in Women of Childbearing Age and Potential Risk for Vertical Transmission - United States and Kentucky, 2011-2014. MMWR Morb Mortal Wkly Rep. 2016;65:705-10.
PubMed Abstract»Lin HH, Kao JH. Hepatitis C virus load during pregnancy and puerperium. BJOG. 2000;107:1503-6.
PubMed Abstract»Mast EE, Hwang LY, Seto DS, Nolte FS, Nainan OV, Wurtzel H, Alter MJ. Risk factors for perinatal transmission of hepatitis C virus (HCV) and the natural history of HCV infection acquired in infancy. J Infect Dis. 2005;192:1880-9.
PubMed Abstract»Ohto H, Terazawa S, Sasaki N, et al. Transmission of hepatitis C virus from mothers to infants. The Vertical Transmission of Hepatitis C Virus Collaborative Study Group. N Engl J Med. 1994;330:744-50.
PubMed Abstract»Page CM, Hughes BL, Rhee EHJ, Kuller JA. Hepatitis C in Pregnancy: Review of Current Knowledge and Updated Recommendations for Management. Obstet Gynecol Surv. 2017;72:347-355.
PubMed Abstract»Panagiotakopoulos L, Sandul AL, Conners EE, Foster MA, Nelson NP, Wester C. CDC Recommendations for Hepatitis C Testing Among Perinatally Exposed Infants and Children - United States, 2023. MMWR Recomm Rep. 2023;72:1-21.
PubMed Abstract»Post JJ. Update on hepatitis C and implications for pregnancy. Obstet Med. 2017;10:157-160.
PubMed Abstract»Recommendations for the prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. Centers for Disease Control. MMWR Recomm Rep. 1998;47(RR-19):1-39.
CDC and MMWR»Resti M, Azzari C, Galli L, et al. Maternal drug use is a preeminent risk factor for mother-to-child hepatitis C virus transmission: results from a multicenter study of 1372 mother-infant pairs. J Infect Dis. 2002;185:567-72.
PubMed Abstract»Roberts EA, Yeung L. Maternal-infant transmission of hepatitis C virus infection. Hepatology. 2002;36:S106-13.
PubMed Abstract»Watts T, Stockman L, Martin J, Guilfoyle S, Vergeront JM. Increased Risk for Mother-to-Infant Transmission of Hepatitis C Virus Among Medicaid Recipients - Wisconsin, 2011-2015. MMWR Morb Mortal Wkly Rep. 2017;66:1136-1139.
PubMed Abstract»Yeung LT, King SM, Roberts EA. Mother-to-infant transmission of hepatitis C virus. Hepatology. 2001;34:223-9.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»Ackerman Z, Ackerman E, Paltiel O. Intrafamilial transmission of hepatitis C virus: a systematic review. J Viral Hepat. 2000;7:93-103.
PubMed Abstract»Benova L, Mohamoud YA, Calvert C, Abu-Raddad LJ. Vertical transmission of hepatitis C virus: systematic review and meta-analysis. Clin Infect Dis. 2014;59:765-73.
PubMed Abstract»Binka M, Paintsil E, Patel A, Lindenbach BD, Heimer R. Survival of Hepatitis C Virus in Syringes Is Dependent on the Design of the Syringe-Needle and Dead Space Volume. PLoS One. 2015;10:e0139737.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). 2019 Viral Hepatitis Surveillance Report—Hepatitis C. Published May 2021.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Centers for Disease Control and Prevention (CDC). National Notifiable Diseases Surveillance System (NNDSS). Hepatitis C, Perinatal Infection: 2018 Case Definition.
CDC and NNDSS»Centers for Disease Control and Prevention (CDC). Sexual transmission of hepatitis C virus among HIV-infected men who have sex with men--New York City, 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60:945-50.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Viral Hepatitis Statistics and Surveillance—United States, 2016.
CDC Viral Hepatitis Surveillance»Diago M, Zapater R, Tuset C, et al. Intrafamily transmission of hepatitis C virus: sexual and non-sexual contacts. J Hepatol. 1996;25:125-8.
PubMed Abstract»Falade-Nwulia O, Sulkowski MS, Merkow A, Latkin C, Mehta SH. Understanding and addressing hepatitis C reinfection in the oral direct-acting antiviral era. J Viral Hepat. 2018;25:220-227.
PubMed Abstract»Foster AL, Gaisa MM, Hijdra RM, et al. Shedding of Hepatitis C Virus Into the Rectum of HIV-infected Men Who Have Sex With Men. Clin Infect Dis. 2017;64:284-288.
PubMed Abstract»Gorgos L. Sexual transmission of viral hepatitis. Infect Dis Clin North Am. 2013;27:811-36.
PubMed Abstract»Hagan H, Pouget ER, Des Jarlais DC, Lelutiu-Weinberger C. Meta-regression of hepatitis C virus infection in relation to time since onset of illicit drug injection: the influence of time and place. Am J Epidemiol. 2008;168:1099-109.
PubMed Abstract»Hoornenborg E, Achterbergh RCA, Schim van der Loeff MF, et al. MSM starting preexposure prophylaxis are at risk of hepatitis C virus infection. AIDS. 2017;31:1603-1610.
PubMed Abstract»Jin F, Matthews GV, Grulich AE. Sexual transmission of hepatitis C virus among gay and bisexual men: a systematic review. Sex Health. 2017;14:28-41.
PubMed Abstract»Kao JH, Liu CJ, Chen PJ, Chen W, Lai MY, Chen DS. Low incidence of hepatitis C virus transmission between spouses: a prospective study. J Gastroenterol Hepatol. 2000;15:391-5.
PubMed Abstract»Kuncio DE, Newbern EC, Johnson CC, Viner KM. Failure to Test and Identify Perinatally Infected Children Born to Hepatitis C Virus-Infected Women. Clin Infect Dis. 2016;62:980-5.
PubMed Abstract»Lo Re V, 3rd, Teal V, Localio AR, Amorosa VK, Kaplan DE, Gross R. Adherence to hepatitis C virus therapy in HIV/hepatitis C-coinfected patients. AIDS Behav. 2013;17:94-103.
PubMed Abstract»Lo Re V, 3rd, Teal V, Localio AR, Amorosa VK, Kaplan DE, Gross R. Relationship between adherence to hepatitis C virus therapy and virologic outcomes: a cohort study. Ann Intern Med. 2011;155:353-60.
PubMed Abstract»Ly KN, Jiles RB, Teshale EH, Foster MA, Pesano RL, Holmberg SD. Hepatitis C Virus Infection Among Reproductive-Aged Women and Children in the United States, 2006 to 2014. Ann Intern Med. 2017;166:775-782.
PubMed Abstract»Martinello M, Hajarizadeh B, Grebely J, Dore GJ, Matthews GV. HCV Cure and Reinfection Among People With HIV/HCV Coinfection and People Who Inject Drugs. Curr HIV/AIDS Rep. 2017;14:110-121.
PubMed Abstract»Page CM, Hughes BL, Rhee EHJ, Kuller JA. Hepatitis C in Pregnancy: Review of Current Knowledge and Updated Recommendations for Management. Obstet Gynecol Surv. 2017;72:347-355.
PubMed Abstract»Paintsil E, Binka M, Patel A, Lindenbach BD, Heimer R. Hepatitis C virus maintains infectivity for weeks after drying on inanimate surfaces at room temperature: implications for risks of transmission. J Infect Dis. 2014;209:1205-11.
PubMed Abstract»Panagiotakopoulos L, Sandul AL, Conners EE, Foster MA, Nelson NP, Wester C. CDC Recommendations for Hepatitis C Testing Among Perinatally Exposed Infants and Children - United States, 2023. MMWR Recomm Rep. 2023;72:1-21.
PubMed Abstract»Pearlman B, Perrys M, Hinds A. Sofosbuvir/Velpatasvir/Voxilaprevir for Previous Treatment Failures With Glecaprevir/Pibrentasvir in Chronic Hepatitis C Infection. Am J Gastroenterol. 2019;114:1550-2.
PubMed Abstract»Petersen T, Townsend K, Gordon LA, et al. High adherence to all-oral directly acting antiviral HCV therapy among an inner-city patient population in a phase 2a study. Hepatol Int. 2016;10:310-9.
PubMed Abstract»Post JJ. Update on hepatitis C and implications for pregnancy. Obstet Med. 2017;10:157-160.
PubMed Abstract»Pufall EL, Kall M, Shahmanesh M, et al. Sexualized drug use ('chemsex') and high-risk sexual behaviours in HIV-positive men who have sex with men. HIV Med. 2018;19:261-270.
PubMed Abstract»Sarrazin C, Isakov V, Svarovskaia ES, et al. Late Relapse Versus Hepatitis C Virus Reinfection in Patients With Sustained Virologic Response After Sofosbuvir-Based Therapies. Clin Infect Dis. 2017;64:44-52.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Suryaprasad AG, White JZ, Xu F, et al. Emerging epidemic of hepatitis C virus infections among young nonurban persons who inject drugs in the United States, 2006-2012. Clin Infect Dis. 2014;59:1411-9.
PubMed Abstract»Tahan V, Karaca C, Yildirim B, et al. Sexual transmission of HCV between spouses. Am J Gastroenterol. 2005;100:821-4.
PubMed Abstract»Terrault NA, Dodge JL, Murphy EL, Tavis JE, Kiss A, Levin TR, Gish RG, Busch MP, Reingold AL, Alter MJ. Sexual transmission of hepatitis C virus among monogamous heterosexual couples: the HCV partners study. Hepatology. 2013;57:881-9.
PubMed Abstract»Terrault NA. Sexual activity as a risk factor for hepatitis C. Hepatology. 2002;36(5 Suppl 1):S99-105.
PubMed Abstract»Tohme RA, Holmberg SD. Is sexual contact a major mode of hepatitis C virus transmission? Hepatology. 2010;52:1497-505.
PubMed Abstract»Urbanus AT, Van De Laar TJ, Geskus R, et al. Trends in hepatitis C virus infections among MSM attending a sexually transmitted infection clinic; 1995-2010. AIDS. 2014;28:781-90.
PubMed Abstract»US Preventive Services Task Force, Owens DK, Davidson KW, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;323:970-5.
PubMed Abstract»Vandelli C, Renzo F, Romanò L, et al. Lack of evidence of sexual transmission of hepatitis C among monogamous couples: results of a 10-year prospective follow-up study. Am J Gastroenterol. 2004;99:855-9.
PubMed Abstract»Yaphe S, Bozinoff N, Kyle R, Shivkumar S, Pai NP, Klein M. Incidence of acute hepatitis C virus infection among men who have sex with men with and without HIV infection: a systematic review. Sex Transm Infect. 2012;88:558-64.
PubMed Abstract»Zibbell JE, Asher AK, Patel RC, et al. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am J Public Health. 2018;108:175-181.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»Lesson 5. Diagnosis of Acute HCV Infection
Definition of Acute HCV
Blackard JT, Shata MT, Shire NJ, Sherman KE. Acute hepatitis C virus infection: a chronic problem. Hepatology. 2008;47:321-31.
PubMed Abstract»Grebely J, Page K, Sacks-Davis R, et al. The effects of female sex, viral genotype, and IL28B genotype on spontaneous clearance of acute hepatitis C virus infection. Hepatology. 2014;59:109-20.
PubMed Abstract»Hajarizadeh B, Grebely J, Dore GJ. Case definitions for acute hepatitis C virus infection: A systematic review. J Hepatol. 2012;57:1349-60.
PubMed Abstract»Hofer H, Watkins-Riedel T, Janata O, et al. Spontaneous viral clearance in patients with acute hepatitis C can be predicted by repeated measurements of serum viral load. Hepatology. 2003;37:60-4.
PubMed Abstract»Kamal SM. Acute hepatitis C: a systematic review. Am J Gastroenterol. 2008;103:1283-97.
PubMed Abstract»McGovern BH, Birch CE, Bowen MJ, Reyor LL, Nagami EH, Chung RT, Kim AY. Improving the diagnosis of acute hepatitis C virus infection with expanded viral load criteria. Clin Infect Dis. 2009;49:1051-60.
PubMed Abstract»Clinical Features of Acute HCV
Barrera JM, Bruguera M, Ercilla MG, et al. Persistent hepatitis C viremia after acute self-limiting posttransfusion hepatitis C. Hepatology. 1995;21:639-44.
PubMed Abstract»Bulteel N, Partha Sarathy P, Forrest E, et al. Factors associated with spontaneous clearance of chronic hepatitis C virus infection. J Hepatol. 2016;65:266-72.
PubMed Abstract»Busch MP, Shafer KA. Acute-phase hepatitis C virus infection: implications for research, diagnosis, and treatment. Clin Infect Dis. 2005;40:959-61.
PubMed Abstract»Centers for Disease Control and Prevention. Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. Centers for Disease Control and Prevention. MMWR Recomm Rep. 1998;47(RR-19):1-39.
CDC and MMWR»Chu CM, Yeh CT, Liaw YF. Fulminant hepatic failure in acute hepatitis C: increased risk in chronic carriers of hepatitis B virus. Gut. 1999;45:613-7.
PubMed Abstract»Chung RT. Acute hepatitis C virus infection. Clin Infect Dis. 2005;41 Suppl 1:S14-7.
PubMed Abstract»Gerlach JT, Diepolder HM, Zachoval R, et al. Acute hepatitis C: high rate of both spontaneous and treatment-induced viral clearance. Gastroenterology. 2003;125:80-8.
PubMed Abstract»Grebely J, Matthews GV, Dore GJ. Treatment of acute HCV infection. Nat Rev Gastroenterol Hepatol. 2011;8:265-74.
PubMed Abstract»Hoofnagle JH, Carithers RL Jr, Shapiro C, Ascher N. Fulminant hepatic failure: summary of a workshop. Hepatology. 1995;21:240-52.
PubMed Abstract»Jin F, Matthews GV, Grulich AE. Sexual transmission of hepatitis C virus among gay and bisexual men: a systematic review. Sex Health. 2017;14:28-41.
PubMed Abstract»Kamal SM. Acute hepatitis C: a systematic review. Am J Gastroenterol. 2008;103:1283-97.
PubMed Abstract»Kimble MM, Javanbakht M, Chew KW, et al. Sociodemographic and clinical characteristics of persons who experienced spontaneous hepatitis C viral clearance. BMC Infect Dis. 2019;19:626.
PubMed Abstract»Maheshwari A, Ray S, Thuluvath PJ. Acute hepatitis C. Lancet. 2008;372(9635):321-32.
PubMed Abstract»Marcellin P. Hepatitis C: the clinical spectrum of the disease. J Hepatol. 1999;31 Suppl 1:9-16.
PubMed Abstract»Newsum AM, Schinkel J, van de Laar TJW, van der Meer JTM, Prins M. Spontaneous Clearance of Hepatitis C Virus Infection Among Human Immunodeficiency Virus-Infected Men Who Have Sex With Men. Open Forum Infect Dis. 2017;4:ofx090.
PubMed Abstract»Ragonnet R, Deuffic-Burban S, Boesecke C, et al. Estimating the Time to Diagnosis and the Chance of Spontaneous Clearance During Acute Hepatitis C in Human Immunodeficiency Virus-Infected Individuals. Open Forum Infect Dis. 2017;4:ofw235.
PubMed Abstract»Rao A, Rule JA, Cerro-Chiang G, et al. Role of Hepatitis C Infection in Acute Liver Injury/Acute Liver Failure in North America. Dig Dis Sci. 2023;68:304-11.
PubMed Abstract»Seo S, Silverberg MJ, Hurley LB, et al. Prevalence of Spontaneous Clearance of Hepatitis C Virus Infection Doubled From 1998 to 2017. Clin Gastroenterol Hepatol. 2020;18:511-3.
PubMed Abstract»Smith DJ, Jordan AE, Frank M, Hagan H. Spontaneous viral clearance of hepatitis C virus (HCV) infection among people who inject drugs (PWID) and HIV-positive men who have sex with men (HIV+ MSM): a systematic review and meta-analysis. BMC Infect Dis. 2016;16:471.
PubMed Abstract»Thomas DL, Astemborski J, Rai RM, et al. The natural history of hepatitis C virus infection: host, viral, and environmental factors. JAMA 2000;284:450-6.
PubMed Abstract»Laboratory Studies Used for the Evaluation of Initial HCV Infection
Busch MP, Murthy KK, Kleinman SH, et al. Infectivity in chimpanzees (Pan troglodytes) of plasma collected before HCV RNA detectability by FDA-licensed assays: implications for transfusion safety and HCV infection outcomes. Blood. 2012;119:6326-34.
PubMed Abstract»Busch MP, Shafer KA. Acute-phase hepatitis C virus infection: implications for research, diagnosis, and treatment. Clin Infect Dis. 2005;40:959-61.
PubMed Abstract»Chung RT. Acute hepatitis C virus infection. Clin Infect Dis. 2005;41 Suppl 1:S14-7.
PubMed Abstract»Cox AL, Netski DM, Mosbruger T, et al. Prospective evaluation of community-acquired acute-phase hepatitis C virus infection. Clin Infect Dis. 2005;40:951-8.
PubMed Abstract»Dustin LB, Rice CM. Flying under the radar: the immunobiology of hepatitis C. Annu Rev Immunol. 2007;25:71-99.
PubMed Abstract»Freiman JM, Tran TM, Schumacher SG, et al. Hepatitis C Core Antigen Testing for Diagnosis of Hepatitis C Virus Infection: A Systematic Review and Meta-analysis. Ann Intern Med. 2016;165:345-55.
PubMed Abstract»Gawlik K, Gallay PA. HCV core protein and virus assembly: what we know without structures. Immunol Res. 2014;60:1-10.
PubMed Abstract»Glynn SA, Wright DJ, Kleinman SH, et al. Dynamics of viremia in early hepatitis C virus infection. Transfusion. 2005;45:994-1002.
PubMed Abstract»Grebely J, Matthews GV, Dore GJ. Treatment of acute HCV infection. Nat Rev Gastroenterol Hepatol. 2011;8:265-74.
PubMed Abstract»Hajarizadeh B, Grebely J, Dore GJ. Case definitions for acute hepatitis C virus infection: A systematic review. J Hepatol. 2012;57:1349-60.
PubMed Abstract»Hullegie SJ, GeurtsvanKessel CH, van der Eijk AA, Ramakers C, Rijnders BJA. HCV antigen instead of RNA testing to diagnose acute HCV in patients treated in the Dutch Acute HCV in HIV Study. J Int AIDS Soc. 2017;20:21621.
PubMed Abstract»Khan H, Hill A, Main J, Brown A, Cooke G. Can Hepatitis C Virus Antigen Testing Replace Ribonucleic Acid Polymearse Chain Reaction Analysis for Detecting Hepatitis C Virus? A Systematic Review. Open Forum Infect Dis. 2017;4:ofw252.
PubMed Abstract»Klein KC, Polyak SJ, Lingappa JR. Unique features of hepatitis C virus capsid formation revealed by de novo cell-free assembly. J Virol. 2004;78:9257-69.
PubMed Abstract»Laperche S, Le Marrec N, Girault A, et al. Simultaneous detection of hepatitis C virus (HCV) core antigen and anti-HCV antibodies improves the early detection of HCV infection. J Clin Microbiol. 2005;43:3877-83.
PubMed Abstract»Laperche S, Nübling CM, Stramer SL, et al. Sensitivity of hepatitis C virus core antigen and antibody combination assays in a global panel of window period samples. Transfusion. 2015;55:2489-98.
PubMed Abstract»Maheshwari A, Ray S, Thuluvath PJ. Acute hepatitis C. Lancet. 2008;372(9635):321-32.
PubMed Abstract»Mondelli MU, Cerino A, Cividini A. Acute hepatitis C: diagnosis and management. J Hepatol. 2005;42 Suppl(1):S108-14.
PubMed Abstract»Nübling CM, Unger G, Chudy M, Raia S, Löwer J. Sensitivity of HCV core antigen and HCV RNA detection in the early infection phase. Transfusion. 2002;42:1037-45.
PubMed Abstract»Ottiger C, Gygli N, Huber AR. Detection limit of architect hepatitis C core antigen assay in correlation with HCV RNA, and renewed confirmation algorithm for reactive anti-HCV samples. J Clin Virol. 2013;58:535-40.
PubMed Abstract»Ross RS, Viazov S, Salloum S, Hilgard P, Gerken G, Roggendorf M. Analytical performance characteristics and clinical utility of a novel assay for total hepatitis C virus core antigen quantification. J Clin Microbiol. 2010;48:1161-8.
PubMed Abstract»Stramer SL, Glynn SA, Kleinman SH, et al. Detection of HIV-1 and HCV infections among antibody-negative blood donors by nucleic acid-amplification testing. N Engl J Med. 2004;351:760-8.
PubMed Abstract»Tuke PW, Grant PR, Waite J, Kitchen AD, Eglin RP, Tedder RS. Hepatitis C virus window-phase infections: closing the window on hepatitis C virus. Transfusion. 2008;48:594-600.
PubMed Abstract»Diagnosis of Acute HCV Infection
Centers for Disease Control and Prevention (CDC). National Notifiable Diseases Surveillance System (NNDSS). Hepatitis C,
Perinatal Infection 2018 Case Definition
CDC»Centers for Disease Control and Prevention (CDC). National Notifiable Diseases Surveillance System (NNDSS). Hepatitis C, Acute: 2020 Case Definition.
CDC and NNDSS»Additional References
Aisyah DN, Shallcross L, Hully AJ, O'Brien A, Hayward A. Assessing hepatitis C spontaneous clearance and understanding associated factors-A systematic review and meta-analysis. J Viral Hepat. 2018;25:680-698.
PubMed Abstract»Araujo AC, Astrakhantseva IV, Fields HA, Kamili S. Distinguishing acute from chronic hepatitis C virus (HCV) infection based on antibody reactivities to specific HCV structural and nonstructural proteins. J Clin Microbiol. 2011;49:54-7.
PubMed Abstract»Butt AA, Yan P, Shaikh OS, Chung RT, Sherman KE. Treatment adherence and virological response rates in hepatitis C virus infected persons treated with sofosbuvir-based regimens: results from ERCHIVES. Liver Int. 2016;36:1275-83.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). National Notifiable Diseases Surveillance System (NNDSS). Hepatitis C, Acute: 2020 Case Definition.
CDC and NNDSS»Evon DM, Esserman DA, Bonner JE, Rao T, Fried MW, Golin CE. Adherence to PEG/ribavirin treatment for chronic hepatitis C: prevalence, patterns, and predictors of missed doses and nonpersistence. J Viral Hepat. 2013;20:536-49.
PubMed Abstract»Freiman JM, Tran TM, Schumacher SG, et al. Hepatitis C Core Antigen Testing for Diagnosis of Hepatitis C Virus Infection: A Systematic Review and Meta-analysis. Ann Intern Med. 2016;165:345-55.
PubMed Abstract»Glynn SA, Wright DJ, Kleinman SH, et al. Dynamics of viremia in early hepatitis C virus infection. Transfusion. 2005;45:994-1002.
PubMed Abstract»Hullegie SJ, Arends JE, Rijnders BJ, et al. Current knowledge and future perspectives on acute hepatitis C infection. Clin Microbiol Infect. 2015;21:797.e9-797.e17.
PubMed Abstract»Hullegie SJ, GeurtsvanKessel CH, van der Eijk AA, Ramakers C, Rijnders BJA. HCV antigen instead of RNA testing to diagnose acute HCV in patients treated in the Dutch Acute HCV in HIV Study. J Int AIDS Soc. 2017;20:21621.
PubMed Abstract»Jin F, Matthews GV, Grulich AE. Sexual transmission of hepatitis C virus among gay and bisexual men: a systematic review. Sex Health. 2017;14:28-41.
PubMed Abstract»Khan H, Hill A, Main J, Brown A, Cooke G. Can Hepatitis C Virus Antigen Testing Replace Ribonucleic Acid Polymearse Chain Reaction Analysis for Detecting Hepatitis C Virus? A Systematic Review. Open Forum Infect Dis. 2017;4:ofw252.
PubMed Abstract»Lamoury FMJ, Soker A, Martinez D, et al. Hepatitis C virus core antigen: A simplified treatment monitoring tool, including for post-treatment relapse. J Clin Virol. 2017;92:32-38.
PubMed Abstract»Laperche S, Nübling CM, Stramer SL, et al. Sensitivity of hepatitis C virus core antigen and antibody combination assays in a global panel of window period samples. Transfusion. 2015;55:2489-98.
PubMed Abstract»Lo Re V, 3rd, Amorosa VK, Localio AR, et al. Adherence to hepatitis C virus therapy and early virologic outcomes. Clin Infect Dis. 2009;48:186-93.
PubMed Abstract»Lo Re V, 3rd, Teal V, Localio AR, Amorosa VK, Kaplan DE, Gross R. Adherence to hepatitis C virus therapy in HIV/hepatitis C-coinfected patients. AIDS Behav. 2013;17:94-103.
PubMed Abstract»Lo Re V, 3rd, Teal V, Localio AR, Amorosa VK, Kaplan DE, Gross R. Relationship between adherence to hepatitis C virus therapy and virologic outcomes: a cohort study. Ann Intern Med. 2011;155:353-60.
PubMed Abstract»Ottiger C, Gygli N, Huber AR. Detection limit of architect hepatitis C core antigen assay in correlation with HCV RNA, and renewed confirmation algorithm for reactive anti-HCV samples. J Clin Virol. 2013;58:535-40.
PubMed Abstract»Petersen T, Townsend K, Gordon LA, et al. High adherence to all-oral directly acting antiviral HCV therapy among an inner-city patient population in a phase 2a study. Hepatol Int. 2016;10:310-9.
PubMed Abstract»Wietzke-Braun P, Manhardt LB, Rosenberger A, Uy A, Ramadori G, Mihm S. Spontaneous elimination of hepatitis C virus infection: a retrospective study on demographic, clinical, and serological correlates. World J Gastroenterol. 2007;13:4224-9.
PubMed Abstract»Younossi ZM, Stepanova M, Henry L, Nader F, Younossi Y, Hunt S. Adherence to treatment of chronic hepatitis C: from interferon containing regimens to interferon and ribavirin free regimens. Medicine (Baltimore). 2016;95:e4151.
PubMed Abstract»Zibbell JE, Asher AK, Patel RC, et al. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am J Public Health. 2018;108:175-181.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»Module 2. Evaluation, Staging, and Monitoring of Chronic Hepatitis C
Lesson 1. Initial Evaluation of Persons with Chronic HCV
Background
Arora S, Thornton K, Jenkusky SM, Parish B, Scaletti JV. Project ECHO: linking university specialists with rural and prison-based clinicians to improve care for people with chronic hepatitis C in New Mexico. Public Health Rep. 2007;122 Suppl 2:74-7.
PubMed Abstract»Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364:2199-207.
PubMed Abstract»Guss D, Sherigar J, Rosen P, Mohanty SR. Diagnosis and Management of Hepatitis C Infection in Primary Care Settings. J Gen Intern Med. 2018;33:551-7.
PubMed Abstract»General Approach to Initial Evaluation
Bräu N. Evaluation of the hepatitis C virus-infected patient: the initial encounter. Clin Infect Dis. 2013;56:853-60.
PubMed Abstract»Key Aspects of Medical History
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Bacon BR, Adams PC, Kowdley KV, Powell LW, Tavill AS; American Association for the Study of Liver Diseases. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54:328-43.
PubMed Abstract»Bialek SR, Terrault NA. The changing epidemiology and natural history of hepatitis C virus infection. Clin Liver Dis. 2006;10:697-715.
PubMed Abstract»Bräu N. Evaluation of the hepatitis C virus-infected patient: the initial encounter. Clin Infect Dis. 2013;56:853-60.
PubMed Abstract»Bradley KA, Bush KR, Epler AJ, et al. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med. 2003;163:821-9.
PubMed Abstract»Bradshaw D1, Matthews G, Danta M. Sexually transmitted hepatitis C infection: the new epidemic in MSM? Curr Opin Infect Dis. 2013;26:66-72.
PubMed Abstract»Buchsbaum DG, Buchanan RG, Centor RM, Schnoll SH, Lawton MJ. Screening for alcohol abuse using CAGE scores and likelihood ratios. Ann Intern Med. 1991;115:774-7.
PubMed Abstract»Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158:1789-95.
PubMed Abstract»Cacoub P, Poynard T, Ghillani P, et al. Extrahepatic manifestations of chronic hepatitis C. MULTIVIRC Group. Multidepartment Virus C. Arthritis Rheum. 1999;42:2204-12.
PubMed Abstract»Castera L. Noninvasive methods to assess liver disease in patients with hepatitis B or C. Gastroenterology. 2012;142:1293-1302.e4.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Centers for Disease Control and Prevention (CDC). Testing for HCV infection: an update of guidance for clinicians and laboratorians. MMWR Morb Mortal Wkly Rep. 2013;62:362-5.
PubMed Abstract»Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592-609.
PubMed Abstract»Charre C, Cotte L, Kramer R, et al. Hepatitis C virus spread from HIV-positive to HIV-negative men who have sex with men. PLoS One. 2018;13:e0190340.
PubMed Abstract»Chasser Y, Kim AY, Freudenreich O. Hepatitis C Treatment: Clinical Issues for Psychiatrists in the Post-Interferon Era. Psychosomatics. 2017;58:1-10.
PubMed Abstract»Chen CM, Yoon YH, Yi HY, Lucas DL. Alcohol and hepatitis C mortality among males and females in the United States: a life table analysis. Alcohol Clin Exp Res. 2007;31:285-92.
PubMed Abstract»Cox AL, Thomas DL. Hepatitis C virus vaccines among people who inject drugs. Clin Infect Dis. 2013;57 Suppl 2:S46-50.
PubMed Abstract»Czaja AJ. Review article: next-generation transformative advances in the pathogenesis and management of autoimmune hepatitis. Aliment Pharmacol Ther. 2017;46:920-937.
PubMed Abstract»Diehl AM, Day C. Cause, Pathogenesis, and Treatment of Nonalcoholic Steatohepatitis. N Engl J Med. 2017;377:2063-2072.
PubMed Abstract»Falade-Nwulia O, Sulkowski MS, Merkow A, Latkin C, Mehta SH. Understanding and addressing hepatitis C reinfection in the oral direct-acting antiviral era. J Viral Hepat. 2018;25:220-227.
PubMed Abstract»Fill MA, Sizemore LA, Rickles M, et al. Epidemiology and risk factors for hepatitis C virus infection in a high-prevalence population. Epidemiol Infect. 2018:1-7.
PubMed Abstract»Ghany MG, Strader DB, Thomas DL, Seeff LB; American Association for the Study of Liver Diseases. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335-74.
AASLD Practice Guidelines»Grady BP, Schinkel J, Thomas XV, Dalgard O. Hepatitis C virus reinfection following treatment among people who use drugs. Clin Infect Dis. 2013;57 Suppl 2:S105-10.
PubMed Abstract»Hagan H, Neurer J, Jordan AE, et al. Hepatitis C virus infection among HIV-positive men who have sex with men: protocol for a systematic review and meta-analysis. Syst Rev. 2014;3:31.
PubMed Abstract»Hauser P, Kern S. Psychiatric and substance use disorders co-morbidities and hepatitis C: Diagnostic and treatment implications. World J Hepatol. 2015;7:1921-35.
PubMed Abstract»Jamma S, Hussain G, Lau DT. Current Concepts of HBV/HCV Coinfection: Coexistence, but Not Necessarily in Harmony. Curr Hepat Rep. 2010;9:260-9.
PubMed Abstract»Kim AY, Onofrey S, Church DR. An epidemiologic update on hepatitis C infection in persons living with or at risk of HIV infection. J Infect Dis. 2013;207 Suppl 1:S1-6.
PubMed Abstract»Mack CL, Adams D, Assis DN, et al. Diagnosis and Management of Autoimmune Hepatitis in Adults and Children: 2019 Practice Guidance and Guidelines From the American Association for the Study of Liver Diseases. Hepatology. 2020;72:671-722.
PubMed Abstract»Manns MP, Czaja AJ, Gorham JD, et al. Diagnosis and management of autoimmune hepatitis. Hepatology. 2010;51:2193-213.
PubMed Abstract»Martinello M, Hajarizadeh B, Grebely J, Dore GJ, Matthews GV. HCV Cure and Reinfection Among People With HIV/HCV Coinfection and People Who Inject Drugs. Curr HIV/AIDS Rep. 2017;14:110-121.
PubMed Abstract»McGowan CE, Fried MW. Barriers to hepatitis C treatment. Liver Int. 2012;32 Suppl 1:151-6.
PubMed Abstract»Missiha SB, Ostrowski M, Heathcote EJ. Disease progression in chronic hepatitis C: modifiable and nonmodifiable factors. Gastroenterology. 2008;134;1699-714.
PubMed Abstract»Nelson DR, Teckman J, Di Bisceglie AM, Brenner DA. Diagnosis and management of patients with α1-antitrypsin (A1AT) deficiency. Clin Gastroenterol Hepatol. 2012;10:575-80.
PubMed Abstract»Page K, Morris MD, Hahn JA, Maher L, Prins M. Injection drug use and hepatitis C virus infection in young adult injectors: using evidence to inform comprehensive prevention. Clin Infect Dis. 2013;57 Suppl 2:S32-8.
PubMed Abstract»Pappachan JM, Babu S, Krishnan B, Ravindran NC. Non-alcoholic Fatty Liver Disease: A Clinical Update. J Clin Transl Hepatol. 2017;5:384-393.
PubMed Abstract»Pascale A, Pais R, Ratziu V. An overview of nonalcoholic steatohepatitis: past, present and future directions. J Gastrointestin Liver Dis. 2010;19:415-23.
PubMed Abstract»Poynard T, Ratziu V, Charlotte F, Goodman Z, McHutchison J, Albrecht J. Rates and risk factors of liver fibrosis progression in patients with chronic hepatitis C. J Hepatol. 2001;34:730-9.
PubMed Abstract»Rifai MA, Indest D, Loftis J, Hauser P. Psychiatric management of the hepatitis C patient. Curr Treat Options Gastroenterol. 2006;9:508-19.
PubMed Abstract»Rinella ME, Lazarus JV, Ratziu V, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol. 2023;79:1542-56.
PubMed Abstract»Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015;313:2263-73.
PubMed Abstract»Schaefer M, Hinzpeter A, Mohmand A, et al. Hepatitis C treatment in "difficult-to-treat" psychiatric patients with pegylated interferon-alpha and ribavirin: response and psychiatric side effects. Hepatology. 2007;46:991-8.
PubMed Abstract»Sherman AC, Sherman KE. Extrahepatic manifestations of hepatitis C infection: navigating CHASM. Curr HIV/AIDS Rep. 2015;12:353-61.
PubMed Abstract»Sockalingam S, Tseng A, Giguere P, Wong D. Psychiatric treatment considerations with direct acting antivirals in hepatitis C. BMC Gastroenterol. 2013;13:86.
PubMed Abstract»Theise ND. Liver biopsy assessment in chronic viral hepatitis: a personal, practical approach. Mod Pathol. 2007;20 Suppl 1:S3-14.
PubMed Abstract»van de Laar TJ, Matthews GV, Prins M, Danta M. Acute hepatitis C in HIV-infected men who have sex with men: an emerging sexually transmitted infection. AIDS. 2010;24:1799-812.
PubMed Abstract»Vento S, Garofano T, Renzini C, et al. Fulminant hepatitis associated with hepatitis A virus superinfection in patients with chronic hepatitis C. N Engl J Med. 1998;338:286-90.
PubMed Abstract»Younossi Z, Park H, Henry L, Adeyemi A, Stepanova M. Extrahepatic Manifestations of Hepatitis C: A Meta-analysis of Prevalence, Quality of Life, and Economic Burden. Gastroenterology. 2016;150:1599-1608.
PubMed Abstract»Zibbell JE, Asher AK, Patel RC, et al. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am J Public Health. 2018;108:175-181.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»Key Aspects of Physical Examination
Cattau EL Jr, Benjamin SB, Knuff TE, Castell DO. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982;247:1164-6.
PubMed Abstract»de Bruyn G, Graviss EA. A systematic review of the diagnostic accuracy of physical examination for the detection of cirrhosis. BMC Med Inform Decis Mak. 2001;1:6.
PubMed Abstract»Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. Am Fam Physician. 2006;74:756-62.
PubMed Abstract»Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. Am Fam Physician.2006;74:756-62.
PubMed Abstract»Holzberg M, Walker HK. Terry's nails: revised definition and new correlations. Lancet. 1984;1:896-9.
PubMed Abstract»Karnath B. Stigmata of chronic liver disease. Hospital Physician. 2003;39:14-16.
Turner White Communications, Inc.»Kim Sh, Keum B, Kim E, Jeen Y, Chun H. Hepatobiliary and pancreatic: Caput medusae. J Gastroenterol Hepatol. 2014;29:1952.
PubMed Abstract»Li CP, Lee FY, Hwang SJ, et al. Role of substance P in the pathogenesis of spider angiomas in patients with nonalcoholic liver cirrhosis. Am J Gastroenterol. 1999;94:502-7.
PubMed Abstract»Li CP, Lee FY, Hwang SJ, et al. Spider angiomas in patients with liver cirrhosis: role of vascular endothelial growth factor and basic fibroblast growth factor. World J Gastroenterol. 2003;9:2832-5.
PubMed Abstract»Li L, Duan M, Chen W, et al. The spleen in liver cirrhosis: revisiting an old enemy with novel targets. J Transl Med. 2017;15:111.
PubMed Abstract»Pitukweerakul S, Pilla S. Terry's Nails and Lindsay's Nails: Two Nail Abnormalities in Chronic Systemic Diseases. J Gen Intern Med. 2016;31:970.
PubMed Abstract»Ruiz MA, Saab S, Rickman LS. The clinical detection of scleral icterus: observations of multiple examiners. Mil Med. 1997;162:560-3.
PubMed Abstract»Satapathy SK, Bernstein D. Dermatologic disorders and the liver. Clin Liver Dis. 2011;15:165-82.
PubMed Abstract»Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012;307:832-42.
PubMed Abstract»Yang PM, Chen DS. Images in clinical medicine. Caput medusae. N Engl J Med. 2005;353:e19.
PubMed Abstract»Recommended Initial Laboratory Studies
Alter MJ, Kruszon-Moran D, Nainan OV, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999;341:556-62.
PubMed Abstract»Bräu N. Evaluation of the hepatitis C virus-infected patient: the initial encounter. Clin Infect Dis. 2013;56:853-60.
PubMed Abstract»Sherman AC, Sherman KE. Extrahepatic manifestations of hepatitis C infection: navigating CHASM. Curr HIV/AIDS Rep. 2015;12:353-61.
PubMed Abstract»Thomas DL, Thio CL, Martin MP, et al. Genetic variation in IL28B and spontaneous clearance of hepatitis C virus. Nature. 2009;461:798-801.
PubMed Abstract»Zeuzem S, Rodríguez-Torres M, Rajender Reddy K, et al. Optimized threshold for serum HCV RNA to predict treatment outcomes in hepatitis C patients receiving peginterferon alfa-2a/ribavirin. J Viral Hepat. 2012;19:766-74.
PubMed Abstract»Immunizations for Persons with Chronic HCV
Advisory Committee on Immunization Practices (ACIP), Fiore AE, Wasley A, Bell BP. Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2006;55:1-23.
PubMed Abstract»Advisory Committee on Immunization Practices. Recommended adult immunization schedule: United States, 2012. Ann Intern Med. 2012;156:211-7.
PubMed Abstract»Advisory Committee on Immunization Practices. Recommended Immunization Schedule for Adults Aged 19 Years or Older by Medical Conditions and Other Indications, United States, 2024
ACIP»Centers for Disease Control and Prevention (CDC); Advisory Committee on Immunization Practices. Updated recommendations for prevention of invasive pneumococcal disease among adults using the 23-valent pneumococcal polysaccharide vaccine (PPSV23). MMWR Morb Mortal Wkly Rep. 2010;59:1102-6.
PubMed Abstract»Ghany MG, Strader DB, Thomas DL, Seeff LB; American Association for the Study of Liver Diseases. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335-74.
AASLD Practice Guidelines»Jackson S, Lentino J, Kopp J, et al. Immunogenicity of a two-dose investigational hepatitis B vaccine, HBsAg-1018, using a toll-like receptor 9 agonist adjuvant compared with a licensed hepatitis B vaccine in adults. Vaccine. 2018;36:668-674.
PubMed Abstract»Keeffe EB, Iwarson S, McMahon BJ, et al. Safety and immunogenicity of hepatitis A vaccine in patients with chronic liver disease. Hepatology. 1998;27:881-6.
PubMed Abstract»Lee SD, Chan CY, Yu MI, et al. Safety and immunogenicity of inactivated hepatitis A vaccine in patients with chronic liver disease. J Med Virol. 1997;52:215-8.
PubMed Abstract»Mast EE, Weinbaum CM, Fiore AE, et al. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) Part II: immunization of adults. MMWR Recomm Rep. 2006;55:1-33; quiz CE1-4.
PubMed Abstract»Nelson NP, Weng MK, Hofmeister MG, et al. Prevention of Hepatitis A Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization Practices, 2020. MMWR Recomm Rep. 2020;69:1-38.
PubMed Abstract»Schillie S, Vellozzi C, Reingold A, et al. Prevention of Hepatitis B Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 2018;67:1-31.
PubMed Abstract»Vento S, Garofano T, Renzini C, et al. Fulminant hepatitis associated with hepatitis A virus superinfection in patients with chronic hepatitis C. N Engl J Med. 1998;338:286-90.
PubMed Abstract»Screening for other Causes of Liver Disease
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»Bacon BR, Adams PC, Kowdley KV, Powell LW, Tavill AS; American Association for the Study of Liver Diseases. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54:328-43.
PubMed Abstract»Bacon BR, Adams PC, Kowdley KV, Powell LW, Tavill AS. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54:328-43.
PubMed Abstract»Brandhagen DJ, Fairbanks VF, Baldus W. Recognition and management of hereditary hemochromatosis. Am Fam Physician. 2002;65:853-60.
PubMed Abstract»Buchsbaum DG, Buchanan RG, Centor RM, Schnoll SH, Lawton MJ. Screening for alcohol abuse using CAGE scores and likelihood ratios. Ann Intern Med. 1991;115:774-7.
PubMed Abstract»Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592-609.
PubMed Abstract»Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328-57.
PubMed Abstract»Cohen JA, Kaplan MM. The SGOT/SGPT ratio--an indicator of alcoholic liver disease. Dig Dis Sci. 1979;24:835-8.
PubMed Abstract»Czaja AJ, Freese DK; American Association for the Study of Liver Disease. Diagnosis and treatment of autoimmune hepatitis. Hepatology. 2002;36:479-97.
PubMed Abstract»Diehl AM, Day C. Cause, Pathogenesis, and Treatment of Nonalcoholic Steatohepatitis. N Engl J Med. 2017;377:2063-2072.
PubMed Abstract»Dugum M, McCullough A. Diagnosis and Management of Alcoholic Liver Disease. J Clin Transl Hepatol. 2015;3:109-16.
PubMed Abstract»Ghany MG, Nelson DR, Strader DB, Thomas DL, Seeff LB; American Association for the Study of Liver Diseases. An update on treatment of genotype 1 chronic hepatitis C virus infection: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54:1433-44.
PubMed Abstract»Hennes EM, Zeniya M, Czaja AJ, et al. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology. 2008;48:169-76.
PubMed Abstract»Heymsfield SB, Wadden TA. Mechanisms, Pathophysiology, and Management of Obesity. N Engl J Med. 2017;376:254-266.
PubMed Abstract»Kane SF, Roberts C, Paulus R. Hereditary Hemochromatosis: Rapid Evidence Review. Am Fam Physician. 2021;104:263-70.
PubMed Abstract»Lucey MR, Mathurin P, Morgan TR. Alcoholic hepatitis. N Engl J Med. 2009;360:2758-69.
PubMed Abstract»Mack CL, Adams D, Assis DN, et al. Diagnosis and Management of Autoimmune Hepatitis in Adults and Children: 2019 Practice Guidance and Guidelines From the American Association for the Study of Liver Diseases. Hepatology. 2020;72:671-722.
PubMed Abstract»Manns MP, Czaja AJ, Gorham JD, et al. Diagnosis and management of autoimmune hepatitis. Hepatology. 2010;51:2193-213.
PubMed Abstract»Manns MP, Lohse AW, Vergani D. Autoimmune hepatitis--Update 2015. J Hepatol. 2015;62:S100-11.
PubMed Abstract»Marciniak SJ, Lomas DA. Alpha1-antitrypsin deficiency and autophagy. N Engl J Med. 2010;363:1863-4.
PubMed Abstract»Mieli-Vergani G, Vergani D, Czaja AJ, et al. Autoimmune hepatitis. Nat Rev Dis Primers. 2018;4:18017.
PubMed Abstract»Nelson DR, Teckman J, Di Bisceglie AM, Brenner DA. Diagnosis and management of patients with α1-antitrypsin (A1AT) deficiency. Clin Gastroenterol Hepatol. 2012;10:575-80.
PubMed Abstract»Pascale A, Pais R, Ratziu V. An overview of nonalcoholic steatohepatitis: past, present and future directions. J Gastrointestin Liver Dis. 2010;19:415-23.
PubMed Abstract»Poynard T, Bedossa P, Opolon P. Lancet. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825-32.
PubMed Abstract»Qaseem A, Aronson M, Fitterman N, Snow V, Weiss KB, Owens DK. Screening for hereditary hemochromatosis: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2005;143:517-21.
PubMed Abstract»Rinella ME, Lazarus JV, Ratziu V, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol. 2023;79:1542-56.
PubMed Abstract»Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015;313:2263-73.
PubMed Abstract»Schmitt B, Golub RM, Green R. Screening primary care patients for hereditary hemochromatosis with transferrin saturation and serum ferritin level: systematic review for the American College of Physicians. Ann Intern Med. 2005;143:522-36.
PubMed Abstract»Shrestha R, Kc S, Thapa P, Pokharel A, Karki N, Jaishi B. Estimation of Liver Fat by FibroScan in Patients With Nonalcoholic Fatty Liver Disease. Cureus. 2021;13:e16414.
PubMed Abstract»Singal AK, Bataller R, Ahn J, Kamath PS, Shah VH. ACG Clinical Guideline: Alcoholic Liver Disease. Am J Gastroenterol. 2018;113:175-194.
PubMed Abstract»Tome S, Lucey MR. Review article: current management of alcoholic liver disease. Aliment Pharmacol Ther. 2004;19:707-14.
PubMed Abstract»Wang T, Xi Y, Raji A, et al. Overall and subgroup prevalence of non-alcoholic fatty liver disease and prevalence of advanced fibrosis in the United States: An updated national estimate in National Health and Nutrition Examination Survey (NHANES) 2011-2018. Ann Hepatol. 2024;29:101154.
PubMed Abstract»Wiley TE, McCarthy M, Breidi L, McCarthy M, Layden TJ. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology. 1998;28:805-9.
PubMed Abstract»Yasui S, Fujiwara K, Yokosuka O. Autoimmune fulminant hepatic failure in chronic hepatitis C during Peg-interferon-alpha 2b plus ribavirin treatment showing histological heterogeneity. Dig Liver Dis. 2011;43:666-7.
PubMed Abstract»Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11-20.
PubMed Abstract»Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73-84.
PubMed Abstract»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»Ahmed A, Wong RJ, Harrison SA. Nonalcoholic Fatty Liver Disease Review: Diagnosis, Treatment, and Outcomes. Clin Gastroenterol Hepatol. 2015;13:2062-70.
PubMed Abstract»Alter MJ. Hepatitis C virus infection in the United States. J Hepatol. 1999;31 Suppl 1:88-91.
PubMed Abstract»Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364:2199-207.
PubMed Abstract»Bradshaw D1, Matthews G, Danta M. Sexually transmitted hepatitis C infection: the new epidemic in MSM? Curr Opin Infect Dis. 2013;26:66-72.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Centers for Disease Control and Prevention (CDC). Testing for HCV infection: an update of guidance for clinicians and laboratorians. MMWR Morb Mortal Wkly Rep. 2013;62:362-5.
PubMed Abstract»Falade-Nwulia O, Sulkowski MS, Merkow A, Latkin C, Mehta SH. Understanding and addressing hepatitis C reinfection in the oral direct-acting antiviral era. J Viral Hepat. 2018;25:220-227.
PubMed Abstract»Grady BP, Schinkel J, Thomas XV, Dalgard O. Hepatitis C virus reinfection following treatment among people who use drugs. Clin Infect Dis. 2013;57 Suppl 2:S105-10.
PubMed Abstract»Guss D, Sherigar J, Rosen P, Mohanty SR. Diagnosis and Management of Hepatitis C Infection in Primary Care Settings. J Gen Intern Med. 2018;33:551-7.
PubMed Abstract»Martinello M, Hajarizadeh B, Grebely J, Dore GJ, Matthews GV. HCV Cure and Reinfection Among People With HIV/HCV Coinfection and People Who Inject Drugs. Curr HIV/AIDS Rep. 2017;14:110-121.
PubMed Abstract»Stevenson M, Lloyd-Jones M, Morgan MY, Wong R. Non-invasive diagnostic assessment tools for the detection of liver fibrosis in patients with suspected alcohol-related liver disease: a systematic review and economic evaluation. Health Technol Assess. 2012;16:1-174.
PubMed Abstract»van de Laar TJ, Matthews GV, Prins M, Danta M. Acute hepatitis C in HIV-infected men who have sex with men: an emerging sexually transmitted infection. AIDS. 2010;24:1799-812.
PubMed Abstract»Zibbell JE, Asher AK, Patel RC, et al. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am J Public Health. 2018;108:175-181.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»Lesson 2. Natural History of HCV Infection
Spontaneous Clearance versus Chronic Infection
Alter MJ, Kruszon-Moran D, Nainan OV, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999;341:556-62.
PubMed Abstract»Blackard JT, Shata MT, Shire NJ, Sherman KE. Acute hepatitis C virus infection: a chronic problem. Hepatology. 2008;47:321-31.
PubMed Abstract»Danta M, Semmo N, Fabris P, et al. Impact of HIV on host-virus interactions during early hepatitis C virus infection. J Infect Dis. 2008;197:1558-66.
PubMed Abstract»Gerlach JT, Diepolder HM, Jung MC, et al. Recurrence of hepatitis C virus after loss of virus-specific CD4(+) T-cell response in acute hepatitis C. Gastroenterology. 1999;117:933-41.
PubMed Abstract»Grebely J, Page K, Sacks-Davis R, et al. The effects of female sex, viral genotype, and IL28B genotype on spontaneous clearance of acute hepatitis C virus infection. Hepatology. 2014;59:109-20.
PubMed Abstract»Grebely J, Petoumenos K, Hellard M, et al. Potential role for interleukin-28B genotype in treatment decision-making in recent hepatitis C virus infection. Hepatology. 2010;52:1216-24.
PubMed Abstract»Kamal SM. Acute hepatitis C: a systematic review. Am J Gastroenterol. 2008;103:1283-97.
PubMed Abstract»Kenny-Walsh E. Clinical outcomes after hepatitis C infection from contaminated anti-D immune globulin. Irish Hepatology Research Group. N Engl J Med. 1999;340:1228-33.
PubMed Abstract»Kim AY, Kuntzen T, Timm J, et al. Spontaneous control of HCV is associated with expression of HLA-B 57 and preservation of targeted epitopes. Gastroenterology. 2011;140:686-696.e1.
PubMed Abstract»Levine RA, Sanderson SO, Ploutz-Snyder R, et al. Assessment of fibrosis progression in untreated Irish women with chronic hepatitis C contracted from immunoglobulin anti-D. Clin Gastroenterol Hepatol. 2006;4:1271-7.
PubMed Abstract»Liang TJ, Rehermann B, Seeff LB, Hoofnagle JH. Pathogenesis, natural history, treatment, and prevention of hepatitis C. Ann Intern Med. 2000;132:296-305.
PubMed Abstract»Maheshwari A, Ray S, Thuluvath PJ. Acute hepatitis C. Lancet. 2008;372(9635):321-32.
PubMed Abstract»Mehta SH, Cox A, Hoover DR, et al. Protection against persistence of hepatitis C. Lancet. 2002;359:1478-83.
PubMed Abstract»Micallef JM, Kaldor JM, Dore GJ. Spontaneous viral clearance following acute hepatitis C infection: a systematic review of longitudinal studies. J Viral Hepat. 2006;13:34-41.
PubMed Abstract»Newsum AM, Schinkel J, van de Laar TJW, van der Meer JTM, Prins M. Spontaneous Clearance of Hepatitis C Virus Infection Among Human Immunodeficiency Virus-Infected Men Who Have Sex With Men. Open Forum Infect Dis. 2017;4:ofx090.
PubMed Abstract»Rosen HR. Emerging concepts in immunity to hepatitis C virus infection. J Clin Invest. 2013;123:4121-30.
PubMed Abstract»Smith DJ, Jordan AE, Frank M, Hagan H. Spontaneous viral clearance of hepatitis C virus (HCV) infection among people who inject drugs (PWID) and HIV-positive men who have sex with men (HIV+ MSM): a systematic review and meta-analysis. BMC Infect Dis. 2016;16:471.
PubMed Abstract»Thomas DL, Astemborski J, Rai RM, et al. The natural history of hepatitis C virus infection: host, viral, and environmental factors. JAMA 2000;284:450-6.
PubMed Abstract»Thomas DL, Thio CL, Martin MP, et al. Genetic variation in IL28B and spontaneous clearance of hepatitis C virus. Nature. 2009;461:798-801.
PubMed Abstract»Tillmann HL, Thompson AJ, Patel K, et al. A polymorphism near IL28B is associated with spontaneous clearance of acute hepatitis C virus and jaundice. Gastroenterology. 2010;139:1586-92.
PubMed Abstract»Valencia A, Vergara C, Thio CL, et al. Trans-ancestral fine-mapping of MHC reveals key amino acids associated with spontaneous clearance of hepatitis C in HLA-DQβ1. Am J Hum Genet. 2022;109:299-310.
PubMed Abstract»Vogt M, Lang T, Frösner G, et al. Prevalence and clinical outcome of hepatitis C infection in children who underwent cardiac surgery before the implementation of blood-donor screening. N Engl J Med. 1999;341:866-70.
PubMed Abstract»Wang CC, Krantz E, Klarquist J, et al. Acute hepatitis C in a contemporary US cohort: modes of acquisition and factors influencing viral clearance. J Infect Dis. 2007;196:1474-82.
PubMed Abstract»Wojcik GL, Thio CL, Kao WH, et al. Admixture analysis of spontaneous hepatitis C virus clearance in individuals of African descent. Genes Immun. 2014;15:241-6.
PubMed Abstract»Variable Outcomes of Chronic Infection
Benvegnu L, Gios M, Boccato S, Alberti A. Natural history of compensated viral cirrhosis: a prospective study on the incidence and hierarchy of major complications. Gut. 2004;53:744-9.
PubMed Abstract»Donato F, Tagger A, Gelatti U, et al. Alcohol and hepatocellular carcinoma: the effect of lifetime intake and hepatitis virus infections in men and women. Am J Epidemiol. 2002;155:323-31.
PubMed Abstract»Freeman AJ, Dore GJ, Law MG, et al. Estimating progression to cirrhosis in chronic hepatitis C virus infection. Hepatology. 2001;34:809-16.
PubMed Abstract»Hajarizadeh B, Grebely J, Dore GJ. Epidemiology and natural history of HCV infection. Nat Rev Gastroenterol Hepatol. 2013;10:553-62.
PubMed Abstract»Krahn M, Wong JB, Heathcote J, Scully L, Seeff L. Estimating the prognosis of hepatitis C patients infected by transfusion in Canada between 1986 and 1990. Med Decis Making. 2004;24:20-9.
PubMed Abstract»Liang TJ, Rehermann B, Seeff LB, Hoofnagle JH. Pathogenesis, natural history, treatment, and prevention of hepatitis C. Ann Intern Med. 2000;132:296-305.
PubMed Abstract»Lingala S, Ghany MG. Natural History of Hepatitis C. Gastroenterol Clin North Am. 2015;44:717-34.
PubMed Abstract»Missiha SB, Ostrowski M, Heathcote EJ. Disease progression in chronic hepatitis C: modifiable and nonmodifiable factors. Gastroenterology. 2008;134;1699-714.
PubMed Abstract»Poynard T, Ratziu V, Charlotte F, Goodman Z, McHutchison J, Albrecht J. Rates and risk factors of liver fibrosis progression in patients with chronic hepatitis C. J Hepatol. 2001;34:730-9.
PubMed Abstract»Ryder SD, Irving WL, Jones DA, Neal KR, Underwood JC; Trent Hepatitis C Study Group. Progression of hepatic fibrosis in patients with hepatitis C: a prospective repeat liver biopsy study. Gut. 2004;53:451-5.
PubMed Abstract»Host Factors that Impact Rate of Fibrosis Progression
Benhamou Y, Bochet M, Di Martino V, et al. Liver fibrosis progression in human immunodeficiency virus and hepatitis C virus coinfected patients. The Multivirc Group. Hepatology. 1999;30:1054-8.
PubMed Abstract»Benvegnu L, Gios M, Boccato S, Alberti A. Natural history of compensated viral cirrhosis: a prospective study on the incidence and hierarchy of major complications. Gut. 2004;53:744-9.
PubMed Abstract»Bochud PY, Cai T, Overbeck K, et al. Genotype 3 is associated with accelerated fibrosis progression in chronic hepatitis C. J Hepatol. 2009;51:655-66.
PubMed Abstract»Carrieri MP, Protopopescu C, Marcellin F, et al. Protective effect of coffee consumption on all-cause mortality of French HIV-HCV co-infected patients. J Hepatol. 2017;67:1157-1167.
PubMed Abstract»Carrieri MP, Serfaty L, Vilotitch A, et al. Cannabis Use and Reduced Risk of Insulin Resistance in HIV-HCV Infected Patients: A Longitudinal Analysis (ANRS CO13 HEPAVIH). Clin Infect Dis. 2015;61:40-8.
PubMed Abstract»Charlton MR, Pockros PJ, Harrison SA. Impact of obesity on treatment of chronic hepatitis C. Hepatology. 2006;43:1177-86.
PubMed Abstract»Chen CM, Yoon YH, Yi HY, Lucas DL. Alcohol and hepatitis C mortality among males and females in the United States: a life table analysis. Alcohol Clin Exp Res. 2007;31:285-92.
PubMed Abstract»Costentin CE, Roudot-Thoraval F, Zafrani ES, Medkour F, Pawlotsky JM, Mallat A, Hézode C. Association of caffeine intake and histological features of chronic hepatitis C. J Hepatol. 2011;54:1123-9.
PubMed Abstract»Desmet VJ, Gerber M, Hoofnagle JH, Manns M, Scheuer PJ. Classification of chronic hepatitis: diagnosis, grading and staging. Hepatology. 1994;19:1513-20.
PubMed Abstract»Di Martino V, Rufat P, Boyer N, et al. The influence of human immunodeficiency virus coinfection on chronic hepatitis C in injection drug users: a long-term retrospective cohort study. Hepatology. 2001;34:1193-9.
PubMed Abstract»Donato F, Tagger A, Gelatti U, et al. Alcohol and hepatocellular carcinoma: the effect of lifetime intake and hepatitis virus infections in men and women. Am J Epidemiol. 2002;155:323-31.
PubMed Abstract»Everhart JE, Lok AS, Kim HY, et al. Weight-related effects on disease progression in the hepatitis C antiviral long-term treatment against cirrhosis trial. Gastroenterology. 2009;137:549-57.
PubMed Abstract»Fartoux L, Chazouillères O, Wendum D, Poupon R, Serfaty L. Impact of steatosis on progression of fibrosis in patients with mild hepatitis C. Hepatology. 2005;41:82-7.
PubMed Abstract»Freedman ND, Everhart JE, Lindsay KL, et al. Coffee intake is associated with lower rates of liver disease progression in chronic hepatitis C. Hepatology. 2009;50:1360-9.
PubMed Abstract»Freeman AJ, Dore GJ, Law MG, et al. Estimating progression to cirrhosis in chronic hepatitis C virus infection. Hepatology. 2001;34:809-16.
PubMed Abstract»Freeman AJ, Law MG, Kaldor JM, Dore GJ. Predicting progression to cirrhosis in chronic hepatitis C virus infection. J Viral Hepat. 2003;10:285-93.
PubMed Abstract»Graham CS, Baden LR, Yu E, Mrus JM, Carnie J, Heeren T, Koziel MJ. Influence of human immunodeficiency virus infection on the course of hepatitis C virus infection: a meta-analysis. Clin Infect Dis. 2001;33:562-9.
PubMed Abstract»Hézode C, Roudot-Thoraval F, Nguyen S, et al. Daily cannabis smoking as a risk factor for progression of fibrosis in chronic hepatitis C. Hepatology. 2005;42:63-71.
PubMed Abstract»Hézode C, Zafrani ES, Roudot-Thoraval F, et al. Daily cannabis use: a novel risk factor of steatosis severity in patients with chronic hepatitis C. Gastroenterology. 2008;134(2):432-9.
PubMed Abstract»Harris HE, Ramsay ME, Andrews N, Eldridge KP. Clinical course of hepatitis C virus during the first decade of infection: cohort study. BMJ. 2002;324:450-3.
PubMed Abstract»Hodge A, Lim S, Goh E, et al. Coffee Intake Is Associated with a Lower Liver Stiffness in Patients with Non-Alcoholic Fatty Liver Disease, Hepatitis C, and Hepatitis B. Nutrients. 2017;9:56.
PubMed Abstract»Hui JM, Sud A, Farrell GC, et al. Insulin resistance is associated with chronic hepatitis C virus infection and fibrosis progression. Gastroenterology. 2003;125:1695-704.
PubMed Abstract»Ingiliz P, Rockstroh JK. Natural history of liver disease and effect of hepatitis C virus on HIV disease progression. Curr Opin HIV AIDS. 2015;10:303-8.
PubMed Abstract»Ishida JH, Peters MG, Jin C, Louie K, Tan V, Bacchetti P, Terrault NA. Influence of cannabis use on severity of hepatitis C disease. Clin Gastroenterol Hepatol. 2008;6:69-75.
PubMed Abstract»Jamma S, Hussain G, Lau DT. Current Concepts of HBV/HCV Coinfection: Coexistence, but Not Necessarily in Harmony. Curr Hepat Rep. 2010;9:260-9.
PubMed Abstract»Kanwal F, Kramer JR, Ilyas J, Duan Z, El-Serag HB. HCV genotype 3 is associated with an increased risk of cirrhosis and hepatocellular cancer in a national sample of U.S. Veterans with HCV. Hepatology. 2014;60:98-105.
PubMed Abstract»Kruse RL, Kramer JR, Tyson GL, et al. Clinical outcomes of hepatitis B virus coinfection in a United States cohort of hepatitis C virus-infected patients. Hepatology. 2014;60:1871-8.
PubMed Abstract»Lingala S, Ghany MG. Natural History of Hepatitis C. Gastroenterol Clin North Am. 2015;44:717-34.
PubMed Abstract»Maasoumy B, Wedemeyer H. Natural history of acute and chronic hepatitis C. Best Pract Res Clin Gastroenterol. 2012;26:401-12.
PubMed Abstract»Marrero JA, Fontana RJ, Fu S, Conjeevaram HS, Su GL, Lok AS. Alcohol, tobacco and obesity are synergistic risk factors for hepatocellular carcinoma. J Hepatol 2005; 42:218-24.
PubMed Abstract»McMahon BJ, Bruden D, Townshend-Bulson L, et al. Infection With Hepatitis C Virus Genotype 3 Is an Independent Risk Factor for End-Stage Liver Disease, Hepatocellular Carcinoma, and Liver-Related Death. Clin Gastroenterol Hepatol. 2017;15:431-437.e2.
PubMed Abstract»Minola E, Prati D, Suter F, et al. Age at infection affects the long-term outcome of transfusion-associated chronic hepatitis C. Blood. 2002;99:4588-91.
PubMed Abstract»Missiha SB, Ostrowski M, Heathcote EJ. Disease progression in chronic hepatitis C: modifiable and nonmodifiable factors. Gastroenterology. 2008;134;1699-714.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Nkontchou G, Ziol M, Aout M, et al. HCV genotype 3 is associated with a higher hepatocellular carcinoma incidence in patients with ongoing viral C cirrhosis. J Viral Hepat. 2011;18:e516-22.
PubMed Abstract»Nordmann S, Vilotitch A, Roux P, et al. Daily cannabis and reduced risk of steatosis in human immunodeficiency virus and hepatitis C virus-co-infected patients (ANRS CO13-HEPAVIH). J Viral Hepat. 2018;25:171-179.
PubMed Abstract»Noureddin M, Wong MM, Todo T, Lu SC, Sanyal AJ, Mena EA. Fatty liver in hepatitis C patients post-sustained virological response with direct-acting antivirals. World J Gastroenterol. 2018;24:1269-1277.
PubMed Abstract»Poynard T, Bedossa P, Opolon P. Lancet. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825-32.
PubMed Abstract»Poynard T, Ratziu V, Charlotte F, Goodman Z, McHutchison J, Albrecht J. Rates and risk factors of liver fibrosis progression in patients with chronic hepatitis C. J Hepatol. 2001;34:730-9.
PubMed Abstract»Pradat P, Voirin N, Tillmann HL, Chevallier M, Trépo C. Progression to cirrhosis in hepatitis C patients: an age-dependent process. Liver Int. 2007;27:335-9.
PubMed Abstract»Serfaty L. Metabolic Manifestations of Hepatitis C Virus: Diabetes Mellitus, Dyslipidemia. Clin Liver Dis. 2017;21:475-486.
PubMed Abstract»Spiegel BM, Younossi ZM, Hays RD, Revicki D, Robbins S, Kanwal F. Impact of hepatitis C on health related quality of life: a systematic review and quantitative assessment. Hepatology. 2005;41:790-800.
PubMed Abstract»Thein HH, Yi Q, Dore GJ, Krahn MD. Natural history of hepatitis C virus infection in HIV-infected individuals and the impact of HIV in the era of highly active antiretroviral therapy: a meta-analysis. AIDS. 2008;22:1979-91.
PubMed Abstract»Thomas DL, Astemborski J, Rai RM, et al. The natural history of hepatitis C virus infection: host, viral, and environmental factors. JAMA 2000;284:450-6.
PubMed Abstract»Thomas DL, Astemborski J, Vlahov D, et al. Determinants of the quantity of hepatitis C virus RNA. J Infect Dis. 2000;181:844-51.
PubMed Abstract»Veldt BJ, Heathcote EJ, Wedemeyer H, et al. Sustained virologic response and clinical outcomes in patients with chronic hepatitis C and advanced fibrosis. Ann Intern Med. 2007;147:677-84.
PubMed Abstract»White DL, Liu Y, Garcia J, et al. Sex hormone pathway gene polymorphisms are associated with risk of advanced hepatitis C-related liver disease in males. Int J Mol Epidemiol Genet. 2014;5:164-76.
PubMed Abstract»White DL, Tavakoli-Tabasi S, Kuzniarek J, Pascua R, Ramsey DJ, El-Serag HB. Higher serum testosterone is associated with increased risk of advanced hepatitis C-related liver disease in males. Hepatology. 2012;55:759-68.
PubMed Abstract»Wiley TE, McCarthy M, Breidi L, McCarthy M, Layden TJ. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology. 1998;28:805-9.
PubMed Abstract»Wu N, Rao HY, Yang WB, et al. Impact of hepatitis C virus genotype 3 on liver disease progression in a Chinese national cohort. Chin Med J (Engl). 2020;133:253-61.
PubMed Abstract»Zarski JP, Bohn B, Bastie A, et al. Characteristics of patients with dual infection by hepatitis B and C viruses. J Hepatol. 1998;28:27-33.
PubMed Abstract»Additional References
Abenavoli L, Masarone M, Peta V, et al. Insulin resistance and liver steatosis in chronic hepatitis C infection genotype 3. World J Gastroenterol. 2014;20:15233-40.
PubMed Abstract»Alter MJ, Kruszon-Moran D, Nainan OV, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999;341:556-62.
PubMed Abstract»Blackard JT, Shata MT, Shire NJ, Sherman KE. Acute hepatitis C virus infection: a chronic problem. Hepatology. 2008;47:321-31.
PubMed Abstract»Chen CM, Yoon YH, Yi HY, Lucas DL. Alcohol and hepatitis C mortality among males and females in the United States: a life table analysis. Alcohol Clin Exp Res. 2007;31:285-92.
PubMed Abstract»Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31-41.
PubMed Abstract»Covic A, Abramowicz D, Bruchfeld A, et al. Endorsement of the Kidney Disease Improving Global Outcomes (KDIGO) hepatitis C guidelines: a European Renal Best Practice (ERBP) position statement. Nephrol Dial Transplant. 2009;24:719-27.
PubMed Abstract»Finelli L, Miller JT, Tokars JI, Alter MJ, Arduino MJ. National surveillance of dialysis-associated diseases in the United States, 2002. Semin Dial. 2005;18:52-61.
PubMed Abstract»Ghany MG, Strader DB, Thomas DL, Seeff LB; American Association for the Study of Liver Diseases. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335-74.
AASLD Practice Guidelines»Gordon CE, Uhlig K, Lau J, Schmid CH, Levey AS, Wong JB. Interferon treatment in hemodialysis patients with chronic hepatitis C virus infection: a systematic review of the literature and meta-analysis of treatment efficacy and harms. Am J Kidney Dis. 2008;51:263-77.
PubMed Abstract»Grebely J, Page K, Sacks-Davis R, et al. The effects of female sex, viral genotype, and IL28B genotype on spontaneous clearance of acute hepatitis C virus infection. Hepatology. 2014;59:109-20.
PubMed Abstract»Huang YW, Yang SS, Fu SC, et al. Increased risk of cirrhosis and its decompensation in chronic hepatitis C patients with new-onset diabetes: a nationwide cohort study. Hepatology. 2014;60:807-14.
PubMed Abstract»Jamma S, Hussain G, Lau DT. Current Concepts of HBV/HCV Coinfection: Coexistence, but Not Necessarily in Harmony. Curr Hepat Rep. 2010;9:260-9.
PubMed Abstract»Kamal SM. Acute hepatitis C: a systematic review. Am J Gastroenterol. 2008;103:1283-97.
PubMed Abstract»Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461-70.
PubMed Abstract»Levey AS, Coresh J, Greene T, et al. Expressing the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem. 2007;53:766-72.
PubMed Abstract»Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247-54.
PubMed Abstract»Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604-12.
PubMed Abstract»Maheshwari A, Ray S, Thuluvath PJ. Acute hepatitis C. Lancet. 2008;372(9635):321-32.
PubMed Abstract»McCombs J, Matsuda T, Tonnu-Mihara I, et al. The risk of long-term morbidity and mortality in patients with chronic hepatitis C: results from an analysis of data from a Department of Veterans Affairs Clinical Registry. JAMA Intern Med. 2014;174:204-12.
PubMed Abstract»Missiha SB, Ostrowski M, Heathcote EJ. Disease progression in chronic hepatitis C: modifiable and nonmodifiable factors. Gastroenterology. 2008;134;1699-714.
PubMed Abstract»Newsum AM, Schinkel J, van de Laar TJW, van der Meer JTM, Prins M. Spontaneous Clearance of Hepatitis C Virus Infection Among Human Immunodeficiency Virus-Infected Men Who Have Sex With Men. Open Forum Infect Dis. 2017;4:ofx090.
PubMed Abstract»Ozkok A, Yildiz A. Hepatitis C virus associated glomerulopathies. World J Gastroenterol. 2014;20:7544-54.
PubMed Abstract»Peters L, Grint D, Lundgren JD, et al. Hepatitis C virus viremia increases the incidence of chronic kidney disease in HIV-infected patients. AIDS. 2012;26:1917-26.
PubMed Abstract»Poynard T, Bedossa P, Opolon P. Lancet. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825-32.
PubMed Abstract»Poynard T, Ratziu V, Charlotte F, Goodman Z, McHutchison J, Albrecht J. Rates and risk factors of liver fibrosis progression in patients with chronic hepatitis C. J Hepatol. 2001;34:730-9.
PubMed Abstract»Ragonnet R, Deuffic-Burban S, Boesecke C, et al. Estimating the Time to Diagnosis and the Chance of Spontaneous Clearance During Acute Hepatitis C in Human Immunodeficiency Virus-Infected Individuals. Open Forum Infect Dis. 2017;4:ofw235.
PubMed Abstract»Shoker A, Hossain MA, Koru-Sengul T, Raju DL, Cockcroft D. Performance of creatinine clearance equations on the original Cockcroft-Gault population. Clin Nephrol. 2006;66:89-97.
PubMed Abstract»Smith DJ, Jordan AE, Frank M, Hagan H. Spontaneous viral clearance of hepatitis C virus (HCV) infection among people who inject drugs (PWID) and HIV-positive men who have sex with men (HIV+ MSM): a systematic review and meta-analysis. BMC Infect Dis. 2016;16:471.
PubMed Abstract»Thomas DL, Astemborski J, Rai RM, et al. The natural history of hepatitis C virus infection: host, viral, and environmental factors. JAMA 2000;284:450-6.
PubMed Abstract»Thomas DL, Thio CL, Martin MP, et al. Genetic variation in IL28B and spontaneous clearance of hepatitis C virus. Nature. 2009;461:798-801.
PubMed Abstract»Tsui JI, Vittinghoff E, Shlipak MG, Bertenthal D, Inadomi J, Rodriguez RA, O'Hare AM. Association of hepatitis C seropositivity with increased risk for developing end-stage renal disease. Arch Intern Med. 2007;167:1271-6.
PubMed Abstract»Westbrook RH, Dusheiko G. Natural history of hepatitis C. J Hepatol. 2014;61:S58-68.
PubMed Abstract»Wiley TE, McCarthy M, Breidi L, McCarthy M, Layden TJ. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology. 1998;28:805-9.
PubMed Abstract»Winter MA, Guhr KN, Berg GM. Impact of various body weights and serum creatinine concentrations on the bias and accuracy of the Cockcroft-Gault equation. Pharmacotherapy. 2012;32:604-12.
PubMed Abstract»Wirth TC, Manns MP. The impact of the revolution in hepatitis C treatment on hepatocellular carcinoma. Ann Oncol. 2016;27:1467-74.
PubMed Abstract»Lesson 3. Counseling Persons with Chronic HCV Infection
Over-the-Counter Pain Medications
Backstedt D, Pedersen M, Choi M, Seetharam A. 25-Vitamin D levels in chronic hepatitis C infection: association with cirrhosis and sustained virologic response. Ann Gastroenterol. 2017;30:344-348.
PubMed Abstract»Bauerlein DK, Williams AP, John PR. Optimizing Acetaminophen Use in Patients with Risk Factors for Hepatotoxicity: Reviewing Dosing Recommendations in Adults. Pain Med. 2021;22:1469-72.
PubMed Abstract»Bitetto D, Fattovich G, Fabris C, et al. Complementary role of vitamin D deficiency and the interleukin-28B rs12979860 C/T polymorphism in predicting antiviral response in chronic hepatitis C. Hepatology. 2011;53:1118-26.
PubMed Abstract»Bosilkovska M, Walder B, Besson M, Daali Y, Desmeules J. Analgesics in patients with hepatic impairment: pharmacology and clinical implications. Drugs. 2012;72:1645-69.
PubMed Abstract»Chandok N, Watt KD. Pain management in the cirrhotic patient: the clinical challenge. Mayo Clin Proc. 2010;85:451-8.
PubMed Abstract»D'Souza RF, Feakins R, Mears L, Sabin CA, Foster GR. Relationship between serum ferritin, hepatic iron staining, diabetes mellitus and fibrosis progression in patients with chronic hepatitis C. Aliment Pharmacol Ther. 2005;21:519-24.
PubMed Abstract»Dawson-Hughes B, Mithal A, Bonjour JP, et al. IOF position statement: vitamin D recommendations for older adults. Osteoporos Int. 2010;21:1151-4.
PubMed Abstract»de Pee S, Dary O. Biochemical indicators of vitamin A deficiency: serum retinol and serum retinol binding protein. J Nutr. 2002;132:2895S-2901S.
PubMed Abstract»Dwyer JP, Jayasekera C, Nicoll A. Analgesia for the cirrhotic patient: a literature review and recommendations. J Gastroenterol Hepatol. 2014;29:1356-60.
PubMed Abstract»Fallon MB, Boyer JL. Hepatic toxicity of vitamin A and synthetic retinoids. J Gastroenterol Hepatol. 1990;5:334-42.
PubMed Abstract»García-Álvarez M, Pineda-Tenor D, Jiménez-Sousa MA, Fernández-Rodríguez A, Guzmán-Fulgencio M, Resino S. Relationship of vitamin D status with advanced liver fibrosis and response to hepatitis C virus therapy: A meta-analysis. Hepatology. 2014;60:1541-50.
PubMed Abstract»Gutierrez JA, Parikh N, Branch AD. Classical and emerging roles of vitamin D in hepatitis C virus infection. Semin Liver Dis. 2011;31:387-98.
PubMed Abstract»Hézode C, Cazeneuve C, Coué O, et al. Liver iron accumulation in patients with chronic active hepatitis C: prevalence and role of hemochromatosis gene mutations and relationship with hepatic histological lesions. J Hepatol. 1999;31:979-84.
PubMed Abstract»Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-30.
PubMed Abstract»Institute of Medicine of the National Academies. Report at a Glance, Report Brief: Dietary Feference Intakes for Calcium and Vitamin D. November 2010.
Institute of Medicine»Ioannides SJ, Siebers R, Perrin K, et al. The effect of 1g of acetaminophen twice daily for 12 weeks on alanine transaminase levels--A randomized placebo-controlled trial. Clin Biochem. 2015;48:713-5.
PubMed Abstract»Khandelwal N, James LP, Sanders C, Larson AM, Lee WM; Acute Liver Failure Study Group. Unrecognized acetaminophen toxicity as a cause of indeterminate acute liver failure. Hepatology. 2011;53:567-76.
PubMed Abstract»Kitson MT, Dore GJ, George J, et al. Vitamin D status does not predict sustained virologic response or fibrosis stage in chronic hepatitis C genotype 1 infection. J Hepatol. 2013;58:467-72.
PubMed Abstract»Kowalski TE, Falestiny M, Furth E, Malet PF. Vitamin A hepatotoxicity: a cautionary note regarding 25,000 IU supplements. Am J Med. 1994;97:523-8.
PubMed Abstract»Larson AM, Polson J, Fontana RJ, Davern TJ, Lalani E, Hynan LS, Reisch JS, Schiødt FV, Ostapowicz G, Shakil AO, Lee WM; Acute Liver Failure Study Group. Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology. 2005; 42:1364-72.
PubMed Abstract»Mandorfer M, Reiberger T, Payer BA, et al. Low vitamin D levels are associated with impaired virologic response to PEGIFN + RBV therapy in HIV-hepatitis C virus coinfected patients. AIDS. 2013;27:227-32.
PubMed Abstract»Martineau AR. Vitamin D: An adjunct to antiretroviral therapy? J Infect Dis. 2013;207:373-5.
PubMed Abstract»Metwally MA, Zein CO, Zein NN. Clinical significance of hepatic iron deposition and serum iron values in patients with chronic hepatitis C infection. Am J Gastroenterol. 2004;99:286-91.
PubMed Abstract»Minuk GY, Kelly JK, Hwang WS. Vitamin A hepatotoxicity in multiple family members. Hepatology. 1988;8:272-5.
PubMed Abstract»Myers RP, Shaheen AA, Li B, Dean S, Quan H. Impact of liver disease, alcohol abuse, and unintentional ingestions on the outcomes of acetaminophen overdose. Clin Gastroenterol Hepatol. 2008;6:918-25.
PubMed Abstract»Nguyen GC, Sam J, Thuluvath PJ. Hepatitis C is a predictor of acute liver injury among hospitalizations for acetaminophen overdose in the United States: a nationwide analysis. Hepatology. 2008;48:1336-41.
PubMed Abstract»Petta S, Cammà C, Scazzone C, et al. Low vitamin D serum level is related to severe fibrosis and low responsiveness to interferon-based therapy in genotype 1 chronic hepatitis C. Hepatology. 2010;51:1158-67.
PubMed Abstract»Piperno A, Vergani A, Malosio I, et al. Hepatic iron overload in patients with chronic viral hepatitis: role of HFE gene mutations. Hepatology. 1998;28:1105-9.
PubMed Abstract»Rahman AH, Branch AD. Vitamin D for your patients with chronic hepatitis C? J Hepatol. 2013;58:184-9.
PubMed Abstract»Rakoski M, Goyal P, Spencer-Safier M, Weissman J, Mohr G, Volk M. Pain management in patients with cirrhosis. Clin Liver Dis (Hoboken). 2018;11:135-140.
PubMed Abstract»Recommendations abstracted from the American Geriatrics Society Consensus Statement on vitamin D for Prevention of Falls and Their Consequences. J Am Geriatr Soc. 2014;62:147-52.
PubMed Abstract»Riggio O, Montagnese F, Fiore P, et al. Iron overload in patients with chronic viral hepatitis: how common is it? Am J Gastroenterol. 1997;92:1298-1301.
PubMed Abstract»Riley TR 3rd, Smith JP. Ibuprofen-induced hepatotoxicity in patients with chronic hepatitis C: a case series. Am J Gastroenterol. 1998;93:1563-5.
PubMed Abstract»Riley TR, Smith JP. Preventive care in chronic liver disease. J Gen Intern Med. 1999;14:699-704.
PubMed Abstract»Risser A, Donovan D, Heintzman J, Page T. NSAID prescribing precautions. Am Fam Physician. 2009;80:1371-8.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Stokes CS, Volmer DA, Grünhage F, Lammert F. Vitamin D in chronic liver disease. Liver Int. 2013; 33:338-52.
PubMed Abstract»Terrier B, Lapidus N, Pol S, et al. Vitamin D in addition to peg-interferon-alpha/ribavirin in chronic hepatitis C virus infection: ANRS-HC25-VITAVIC study. World J Gastroenterol. 2015;21:5647-53.
PubMed Abstract»Watkins PB, Kaplowitz N, Slattery JT, Colonese CR, Colucci SV, Stewart PW, Harris SC. Aminotransferase elevations in healthy adults receiving 4 grams of acetaminophen daily: a randomized controlled trial. JAMA. 2006; 296:87-93.
PubMed Abstract»Weber FL Jr, Mitchell GE Jr, Powell DE, Reiser BJ, Banwell JG. Reversible hepatotoxicity associated with hepatic vitamin A accumulation in a protein-deficient patient. Gastroenterology. 1982;82:118-23.
PubMed Abstract»Wohlrab P, Boehme S, Kaun C, et al. Ropivacaine Activates Multiple Proapoptotic and Inflammatory Signaling Pathways That Might Subsume to Trigger Epidural-Related Maternal Fever. Anesth Analg. 2020;130:321-31.
PubMed Abstract»Iron and Vitamin Supplements
Backstedt D, Pedersen M, Choi M, Seetharam A. 25-Vitamin D levels in chronic hepatitis C infection: association with cirrhosis and sustained virologic response. Ann Gastroenterol. 2017;30:344-348.
PubMed Abstract»Bitetto D, Fattovich G, Fabris C, et al. Complementary role of vitamin D deficiency and the interleukin-28B rs12979860 C/T polymorphism in predicting antiviral response in chronic hepatitis C. Hepatology. 2011;53:1118-26.
PubMed Abstract»Bjelakovic M, Nikolova D, Bjelakovic G, Gluud C. Vitamin D supplementation for chronic liver diseases in adults. Cochrane Database Syst Rev. 2021;8:CD011564.
PubMed Abstract»D'Souza RF, Feakins R, Mears L, Sabin CA, Foster GR. Relationship between serum ferritin, hepatic iron staining, diabetes mellitus and fibrosis progression in patients with chronic hepatitis C. Aliment Pharmacol Ther. 2005;21:519-24.
PubMed Abstract»Dawson-Hughes B, Mithal A, Bonjour JP, et al. IOF position statement: vitamin D recommendations for older adults. Osteoporos Int. 2010;21:1151-4.
PubMed Abstract»de Pee S, Dary O. Biochemical indicators of vitamin A deficiency: serum retinol and serum retinol binding protein. J Nutr. 2002;132:2895S-2901S.
PubMed Abstract»Fallon MB, Boyer JL. Hepatic toxicity of vitamin A and synthetic retinoids. J Gastroenterol Hepatol. 1990;5:334-42.
PubMed Abstract»García-Álvarez M, Pineda-Tenor D, Jiménez-Sousa MA, Fernández-Rodríguez A, Guzmán-Fulgencio M, Resino S. Relationship of vitamin D status with advanced liver fibrosis and response to hepatitis C virus therapy: A meta-analysis. Hepatology. 2014;60:1541-50.
PubMed Abstract»Gutierrez JA, Parikh N, Branch AD. Classical and emerging roles of vitamin D in hepatitis C virus infection. Semin Liver Dis. 2011;31:387-98.
PubMed Abstract»Hézode C, Cazeneuve C, Coué O, et al. Liver iron accumulation in patients with chronic active hepatitis C: prevalence and role of hemochromatosis gene mutations and relationship with hepatic histological lesions. J Hepatol. 1999;31:979-84.
PubMed Abstract»Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-30.
PubMed Abstract»Institute of Medicine of the National Academies. Report at a Glance, Report Brief: Dietary Feference Intakes for Calcium and Vitamin D. November 2010.
Institute of Medicine»Kitson MT, Dore GJ, George J, et al. Vitamin D status does not predict sustained virologic response or fibrosis stage in chronic hepatitis C genotype 1 infection. J Hepatol. 2013;58:467-72.
PubMed Abstract»Kowalski TE, Falestiny M, Furth E, Malet PF. Vitamin A hepatotoxicity: a cautionary note regarding 25,000 IU supplements. Am J Med. 1994;97:523-8.
PubMed Abstract»Mandorfer M, Reiberger T, Payer BA, et al. Low vitamin D levels are associated with impaired virologic response to PEGIFN + RBV therapy in HIV-hepatitis C virus coinfected patients. AIDS. 2013;27:227-32.
PubMed Abstract»Martín-González C, Pelazas-González R, Fernández-Rodríguez C, et al. Ferritin and liver fibrosis among patients with chronic hepatitis C virus infection. J Trace Elem Med Biol. 2020;61:126542.
PubMed Abstract»Metwally MA, Zein CO, Zein NN. Clinical significance of hepatic iron deposition and serum iron values in patients with chronic hepatitis C infection. Am J Gastroenterol. 2004;99:286-91.
PubMed Abstract»Minuk GY, Kelly JK, Hwang WS. Vitamin A hepatotoxicity in multiple family members. Hepatology. 1988;8:272-5.
PubMed Abstract»Petta S, Cammà C, Scazzone C, et al. Low vitamin D serum level is related to severe fibrosis and low responsiveness to interferon-based therapy in genotype 1 chronic hepatitis C. Hepatology. 2010;51:1158-67.
PubMed Abstract»Piperno A, Vergani A, Malosio I, et al. Hepatic iron overload in patients with chronic viral hepatitis: role of HFE gene mutations. Hepatology. 1998;28:1105-9.
PubMed Abstract»Rahman AH, Branch AD. Vitamin D for your patients with chronic hepatitis C? J Hepatol. 2013;58:184-9.
PubMed Abstract»Recommendations abstracted from the American Geriatrics Society Consensus Statement on vitamin D for Prevention of Falls and Their Consequences. J Am Geriatr Soc. 2014;62:147-52.
PubMed Abstract»Riggio O, Montagnese F, Fiore P, et al. Iron overload in patients with chronic viral hepatitis: how common is it? Am J Gastroenterol. 1997;92:1298-1301.
PubMed Abstract»Riley TR, Smith JP. Preventive care in chronic liver disease. J Gen Intern Med. 1999;14:699-704.
PubMed Abstract»Stokes CS, Volmer DA, Grünhage F, Lammert F. Vitamin D in chronic liver disease. Liver Int. 2013; 33:338-52.
PubMed Abstract»Terrier B, Lapidus N, Pol S, et al. Vitamin D in addition to peg-interferon-alpha/ribavirin in chronic hepatitis C virus infection: ANRS-HC25-VITAVIC study. World J Gastroenterol. 2015;21:5647-53.
PubMed Abstract»Weber FL Jr, Mitchell GE Jr, Powell DE, Reiser BJ, Banwell JG. Reversible hepatotoxicity associated with hepatic vitamin A accumulation in a protein-deficient patient. Gastroenterology. 1982;82:118-23.
PubMed Abstract»Complementary and Alternative Therapies
Andreone P, Gramenzi A, Cursaro C, et al. Thymosin-alpha 1 plus interferon-alpha for naive patients with chronic hepatitis C: results of a randomized controlled pilot trial. J Viral Hepat. 2004;11:69-73.
PubMed Abstract»Anstee QM, Day CP. S-adenosylmethionine (SAMe) therapy in liver disease: A review of current evidence and clinical utility. J Hepatol 2012; 57:1097-1109.
PubMed Abstract»Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004:1-19.
PubMed Abstract»Bottiglieri T. S-Adenosyl-L-methionine (SAMe): from the bench to the bedside--molecular basis of a pleiotrophic molecule. Am J Clin Nutr. 2002;76:1151S-7S.
PubMed Abstract»Chrubasik-Hausmann S, Vlachojannis J, McLachlan AJ. Understanding drug interactions with St John's wort (Hypericum perforatum L.): impact of hyperforin content. J Pharm Pharmacol. 2019;71:129-38.
PubMed Abstract»Coon JT, Ernst E. Complementary and alternative therapies in the treatment of chronic hepatitis C: a systematic review. J Hepatol. 2004;40:491-500.
PubMed Abstract»Feld JJ, Modi AA, El-Diwany R, et al. S-adenosyl methionine improves early viral responses and interferon-stimulated gene induction in hepatitis C nonresponders. Gastroenterology. 2011;140:830-9.
PubMed Abstract»Filipowicz M, Bernsmeier C, Terracciano L, Duong FH, Heim MH. S-adenosyl-methionine and betaine improve early virological response in chronic hepatitis C patients with previous nonresponse. PLoS One. 2010;5:e15492.
PubMed Abstract»Fiore C, Eisenhut M, Krausse R, Ragazzi E, Pellati D, Armanini D, Bielenberg J.
Antiviral effects of Glycyrrhiza species. Phytother Res. 2008;22:141-8.
PubMed Abstract»Fried MW, Navarro VJ, Afdhal N, et al. Effect of silymarin (milk thistle) on liver disease in patients with chronic hepatitis C unsuccessfully treated with interferon therapy: a randomized controlled trial. JAMA. 2012;308:274-82.
PubMed Abstract»Gerards MC, Terlou RJ, Yu H, Koks CH, Gerdes VE. Traditional Chinese lipid-lowering agent red yeast rice results in significant LDL reduction but safety is uncertain - a systematic review and meta-analysis. Atherosclerosis. 2015;240:415-23.
PubMed Abstract»Ginseng. In: LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012. [Last Updated Mar 14, 2018].
LiverTox»Goldstein AL, Goldstein AL. From lab to bedside: emerging clinical applications of thymosin alpha 1. Expert Opin Biol Ther. 2009;9:593-608.
PubMed Abstract»Hawke RL, Schrieber SJ, Soule TA, et al. Silymarin ascending multiple oral dosing phase I study in noncirrhotic patients with chronic hepatitis C. J Clin Pharmacol. 2010;50:434-49.
PubMed Abstract»Hirayama C, Okumura M, Tanikawa K, Yano M, Mizuta M, Ogawa N. A multicenter randomized controlled clinical trial of Shosaiko-to in chronic active hepatitis. Gastroenterol Jpn. 1989;24:715-9.
PubMed Abstract»Hypericum Depression Trial Study Group. Effect of Hypericum perforatum (St John's wort) in major depressive disorder: a randomized controlled trial. JAMA. 2002;287:1807-14.
PubMed Abstract»Ishibashi Y, Takeda K, Tsukidate N, Miyazaki H, Ohira K, Dosaka-Akita H, Nishimura M. Randomized placebo-controlled trial of interferon alpha-2b plus ribavirin with and without lactoferrin for chronic hepatitis C. Hepatol Res. 2005;32:218-23.
PubMed Abstract»Itoh S, Marutani K, Nishijima T, Matsuo S, Itabashi M. Liver injuries induced by herbal medicine, syo-saiko-to (xiao-chai-hu-tang). Dig Dis Sci. 1995;40:1845-8.
PubMed Abstract»Jacobson JM, Feinman L, Liebes L, et al. Pharmacokinetics, safety, and antiviral effects of hypericin, a derivative of St. John's wort plant, in patients with chronic hepatitis C virus infection. Antimicrob Agents Chemother. 2001;45:517-24.
PubMed Abstract»Kamiyama T, Nouchi T, Kojima S, Murata N, Ikeda T, Sato C. Autoimmune hepatitis triggered by administration of an herbal medicine. Am J Gastroenterol. 1997;92:703-4.
PubMed Abstract»Licorice. In: LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012. [Last Updated March 20, 2023].
LiverTox»LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012.
LiverTox»Marzio DL, Fenkel JM. Complementary and alternative medications in hepatitis C infection. World J Hepatol. 2014;6:9-16.
PubMed Abstract»Matsuda R, Takahashi D, Chiba E, et al. [A case of drug induced hepatitis and interstitial pneumonia caused by a herbal drug, Dai-saiko-to]. Nihon Shokakibyo Gakkai Zasshi. 1997;94:787-91.
PubMed Abstract»Matsumoto Y, Matsuura T, Aoyagi H, et al. Antiviral activity of glycyrrhizin against hepatitis C virus in vitro. PLoS One. 2013;8:e68992.
PubMed Abstract»Milk Thistle. In: LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012. [Last Updated January 21, 2020].
LiverTox»Mora SI, García-Román J, Gómez-Ñañez I, García-Román R. Chronic liver diseases and the potential use of S-adenosyl-L-methionine as a hepatoprotector. Eur J Gastroenterol Hepatol. 2018;30:893-900.
PubMed Abstract»Oka H, Yamamoto S, Kuroki T, et al. Prospective study of chemoprevention of hepatocellular carcinoma with Sho-saiko-to (TJ-9). Cancer. 1995;76:743-9.
PubMed Abstract»Okada S, Tanaka K, Sato T, et al. Dose-response trial of lactoferrin in patients with chronic hepatitis C. Jpn J Cancer Res. 2002;93:1063-9.
PubMed Abstract»Ottenbacher R, Blehm J. An Unusual Case of Licorice-Induced Hypertensive Crisis. S D Med. 2015;68:346-7, 349.
PubMed Abstract»Parés A, Planas R, Torres M, et al. Effects of silymarin in alcoholic patients with cirrhosis of the liver: results of a controlled, double-blind, randomized and multicenter trial. J Hepatol. 1998;28:615-21.
PubMed Abstract»Park TY, Hong M, Sung H, Kim S, Suk KT. Effect of Korean Red Ginseng in chronic liver disease. J Ginseng Res. 2017;41:450-455.
PubMed Abstract»Picard-Jean F, Bouchard S, Larivée G, Bisaillon M. The intracellular inhibition of HCV replication represents a novel mechanism of action by the innate immune Lactoferrin protein. Antiviral Res. 2014;111:13-22.
PubMed Abstract»Polyak S, Ferenci P, Pawlotsky JM. Hepatoprotective and antiviral functions of silymarin components in hepatitis C virus infection. Hepatology. 2013;57:1262-71.
PubMed Abstract»Polyak SJ, Oberlies NH, Pécheur EI, Dahari H, Ferenci P, Pawlotsky JM. Silymarin for HCV infection. Antivir Ther. 2013;18:141-7.
PubMed Abstract»Raymond RS, Fallon MB, Abrams GA. Oral thymic extract for chronic hepatitis C in patients previously treated with interferon. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1998;129:797-800.
PubMed Abstract»Red Yeast Rice. In: LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012. [Last Updated March 20, 2023].
LiverTox»Redwan el-RM, Tabll A. Camel lactoferrin markedly inhibits hepatitis C virus genotype 4 infection of human peripheral blood leukocytes. J Immunoassay Immunochem. 2007;28:267-77.
PubMed Abstract»Seeff LB, Curto TM, Szabo G, et al. Herbal product use by persons enrolled in the hepatitis C Antiviral Long-Term Treatment Against Cirrhosis (HALT-C) Trial. Hepatology. 2008;47:605-12.
PubMed Abstract»Sherman KE, Sjogren M, Creager RL, et al. Combination therapy with thymosin alpha1 and interferon for the treatment of chronic hepatitis C infection: a randomized, placebo-controlled double-blind trial. Hepatology. 1998;27:1128-35.
PubMed Abstract»Sherman KE. Thymosin alpha 1 for treatment of hepatitis C virus: promise and proof. Ann N Y Acad Sci. 2010;1194:136-40.
PubMed Abstract»Shimizu I. Sho-saiko-to: Japanese herbal medicine for protection against hepatic fibrosis and carcinoma. J Gastroenterol Hepatol. 2000;15 Suppl:D84-90.
PubMed Abstract»Sho Saiko To and Dai Saiko To. In: LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012. Last Update Aug 15, 2020.
LiverTox»Sinopoli A, Isonne C, Santoro MM, Baccolini V. The effects of orally administered lactoferrin in the prevention and management of viral infections: A systematic review. Rev Med Virol. 2022;32:e2261.
PubMed Abstract»Soleymani S, Bahramsoltani R, Rahimi R, Abdollahi M. Clinical risks of St John's Wort (Hypericum perforatum) co-administration. Expert Opin Drug Metab Toxicol. 2017;13:1047-62.
PubMed Abstract»St. John's Wort. In: LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012. [Last Updated March 28, 2020].
LiverTox»Tanaka K, Ikeda M, Nozaki A, et al. Lactoferrin inhibits hepatitis C virus viremia in patients with chronic hepatitis C: a pilot study. Jpn J Cancer Res. 1999;90:367-71.
PubMed Abstract»Ueno H, Sato T, Yamamoto S, et al. Randomized, double-blind, placebo-controlled trial of bovine lactoferrin in patients with chronic hepatitis C. Cancer Sci. 2006;97:1105-10.
PubMed Abstract»Venkataramanan R, Ramachandran V, Komoroski BJ, Zhang S, Schiff PL, Strom SC. Milk thistle, a herbal supplement, decreases the activity of CYP3A4 and uridine diphosphoglucuronosyl transferase in human hepatocyte cultures. Drug Metab Dispos. 2000;28:1270-3.
PubMed Abstract»Verhoeven V, Lopez Hartmann M, Remmen R, Wens J, Apers S, Van Royen P. Red yeast rice lowers cholesterol in physicians - a double blind, placebo controlled randomized trial. BMC Complement Altern Med. 2013;13:178.
PubMed Abstract»Yang Z, Zhuang L, Lu Y, Xu Q, Chen X. Effects and tolerance of silymarin (milk thistle) in chronic hepatitis C virus infection patients: a meta-analysis of randomized controlled trials. Biomed Res Int. 2014;2014:941085.
PubMed Abstract»Coffee, Diet, and Sodium Intake
Adinolfi LE, Gambardella M, Andreana A, Tripodi MF, Utili R, Ruggiero G. Steatosis accelerates the liver damage of chronic hepatitis C patients and correlates with specific genotypes and visceral adiposity. Hepatology. 2001;33:1358-64.
PubMed Abstract»Andreone P, Gramenzi A, Cursaro C, et al. Thymosin-alpha 1 plus interferon-alpha for naive patients with chronic hepatitis C: results of a randomized controlled pilot trial. J Viral Hepat. 2004;11:69-73.
PubMed Abstract»Bressler BL, Guindi M, Tomlinson G, Heathcote J. High body mass index Is an independent risk factor for nonresponse to antiviral treatment in chronic hepatitis C. Hepatology. 2003;38:639-44.
PubMed Abstract»Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592-609.
PubMed Abstract»Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328-57.
PubMed Abstract»Eslam M, Aparcero R, Kawaguchi T, Del Campo JA, Sata M, Khattab MA, Romero-Gomez M. Meta-analysis: insulin resistance and sustained virological response in hepatitis C. Aliment Pharmacol Ther. 2011;34:297-305.
PubMed Abstract»European Association for the Study of the Liver.. EASL Clinical Practice Guidelines on nutrition in chronic liver disease. J Hepatol. 2019;70:172-93.
PubMed Abstract»Freedman ND, Curto TM, Lindsay KL, Wright EC, Sinha R, Everhart JE; HALT-C TRIAL GROUP. Coffee consumption is associated with response to peginterferon and ribavirin therapy in patients with chronic hepatitis C. Gastroenterology. 2011;140:1961-9.
PubMed Abstract»Freedman ND, Everhart JE, Lindsay KL, et al. Coffee intake is associated with lower rates of liver disease progression in chronic hepatitis C. Hepatology. 2009;50:1360-9.
PubMed Abstract»Fried MW, Shiffman ML, Reddy KR, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med. 2002;347:975-82.
PubMed Abstract»Goldstein AL, Goldstein AL. From lab to bedside: emerging clinical applications of thymosin alpha 1. Expert Opin Biol Ther. 2009;9:593-608.
PubMed Abstract»Heymsfield SB, Wadden TA. Mechanisms, Pathophysiology, and Management of Obesity. N Engl J Med. 2017;376:254-266.
PubMed Abstract»Hodge A, Lim S, Goh E, et al. Coffee Intake Is Associated with a Lower Liver Stiffness in Patients with Non-Alcoholic Fatty Liver Disease, Hepatitis C, and Hepatitis B. Nutrients. 2017;9:56.
PubMed Abstract»Iqbal U, Jadeja RN, Khara HS, Khurana S. A Comprehensive Review Evaluating the Impact of Protein Source (Vegetarian vs. Meat Based) in Hepatic Encephalopathy. Nutrients. 2021;13:370.
PubMed Abstract»Jaruvongvanich V, Sanguankeo A, Klomjit N, Upala S. Effects of caffeine consumption in patients with chronic hepatitis C: A systematic review and meta-analysis. Clin Res Hepatol Gastroenterol. 2017 Feb;41:46-55.
PubMed Abstract»Khalaf N, White D, Kanwal F, et al. Coffee and Caffeine Are Associated With Decreased Risk of Advanced Hepatic Fibrosis Among Patients With Hepatitis C. Clin Gastroenterol Hepatol. 2015;13:1521-31.e3.
PubMed Abstract»Liu F, Wang X, Wu G, et al. Coffee Consumption Decreases Risks for Hepatic Fibrosis and Cirrhosis: A Meta-Analysis. PLoS One. 2015;10:e0142457.
PubMed Abstract»Milke García MP. Nutritional support in the treatment of chronic hepatic encephalopathy. Ann Hepatol. 2011;10 Suppl 2:S45-9.
PubMed Abstract»Pattullo V, Duarte-Rojo A, Soliman W, V, et al. A 24-week dietary and physical activity lifestyle intervention reduces hepatic insulin resistance in the obese with chronic hepatitis C. Liver Int. 2013;33:410-9.
PubMed Abstract»Pekow JR, Bhan AK, Zheng H, Chung RT. Hepatic steatosis is associated with increased frequency of hepatocellular carcinoma in patients with hepatitis C-related cirrhosis. Cancer. 2007;109:2490-6.
PubMed Abstract»Ramírez MJ, Titos E, Clària J, Navasa M, Fernández J, Rodés J. Increased apoptosis dependent on caspase-3 activity in polymorphonuclear leukocytes from patients with cirrhosis and ascites. J Hepatol. 2004;41:44-8.
PubMed Abstract»Raymond RS, Fallon MB, Abrams GA. Oral thymic extract for chronic hepatitis C in patients previously treated with interferon. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1998;129:797-800.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Setiawan VW, Wilkens LR, Lu SC, Hernandez BY, Le Marchand L, Henderson BE. Association of coffee intake with reduced incidence of liver cancer and death from chronic liver disease in the US multiethnic cohort. Gastroenterology. 2015;148:118-25; quiz e15.
PubMed Abstract»Sherman KE, Sjogren M, Creager RL, et al. Combination therapy with thymosin alpha1 and interferon for the treatment of chronic hepatitis C infection: a randomized, placebo-controlled double-blind trial. Hepatology. 1998;27:1128-35.
PubMed Abstract»Sherman KE. Thymosin alpha 1 for treatment of hepatitis C virus: promise and proof. Ann N Y Acad Sci. 2010;1194:136-40.
PubMed Abstract»Thomopoulos KC, Theocharis GJ, Tsamantas AC, et al. Liver steatosis is an independent risk factor for treatment failure in patients with chronic hepatitis C. Eur J Gastroenterol Hepatol. 2005;17:149-53.
PubMed Abstract»Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60:715-35.
PubMed Abstract»Modifying Obesity
Adinolfi LE, Gambardella M, Andreana A, Tripodi MF, Utili R, Ruggiero G. Steatosis accelerates the liver damage of chronic hepatitis C patients and correlates with specific genotypes and visceral adiposity. Hepatology. 2001;33:1358-64.
PubMed Abstract»Bressler BL, Guindi M, Tomlinson G, Heathcote J. High body mass index Is an independent risk factor for nonresponse to antiviral treatment in chronic hepatitis C. Hepatology. 2003;38:639-44.
PubMed Abstract»Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328-57.
PubMed Abstract»Diehl AM, Day C. Cause, Pathogenesis, and Treatment of Nonalcoholic Steatohepatitis. N Engl J Med. 2017;377:2063-2072.
PubMed Abstract»Eslam M, Aparcero R, Kawaguchi T, Del Campo JA, Sata M, Khattab MA, Romero-Gomez M. Meta-analysis: insulin resistance and sustained virological response in hepatitis C. Aliment Pharmacol Ther. 2011;34:297-305.
PubMed Abstract»Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73:202-9.
PubMed Abstract»Fox DS, McGinnis JJ, Tonnu-Mihara IQ, McCombs JS. Comparative treatment effectiveness of direct acting antiviral regimens for hepatitis C: Data from the Veterans administration. J Gastroenterol Hepatol. 2017;32:1136-1142.
PubMed Abstract»Heymsfield SB, Wadden TA. Mechanisms, Pathophysiology, and Management of Obesity. N Engl J Med. 2017;376:254-266.
PubMed Abstract»Kim MN, Han K, Yoo J, Hwang SG, Ahn SH. Increased risk of hepatocellular carcinoma and mortality in chronic viral hepatitis with concurrent fatty liver. Aliment Pharmacol Ther. 2022;55:97-107.
PubMed Abstract»Kim MN, Han K, Yoo J, Hwang SG, Zhang X, Ahn SH. Diabetic MAFLD is associated with increased risk of hepatocellular carcinoma and mortality in chronic viral hepatitis patients. Int J Cancer. 2023;153:1448-58.
PubMed Abstract»Pekow JR, Bhan AK, Zheng H, Chung RT. Hepatic steatosis is associated with increased frequency of hepatocellular carcinoma in patients with hepatitis C-related cirrhosis. Cancer. 2007;109:2490-6.
PubMed Abstract»Phoolchund AGS, Khakoo SI. MASLD and the Development of HCC: Pathogenesis and Therapeutic Challenges. Cancers (Basel). 2024;16:259.
PubMed Abstract»Rinella ME, Lazarus JV, Ratziu V, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol. 2023;79:1542-56.
PubMed Abstract»Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015;313:2263-73.
PubMed Abstract»Thomopoulos KC, Theocharis GJ, Tsamantas AC, et al. Liver steatosis is an independent risk factor for treatment failure in patients with chronic hepatitis C. Eur J Gastroenterol Hepatol. 2005;17:149-53.
PubMed Abstract»Wang T, Xi Y, Raji A, et al. Overall and subgroup prevalence of non-alcoholic fatty liver disease and prevalence of advanced fibrosis in the United States: An updated national estimate in National Health and Nutrition Examination Survey (NHANES) 2011-2018. Ann Hepatol. 2024;29:101154.
PubMed Abstract»Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11-20.
PubMed Abstract»Alcohol, Cannabis, and Tobacco
Abdel-Rahman O, Helbling D, Schöb O, et al. Cigarette smoking as a risk factor for the development of and mortality from hepatocellular carcinoma: An updated systematic review of 81 epidemiological studies. J Evid Based Med. 2017;10:245-254.
PubMed Abstract»Anand BS, Currie S, Dieperink E, et al. Alcohol use and treatment of hepatitis C virus: results of a national multicenter study. Gastroenterology. 2006;130:1607-16.
PubMed Abstract»Bruggmann P, Dampz M, Gerlach T, Kravecz L, Falcato L. Treatment outcome in relation to alcohol consumption during hepatitis C therapy: an analysis of the Swiss Hepatitis C Cohort Study. Drug Alcohol Depend. 2010;110:167-71.
PubMed Abstract»Brunet L, Moodie EE, Rollet K, et al. Marijuana smoking does not accelerate progression of liver disease in HIV-hepatitis C coinfection: A longitudinal cohort analysis. Clin Infect Dis. 2013;57:663-70.
PubMed Abstract»Carrieri MP, Serfaty L, Vilotitch A, et al. Cannabis Use and Reduced Risk of Insulin Resistance in HIV-HCV Infected Patients: A Longitudinal Analysis (ANRS CO13 HEPAVIH). Clin Infect Dis. 2015;61:40-8.
PubMed Abstract»Costiniuk CT, Brunet L, Rollet-Kurhajec KC, et al. Tobacco Smoking Is Not Associated With Accelerated Liver Disease in Human Immunodeficiency Virus-Hepatitis C Coinfection: A Longitudinal Cohort Analysis. Open Forum Infect Dis. 2016;3:ofw050.
PubMed Abstract»Dawson DA, Grant BF, Stinson FS, Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcohol Clin Exp Res. 2005;29:844-54.
PubMed Abstract»De Luca L, De Angelis C, Fagoonee S, Di Bella S, Rizzetto M, Pellicano R. Is smoking a prognostic factor in patients with chronic hepatitis C? Minerva Gastroeterol Dietol 2009; 55:139-43.
PubMed Abstract»Dev A, Patel K, Conrad A, Blatt LM, McHutchison JG. Relationship of smoking and fibrosis in patients with chronic hepatitis C. Clin Gastroenterol Hepatol. 2006;4:797-801.
PubMed Abstract»Farooqui MT, Khan MA, Cholankeril G, et al. Marijuana is not associated with progression of hepatic fibrosis in liver disease: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2019;31:149-56.
PubMed Abstract»Hézode C, Lonjon I, Roudot-Thoraval F, Mavier JP, Pawlotsky JM, Zafrani ES, Dhumeaux D. Impact of smoking on histological liver lesions in chronic hepatitis C. Gut. 2003;52:126-9.
PubMed Abstract»Hézode C, Lonjon I, Roudot-Thoraval F, Pawlotsky JM, Zafrani ES, Dhumeaux D. Impact of moderate alcohol consumption on histological activity and fibrosis in patients with chronic hepatitis C, and specific influence of steatosis: a prospective study.Aliment Pharmacol Ther. 2003;17:1031-7.
PubMed Abstract»Hézode C, Roudot-Thoraval F, Nguyen S, et al. Daily cannabis smoking as a risk factor for progression of fibrosis in chronic hepatitis C. Hepatology. 2005;42:63-71.
PubMed Abstract»Hézode C, Zafrani ES, Roudot-Thoraval F, et al. Daily cannabis use: a novel risk factor of steatosis severity in patients with chronic hepatitis C. Gastroenterology. 2008;134(2):432-9.
PubMed Abstract»Hsu CC, Kowdley KV. The Effects of Alcohol on Other Chronic Liver Diseases. Clin Liver Dis. 2016;20:581-94.
PubMed Abstract»Ikeda K, Saitoh S, Koida I, et al. A multivariate analysis of risk factors for hepatocellular carcinogenesis: a prospective observation of 795 patients with viral and alcoholic cirrhosis. Hepatology. 1993;18:47-53.
PubMed Abstract»Ishida JH, Peters MG, Jin C, Louie K, Tan V, Bacchetti P, Terrault NA. Influence of cannabis use on severity of hepatitis C disease. Clin Gastroenterol Hepatol. 2008;6:69-75.
PubMed Abstract»Koh WP, Robien K, Wang R, Govindarajan S, Yuan JM, Yu MC. Smoking as an independent risk factor for hepatocellular carcinoma: the Singapore Chinese Health Study. Br J Cancer. 2011 Oct 25;105:1430-5.
PubMed Abstract»Le Lan C, Guillygomarc'h A, Danielou H, et al. A multi-disciplinary approach to treating hepatitis C with interferon and ribavirin in alcohol-dependent patients with ongoing abuse. J Hepatol. 2012;56:334-40.
PubMed Abstract»Marrero JA, Fontana RJ, Fu S, Conjeevaram HS, Su GL, Lok AS. Alcohol, tobacco and obesity are synergistic risk factors for hepatocellular carcinoma. J Hepatol 2005; 42:218-24.
PubMed Abstract»McMahon BJ, Bruden D, Bruce MG, et al. Adverse outcomes in Alaska Natives who recovered from or have chronic hepatitis C infection. Gastroenterology. 2010;138:922-31.
PubMed Abstract»Monto A, Patel K, Bostrom A, Pianko S, Pockros P, McHutchison JG, Wright TL.Risks of a range of alcohol intake on hepatitis C-related fibrosis. Hepatology. 2004;39(3):826-34.
PubMed Abstract»Patsenker E, Sachse P, Chicca A, et al. Elevated levels of endocannabinoids in chronic hepatitis C may modulate cellular immune response and hepatic stellate cell activation. Int J Mol Sci. 2015;16:7057-76.
PubMed Abstract»Pessione F, Degos F, Marcellin P, et al. Effect of alcohol consumption on serum hepatitis C virus RNA and histological lesions in chronic hepatitis C. Hepatology. 1998;27:1717-22.
PubMed Abstract»Pessione F, Ramond MJ, Njapoum C, et al. Cigarette smoking and hepatic lesions in patients with chronic hepatitis C. Hepatology. 2001;34:121-5.
PubMed Abstract»Poynard T, Bedossa P, Opolon P. Lancet. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825-32.
PubMed Abstract»Rigamonti C, Mottaran E, Reale E, et al. Moderate alcohol consumption increases oxidative stress in patients with chronic hepatitis C. Hepatology. 2003;38:42-9.
PubMed Abstract»Russell M, Pauly MP, Moore CD, et al. The impact of lifetime alcohol use on hepatitis C treatment outcomes in privately insured members of an integrated health care plan. Hepatology. 2012;56:1223-30.
PubMed Abstract»Thun MJ, Peto R, Lopez AD, Monaco JH, Henley SJ, Heath CW Jr, Doll R. Alcohol consumption and mortality among middle-aged and elderly U.S. adults. N Engl J Med. 1997;337:1705-14.
PubMed Abstract»Trickey A, Ingle SM, Boyd A, et al. Contribution of alcohol use in HIV/hepatitis C virus co-infection to all-cause and cause-specific mortality: A collaboration of cohort studies. J Viral Hepat. 2023;30:775-86.
PubMed Abstract»Tsochatzis E, Papatheodoridis GV, Manolakopoulos S, Tiniakos DG, Manesis EK, Archimandritis AJ. Smoking is associated with steatosis and severe fibrosis in chronic hepatitis C but not B. Scand J Gastroenterol. 2009;44:752-9.
PubMed Abstract»Tsui JI, Williams EC, Green PK, Berry K, Su F, Ioannou GN. Alcohol use and hepatitis C virus treatment outcomes among patients receiving direct antiviral agents. Drug Alcohol Depend. 2016;169:101-9.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with renal impairment.
AASLD-IDSA Hepatitis C Guidance»Carrieri MP, Serfaty L, Vilotitch A, et al. Cannabis Use and Reduced Risk of Insulin Resistance in HIV-HCV Infected Patients: A Longitudinal Analysis (ANRS CO13 HEPAVIH). Clin Infect Dis. 2015;61:40-8.
PubMed Abstract»Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328-57.
PubMed Abstract»Diehl AM, Day C. Cause, Pathogenesis, and Treatment of Nonalcoholic Steatohepatitis. N Engl J Med. 2017;377:2063-2072.
PubMed Abstract»Fabrizi F, Dixit V, Martin P, Messa P. Combined antiviral therapy of hepatitis C virus in dialysis patients: meta-analysis of clinical trials. J Viral Hepat. 2011;18:e263-9.
PubMed Abstract»Fabrizi F, Dixit V, Messa P, Martin P. Antiviral therapy (pegylated interferon and ribavirin) of hepatitis C in dialysis patients: meta-analysis of clinical studies. J Viral Hepat. 2014;21:681-9.
PubMed Abstract»Fabrizi F, Dixit V, Messa P, Martin P. Interferon therapy of acute hepatitis C in dialysis patients: meta-analysis. J Viral Hepat. 2012;19:784-91.
PubMed Abstract»Fabrizi F, Dixit V, Messa P, Martin P. Pegylated interferon monotherapy of chronic hepatitis C in dialysis patients: Meta-analysis of clinical trials. J Med Virol. 2010;82:768-75.
PubMed Abstract»Fabrizi F, Messa P, Martin P. Recent advances on hepatitis C virus in dialysis population. Kidney Blood Press Res. 2014;39:260-271.
PubMed Abstract»Fabrizi F, Messa P. Therapy of hepatitis C by direct-acting anti-virals: the end of HCV in dialysis population? Expert Rev Clin Pharmacol. 2015;8:785-93.
PubMed Abstract»Fabrizi F, Takkouche B, Lunghi G, Dixit V, Messa P, Martin P. The impact of hepatitis C virus infection on survival in dialysis patients: meta-analysis of observational studies. J Viral Hepat. 2007;14:697-703.
PubMed Abstract»Fabrizi F. Hepatitis C virus infection and dialysis: 2012 update. ISRN Nephrol. 2012;2013:159760.
PubMed Abstract»Freedman ND, Everhart JE, Lindsay KL, et al. Coffee intake is associated with lower rates of liver disease progression in chronic hepatitis C. Hepatology. 2009;50:1360-9.
PubMed Abstract»Garimella T, Wang R, Luo WL, et al. Single-dose pharmacokinetics and safety of daclatasvir in subjects with renal function impairment. Antivir Ther. 2015;20:535-43.
PubMed Abstract»Gordon CE, Uhlig K, Lau J, Schmid CH, Levey AS, Wong JB. Interferon treatment in hemodialysis patients with chronic hepatitis C virus infection: a systematic review of the literature and meta-analysis of treatment efficacy and harms. Am J Kidney Dis. 2008;51:263-77.
PubMed Abstract»Gordon CE, Uhlig K, Schmid CH, Levey AS, Wong JB. Long-term viral negativity after interferon for chronic hepatitis C virus infection in hemodialysis. Clin J Am Soc Nephrol. 2011;6:2226-34.
PubMed Abstract»Gupta SK, Kantesaria B, Glue P. Pharmacokinetics, safety, and tolerability of ribavirin in hemodialysis-dependent patients. Eur J Clin Pharmacol. 2011;68:415-8.
PubMed Abstract»Hézode C, Roudot-Thoraval F, Nguyen S, et al. Daily cannabis smoking as a risk factor for progression of fibrosis in chronic hepatitis C. Hepatology. 2005;42:63-71.
PubMed Abstract»Hézode C, Zafrani ES, Roudot-Thoraval F, et al. Daily cannabis use: a novel risk factor of steatosis severity in patients with chronic hepatitis C. Gastroenterology. 2008;134(2):432-9.
PubMed Abstract»Heymsfield SB, Wadden TA. Mechanisms, Pathophysiology, and Management of Obesity. N Engl J Med. 2017;376:254-266.
PubMed Abstract»Hodge A, Lim S, Goh E, et al. Coffee Intake Is Associated with a Lower Liver Stiffness in Patients with Non-Alcoholic Fatty Liver Disease, Hepatitis C, and Hepatitis B. Nutrients. 2017;9:56.
PubMed Abstract»Ishida JH, Peters MG, Jin C, Louie K, Tan V, Bacchetti P, Terrault NA. Influence of cannabis use on severity of hepatitis C disease. Clin Gastroenterol Hepatol. 2008;6:69-75.
PubMed Abstract»Kalyan Ram B, Frank C, Adam P, et al. Safety, efficacy and tolerability of half-dose sofosbuvir plus simeprevir in treatment of Hepatitis C in patients with end stage renal disease. J Hepatol. 2015;63:763-5.
PubMed Abstract»Kidney Disease Outcome Quality Initiative (KDOQI) Clinical Practice Guidelines. Hepatitis C Management in Kidney Transplantation.
KDOQI»Kumada H, Toyota J, Okanoue T, Chayama K, Tsubouchi H, Hayashi N. Telaprevir with peginterferon and ribavirin for treatment-naive patients chronically infected with HCV of genotype 1 in Japan. J Hepatol. 2011;56:78-84.
PubMed Abstract»Liu CH, Huang CF, Liu CJ, et al. Pegylated interferon-α2a with or without low-dose ribavirin for treatment-naive patients with hepatitis C virus genotype 1 receiving hemodialysis: a randomized trial. Ann Intern Med. 2013;159:729-38.
PubMed Abstract»Liu CH, Liang CC, Lin JW, et al. Pegylated interferon alpha-2a versus standard interferon alpha-2a for treatment-naive dialysis patients with chronic hepatitis C: a randomised study. Gut. 2007;57:525-30.
PubMed Abstract»Liu CH, Liang CC, Liu CJ, et al. Pegylated interferon alfa-2a monotherapy for hemodialysis patients with acute hepatitis C. Clin Infect Dis. 2010;51:541-9.
PubMed Abstract»Liu CH, Liu CJ, Huang CF, et al. Peginterferon alfa-2a with or without low-dose ribavirin for treatment-naive patients with hepatitis C virus genotype 2 receiving haemodialysis: a randomised trial. Gut. 2015;64:303-11.
PubMed Abstract»Marrero JA, Fontana RJ, Fu S, Conjeevaram HS, Su GL, Lok AS. Alcohol, tobacco and obesity are synergistic risk factors for hepatocellular carcinoma. J Hepatol 2005; 42:218-24.
PubMed Abstract»Maruyama A, Partovi N, Yoshida EM, Erb SR, Azalgara VM, Hussaini T. A review of direct-acting antivirals for the treatment of hepatitis C in patients with advanced chronic kidney disease. Nephrol Dial Transplant. 2017;32:35-41.
PubMed Abstract»Mauss S, Hueppe D, Alshuth U. Renal impairment is frequent in chronic hepatitis C patients under triple therapy with telaprevir or boceprevir. Hepatology. 2013;59:46-8.
PubMed Abstract»Nazario HE, Ndungu M, Modi AA. Sofosbuvir and simeprevir in hepatitis C genotype 1-patients with end-stage renal disease on haemodialysis or GFR <30 ml/min. Liver Int. 2016;36:798-801.
PubMed Abstract»Pockros PJ, Reddy KR, Mantry PS, et al. Efficacy of Direct-Acting Antiviral Combination for Patients With Hepatitis C Virus Genotype 1 Infection and Severe Renal Impairment or End-Stage Renal Disease. Gastroenterology. 2016;150:1590-8.
PubMed Abstract»Poynard T, Bedossa P, Opolon P. Lancet. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825-32.
PubMed Abstract»Rinella ME, Lazarus JV, Ratziu V, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol. 2023;79:1542-56.
PubMed Abstract»Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015;313:2263-73.
PubMed Abstract»Roth D, Nelson DR, Bruchfeld A, et al. Grazoprevir plus elbasvir in treatment-naive and treatment-experienced patients with hepatitis C virus genotype 1 infection and stage 4-5 chronic kidney disease (the C-SURFER study): a combination phase 3 study. Lancet. 2015;386:1537-45.
PubMed Abstract»Ruhl CE, Everhart JE. Coffee and tea consumption are associated with a lower incidence of chronic liver disease in the United States. Gastroenterology. 2005;129:1928-36.
PubMed Abstract»Russo MW, Goldsweig CD, Jacobson IM, Brown RS Jr. Interferon monotherapy for dialysis patients with chronic hepatitis C: an analysis of the literature on efficacy and safety. Am J Gastroenterol. 2003;98:1610-5.
PubMed Abstract»Saadoun D, Resche Rigon M, Thibault V, et al. Peg-IFNα/ribavirin/protease inhibitor combination in hepatitis C virus associated mixed cryoglobulinemia vasculitis: results at week 24. Ann Rheum Dis. 2013;73:831-7.
PubMed Abstract»Sawinski D, Kaur N, Ajeti A, et al. Successful Treatment of Hepatitis C in Renal Transplant Recipients With Direct-Acting Antiviral Agents. Am J Transplant. 2016;16:1588-95.
PubMed Abstract»Saxena V, Koraishy FM, Sise ME, et al. Safety and efficacy of sofosbuvir-containing regimens in hepatitis C-infected patients with impaired renal function. Liver Int. 2016;36:807-16.
PubMed Abstract»Tempestilli M, Lionetti R, D'Offizi G, et al. Increased plasma concentration of ribavirin as a result of renal dysfunction in hepatitis C virus patients treated with telaprevir. Hepatology. 2014;60:1109-10.
PubMed Abstract»Tseng PL, Chen TC, Chien YS, et al. Efficacy and safety of pegylated interferon alfa-2b and ribavirin combination therapy versus pegylated interferon monotherapy in hemodialysis patients: a comparison of 2 sequentially treated cohorts. Am J Kidney Dis. 2013;62:789-95.
PubMed Abstract»Wang KL, Xing HQ, Zhao H, et al. Efficacy and tolerability of low-dose interferon-α in hemodialysis patients with chronic hepatitis C virus infection. World J Gastroenterol. 2014;20:4071-5.
PubMed Abstract»Wang T, Xi Y, Raji A, et al. Overall and subgroup prevalence of non-alcoholic fatty liver disease and prevalence of advanced fibrosis in the United States: An updated national estimate in National Health and Nutrition Examination Survey (NHANES) 2011-2018. Ann Hepatol. 2024;29:101154.
PubMed Abstract»Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11-20.
PubMed Abstract»Lesson 4. Evaluation and Staging of Liver Fibrosis
Background
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Boursier J, de Ledinghen V, Zarski JP, et al. Comparison of eight diagnostic algorithms for liver fibrosis in hepatitis C: new algorithms are more precise and entirely noninvasive. Hepatology. 2012;55:58-67.
PubMed Abstract»Carlson JJ, Kowdley KV, Sullivan SD, Ramsey SD, Veenstra DL. An evaluation of the potential cost-effectiveness of non-invasive testing strategies in the diagnosis of significant liver fibrosis. J Gastroenterol Hepatol. 2009;24:786-91.
PubMed Abstract»Chou R, Wasson N. Blood tests to diagnose fibrosis or cirrhosis in patients with chronic hepatitis C virus infection: a systematic review. Ann Intern Med. 2013;158:807-20.
PubMed Abstract»Duarte-Rojo A, Altamirano JT, Feld JJ. Noninvasive markers of fibrosis: key concepts for improving accuracy in daily clinical practice. Ann Hepatol. 2012;11:426-39.
PubMed Abstract»Friedman SL. Evolving challenges in hepatic fibrosis. Nat Rev Gastroenterol Hepatol. 2010;7:425-36.
PubMed Abstract»Hernandez-Gea V, Friedman SL. Pathogenesis of liver fibrosis. Annu Rev Pathol. 2011;6:425-56.
PubMed Abstract»Lackner C, Struber G, Liegl B, et al. Comparison and validation of simple noninvasive tests for prediction of fibrosis in chronic hepatitis C. Hepatology. 2005;41:1376-82.
PubMed Abstract»Nguyen D, Talwalkar JA. Noninvasive assessment of liver fibrosis. Hepatology. 2011;53:2107-10.
PubMed Abstract»Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD; American Association for the Study of Liver Diseases. Liver biopsy. Hepatology. 2009;49:1017-44.
PubMed Abstract»Seki E, Brenner DA. Recent advancement of molecular mechanisms of liver fibrosis. J Hepatobiliary Pancreat Sci. 2015;22:512-8.
PubMed Abstract»Sharma S, Khalili K, Nguyen GC. Non-invasive diagnosis of advanced fibrosis and cirrhosis. World J Gastroenterol. 2014;20:16820-30.
PubMed Abstract»Talwalkar JA. Elastography for detecting hepatic fibrosis: options and considerations. Gastroenterology. 2008;135:299-302.
PubMed Abstract»van Katwyk S, Coyle D, Cooper C, et al. Transient elastography for the diagnosis of liver fibrosis: a systematic review of economic evaluations. Liver Int. 2017;37:851-861.
PubMed Abstract»Indirect Markers for Estimating Hepatic Fibrosis
Becker L, Salameh W, Sferruzza A, et al. Validation of hepascore, compared with simple indices of fibrosis, in patients with chronic hepatitis C virus infection in United States. Clin Gastroenterol Hepatol. 2009;7:696-701.
PubMed Abstract»Castera L. Noninvasive methods to assess liver disease in patients with hepatitis B or C. Gastroenterology. 2012;142:1293-1302.e4.
PubMed Abstract»Duarte-Rojo A, Altamirano JT, Feld JJ. Noninvasive markers of fibrosis: key concepts for improving accuracy in daily clinical practice. Ann Hepatol. 2012;11:426-39.
PubMed Abstract»Forns X, Ampurdanès S, Llovet JM, et al. Identification of chronic hepatitis C patients without hepatic fibrosis by a simple predictive model. Hepatology. 2002;36(4 Pt 1):986-92.
PubMed Abstract»Gressner OA, Weiskirchen R, Gressner AM. Biomarkers of hepatic fibrosis, fibrogenesis and genetic pre-disposition pending between fiction and reality. J Cell Mol Med. 2007;11:1031-51.
PubMed Abstract»Guéchot J, Laudat A, Loria A, Serfaty L, Poupon R, Giboudeau J. Diagnostic accuracy of hyaluronan and type III procollagen amino-terminal peptide serum assays as markers of liver fibrosis in chronic viral hepatitis C evaluated by ROC curve analysis. Clin Chem. 1996;42:558-63.
PubMed Abstract»Haseltine EL, Penney MS, George S, Kieffer TL. Successful treatment with telaprevir-based regimens for chronic hepatitis C results in significant improvements to serum markers of liver fibrosis. J Viral Hepat. 2015;22:701-7.
PubMed Abstract»Holmberg SD, Lu M, Rupp LB, et al. Noninvasive serum fibrosis markers for screening and staging chronic hepatitis C virus patients in a large US cohort. Clin Infect Dis. 2013;57:240-6.
PubMed Abstract»Koda M, Matunaga Y, Kawakami M, Kishimoto Y, Suou T, Murawaki Y. FibroIndex, a practical index for predicting significant fibrosis in patients with chronic hepatitis C. Hepatology. 2007;45:297-306.
PubMed Abstract»Lin ZH, Xin YN, Dong QJ, et al. Performance of the aspartate aminotransferase-to-platelet ratio index for the staging of hepatitis C-related fibrosis: an updated meta-analysis. Hepatology. 2011;53:726-36.
PubMed Abstract»Nguyen D, Talwalkar JA. Noninvasive assessment of liver fibrosis. Hepatology. 2011;53:2107-10.
PubMed Abstract»Patel K, Benhamou Y, Yoshida EM, et al. An independent and prospective comparison of two commercial fibrosis marker panels (HCV FibroSURE and FIBROSpect II) during albinterferon alfa-2b combination therapy for chronic hepatitis C. J Viral Hepat. 2009;16:178-86.
PubMed Abstract»Poynard T, Imbert-Bismut F, Munteanu M, et al. Overview of the diagnostic value of biochemical markers of liver fibrosis (FibroTest, HCV FibroSure) and necrosis (ActiTest) in patients with chronic hepatitis C. Comp Hepatol. 2004;3:8.
PubMed Abstract»Poynard T, Morra R, Halfon P, et al. Meta-analyses of FibroTest diagnostic value in chronic liver disease. BMC Gastroenterol. 2007;7:40.
PubMed Abstract»Schmid P, Bregenzer A, Huber M, et al. Progression of Liver Fibrosis in HIV/HCV Co-Infection: A Comparison between Non-Invasive Assessment Methods and Liver Biopsy. PLoS One. 2015;10:e0138838.
PubMed Abstract»Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43:1317-25.
PubMed Abstract»Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43:1317–25.
PubMed Abstract»Suan MAM, Chan HK, Sem X, Shilton S, Hassan MRA. Diagnostic performance of two non-invasive biomarkers used individually and in sequential combination for cirrhosis associated with hepatitis C virus infection. Sci Rep. 2022;12:20153.
PubMed Abstract»Thabut D, Simon M, Myers RP, et al. Noninvasive prediction of fibrosis in patients with chronic hepatitis C. Hepatology. 2003;37:1220-1.
PubMed Abstract»Tural C, Tor J, Sanvisens A, et al. Accuracy of simple biochemical tests in identifying liver fibrosis in patients co-infected with human immunodeficiency virus and hepatitis C virus. Clin Gastroenterol Hepatol. 2009;7:339-45.
PubMed Abstract»Vallet-Pichard A, Mallet V, Nalpas B, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology. 2007;46:32-6.
PubMed Abstract»Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, Lok AS. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38:518-26.
PubMed Abstract»Direct Markers of Fibrosis
Friedman SL. Evolving challenges in hepatic fibrosis. Nat Rev Gastroenterol Hepatol. 2010;7:425-36.
PubMed Abstract»Hernandez-Gea V, Friedman SL. Pathogenesis of liver fibrosis. Annu Rev Pathol. 2011;6:425-56.
PubMed Abstract»Manning DS, Afdhal NH. Diagnosis and quantitation of fibrosis. Gastroenterology. 2008;134:1670-81.
PubMed Abstract»Neuman MG, Cohen LB, Nanau RM. Hyaluronic acid as a non-invasive biomarker of liver fibrosis. Clin Biochem. 2016;49:302-15.
PubMed Abstract»Patel K, Benhamou Y, Yoshida EM, et al. An independent and prospective comparison of two commercial fibrosis marker panels (HCV FibroSURE and FIBROSpect II) during albinterferon alfa-2b combination therapy for chronic hepatitis C. J Viral Hepat. 2009;16:178-86.
PubMed Abstract»Patel K, Gordon SC, Jacobson I, et al. Evaluation of a panel of non-invasive serum markers to differentiate mild from moderate-to-advanced liver fibrosis in chronic hepatitis C patients. J Hepatol. 2004;41:935-42.
PubMed Abstract»Zaman A, Rosen HR, Ingram K, Corless CL, Oh E, Smith K. Assessment of FIBROSpect II to detect hepatic fibrosis in chronic hepatitis C patients. Am J Med. 2007;120:280.e9-14.
PubMed Abstract»Radiologic Modalities to Estimate Fibrosis
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Afdhal NH. Fibroscan (transient elastography) for the measurement of liver fibrosis. Gastroenterol Hepatol (N Y). 2012;8:605-7.
PubMed Abstract»Ammon FJ, Kohlhaas A, Elshaarawy O, et al. Liver stiffness reversibly increases during pregnancy and independently predicts preeclampsia. World J Gastroenterol. 2018;24:4393-402.
PubMed Abstract»Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»Bonekamp S, Kamel I, Solga S, Clark J. Can imaging modalities diagnose and stage hepatic fibrosis and cirrhosis accurately? J Hepatol. 2009;50:17-35.
PubMed Abstract»Castera L, Forns X, Alberti A. Non-invasive evaluation of liver fibrosis using transient elastography. J Hepatol. 2008;48:835-47.
PubMed Abstract»Castera L, Vergniol J, Foucher J, et al. Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology. 2005;128:343-50.
PubMed Abstract»Castera L. Noninvasive methods to assess liver disease in patients with hepatitis B or C. Gastroenterology. 2012;142:1293-1302.e4.
PubMed Abstract»Gara N, Zhao X, Kleiner DE, Liang TJ, Hoofnagle JH, Ghany MG. Discordance among transient elastography, aspartate aminotransferase to platelet ratio index, and histologic assessments of liver fibrosis in patients with chronic hepatitis C. Clin Gastroenterol Hepatol. 2013;11:303-8.
PubMed Abstract»Goyal N, Jain N, Rachapalli V, Cochlin DL, Robinson M. Non-invasive evaluation of liver cirrhosis using ultrasound. Clin Radiol. 2009;64:1056-66.
PubMed Abstract»Kelly EMM, Feldstein VA, Parks M, Hudock R, Etheridge D, Peters MG. An Assessment of the Clinical Accuracy of Ultrasound in Diagnosing Cirrhosis in the Absence of Portal Hypertension. Gastroenterol Hepatol (N Y). 2018;14:367-73.
PubMed Abstract»Kim HJ, Lee HK, Cho JH, Yang HJ. Quantitative comparison of transient elastography (TE), shear wave elastography (SWE) and liver biopsy results of patients with chronic liver disease. J Phys Ther Sci. 2015;27:2465-8.
PubMed Abstract»Kirk GD, Astemborski J, Mehta SH, et al. Assessment of liver fibrosis by transient elastography in persons with hepatitis C virus infection or HIV-hepatitis C virus coinfection. Clin Infect Dis. 2009;48:963-72.
PubMed Abstract»Li S, Sun X, Chen M, et al. Liver Fibrosis Conventional and Molecular Imaging Diagnosis Update. J Liver. 2019;8:236.
PubMed Abstract»Schmeltzer PA, Talwalkar JA. Noninvasive tools to assess hepatic fibrosis: ready for prime time? Gastroenterol Clin North Am. 2011;40:507-21.
PubMed Abstract»Shire NJ, Yin M, Chen J, et al. Test-retest repeatability of MR elastography for noninvasive liver fibrosis assessment in hepatitis C. J Magn Reson Imaging. 2011;34:947-55.
PubMed Abstract»Steadman R, Myers RP, Leggett L, et al. A health technology assessment of transient elastography in adult liver disease. Can J Gastroenterol. 2013;27:149-58.
PubMed Abstract»Talwalkar JA, Yin M, Fidler JL, Sanderson SO, Kamath PS, Ehman RL. Magnetic resonance imaging of hepatic fibrosis: emerging clinical applications. Hepatology. 2008;47:332-42.
PubMed Abstract»Talwalkar JA. Elastography for detecting hepatic fibrosis: options and considerations. Gastroenterology. 2008;135:299-302.
PubMed Abstract»Verlinden W, Bourgeois S, Gigase P, et al. Liver Fibrosis Evaluation Using Real-time Shear Wave Elastography in Hepatitis C-Monoinfected and Human Immunodeficiency Virus/Hepatitis C-Coinfected Patients. J Ultrasound Med. 2016;35:1299-308.
PubMed Abstract»Wang QB, Zhu H, Liu HL, Zhang B. Performance of magnetic resonance elastography and diffusion-weighted imaging for the staging of hepatic fibrosis: A meta-analysis. Hepatology. 2012;56:239-47.
PubMed Abstract»Wang Y, Ganger DR, Levitsky J, et al. Assessment of chronic hepatitis and fibrosis: comparison of MR elastography and diffusion-weighted imaging. AJR Am J Roentgenol. 2011;196:553-61.
PubMed Abstract»Ziol M, Handra-Luca A, Kettaneh A, et al. Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with chronic hepatitis C. Hepatology. 2005;41:48-54.
PubMed Abstract»Liver Biopsy and Histologic Assessment of the Liver
Batts KP, Ludwig J. Chronic hepatitis. An update on terminology and reporting. Am J Surg Pathol. 1995;19:1409-17.
PubMed Abstract»Becker L, Salameh W, Sferruzza A, et al. Validation of hepascore, compared with simple indices of fibrosis, in patients with chronic hepatitis C virus infection in United States. Clin Gastroenterol Hepatol. 2009;7:696-701.
PubMed Abstract»Bedossa P, Dargère D, Paradis V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology. 2003;38:1449-57.
PubMed Abstract»Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology. 1996;24:289-93.
PubMed Abstract»Chowdhury AB, Mehta KJ. Liver biopsy for assessment of chronic liver diseases: a synopsis. Clin Exp Med. 2023;23:273-85.
PubMed Abstract»Gara N, Zhao X, Kleiner DE, Liang TJ, Hoofnagle JH, Ghany MG. Discordance among transient elastography, aspartate aminotransferase to platelet ratio index, and histologic assessments of liver fibrosis in patients with chronic hepatitis C. Clin Gastroenterol Hepatol. 2013;11:303-8.
PubMed Abstract»Ginès P, Krag A, Abraldes JG, Solà E, Fabrellas N, Kamath PS. Liver cirrhosis. Lancet. 2021;398:1359-76.
PubMed Abstract»Guido M, Mangia A, Faa G; Gruppo Italiano Patologi Apparato Digerente (GIPAD); Società Italiana di Anatomia Patologica e Citopatologia Diagnostica/International Academy of Pathology, Italian division (SIAPEC/IAP). Chronic viral hepatitis: the histology report. Dig Liver Dis. 2011;43 Suppl 4:S331-43.
PubMed Abstract»Ishak K, Baptista A, Bianchi L, et al. Histological grading and staging of chronic hepatitis. J Hepatol. 1995;22:696-9.
PubMed Abstract»Knodell RG, Ishak KG, Black WC, et al. Formulation and application of a numerical scoring system for assessing histological activity in asymptomatic chronic active hepatitis. Hepatology. 1981;1:431-5.
PubMed Abstract»Lefkowitch JH.Arch Med Res. Liver biopsy assessment in chronic hepatitis. 2007;38:634-43.
PubMed Abstract»Malik AH, Kumar KS, Malet PF, Jain R, Prasad P, Ostapowicz G. Correlation of percutaneous liver biopsy fragmentation with the degree of fibrosis. Aliment Pharmacol Ther. 2004;19:545-9.
PubMed Abstract»Manning DS, Afdhal NH. Diagnosis and quantitation of fibrosis. Gastroenterology. 2008;134:1670-81.
PubMed Abstract»Piccinino F, Sagnelli E, Pasquale G, Giusti G. Complications following percutaneous liver biopsy. A multicentre retrospective study on 68,276 biopsies. J Hepatol. 1986;2:165-73.
PubMed Abstract»Regev A, Berho M, Jeffers LJ, et al. Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol. 2002;97:2614-8.
PubMed Abstract»Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD; American Association for the Study of Liver Diseases. Liver biopsy. Hepatology. 2009;49:1017-44.
PubMed Abstract»Scheuer PJ. Classification of chronic viral hepatitis: a need for reassessment. J Hepatol. 1991;13:372-4.
PubMed Abstract»Schmeltzer PA, Talwalkar JA. Noninvasive tools to assess hepatic fibrosis: ready for prime time? Gastroenterol Clin North Am. 2011;40:507-21.
PubMed Abstract»Theise ND. Liver biopsy assessment in chronic viral hepatitis: a personal, practical approach. Mod Pathol. 2007;20 Suppl 1:S3-14.
PubMed Abstract»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with renal impairment.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Boursier J, Bacq Y, Halfon P, et al. Improved diagnostic accuracy of blood tests for severe fibrosis and cirrhosis in chronic hepatitis C. Eur J Gastroenterol Hepatol. 2009;21:28-38.
PubMed Abstract»Castera L. Noninvasive methods to assess liver disease in patients with hepatitis B or C. Gastroenterology. 2012;142:1293-1302.e4.
PubMed Abstract»Gupta SK, Pittenger AL, Swan SK, et al. Single-dose pharmacokinetics and safety of pegylated interferon-alpha2b in patients with chronic renal dysfunction. J Clin Pharmacol. 2002;42:1109-15.
PubMed Abstract»Halfon P, Bacq Y, De Muret A, et al. Comparison of test performance profile for blood tests of liver fibrosis in chronic hepatitis C. J Hepatol. 2007;46:395-402.
PubMed Abstract»Harris R, Harman DJ, Card TR, Aithal GP, Guha IN. Prevalence of clinically significant liver disease within the general population, as defined by non-invasive markers of liver fibrosis: a systematic review. Lancet Gastroenterol Hepatol. 2017;2:288-297.
PubMed Abstract»Kidney Disease Improving Global Outcomes (KDIGO) Guideline for the Prevention, Diagnosis, Evaluation and Treatment of Hepatitis C in Chronic Kidney Disease.
KDIGO»Maruyama A, Partovi N, Yoshida EM, Erb SR, Azalgara VM, Hussaini T. A review of direct-acting antivirals for the treatment of hepatitis C in patients with advanced chronic kidney disease. Nephrol Dial Transplant. 2017;32:35-41.
PubMed Abstract»Naganuma H, Ishida H, Uno A, Nagai H, Kuroda H, Ogawa M. Diagnostic problems in two-dimensional shear wave elastography of the liver. World J Radiol. 2020;12:76-86.
PubMed Abstract»Peginterferon alfa-2a (Pegasys) Full Prescribing Information
Hoffman-La Roche, Inc. and Genetech, Inc.»Rossi E, Adams L, Prins A, et al. Validation of the FibroTest biochemical markers score in assessing liver fibrosis in hepatitis C patients. Clin Chem. 2003;49:450-4.
PubMed Abstract»Rostaing L, Chatelut E, Payen JL, et al. Pharmacokinetics of alphaIFN-2b in chronic hepatitis C virus patients undergoing chronic hemodialysis or with normal renal function: clinical implications. J Am Soc Nephrol. 1998;9:2344-8.
PubMed Abstract»Talal AH, LaFleur J, Hoop R, et al. Absolute and relative contraindications to pegylated-interferon or ribavirin in the US general patient population with chronic hepatitis C: results from a US database of over 45 000 HCV-infected, evaluated patients. Aliment Pharmacol Ther. 2013;37:473-81.
PubMed Abstract»Theise ND. Liver biopsy assessment in chronic viral hepatitis: a personal, practical approach. Mod Pathol. 2007;20 Suppl 1:S3-14.
PubMed Abstract»Yee HS, Chang MF, Pocha C, et al. Update on the management and treatment of hepatitis C virus infection: recommendations from the Department of Veterans Affairs Hepatitis C Resource Center Program and the National Hepatitis C Program Office. Am J Gastroenterol. 2012;107:669-89.
PubMed Abstract»Zarski JP, Sturm N, Guechot J, et al. Comparison of nine blood tests and transient elastography for liver fibrosis in chronic hepatitis C: the ANRS HCEP-23 study. J Hepatol. 2012;56:55-62.
PubMed Abstract»Lesson 5. Evaluation and Prognosis of Persons with Cirrhosis
Background
Brunner F, Berzigotti A, Bosch J. Prevention and treatment of variceal haemorrhage in 2017. Liver Int. 2017;37 Suppl 1:104-115.
PubMed Abstract»D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-31.
PubMed Abstract»D'Amico G, Morabito A, Pagliaro L, Marubini E. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig Dis Sci. 1986;31:468-75.
PubMed Abstract»de Bruyn G, Graviss EA. A systematic review of the diagnostic accuracy of physical examination for the detection of cirrhosis. BMC Med Inform Decis Mak. 2001;1:6.
PubMed Abstract»Fleming KM, Aithal GP, Card TR, West J. All-cause mortality in people with cirrhosis compared with the general population: a population-based cohort study. Liver Int. 2012;32:79-84.
PubMed Abstract»Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335.
PubMed Abstract»Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010;362:823-32.
PubMed Abstract»Garcia-Tsao G, Friedman S, Iredale J, Pinzani M. Now there are many (stages) where before there was one: In search of a pathophysiological classification of cirrhosis. Hepatology. 2010;51:1445-9.
PubMed Abstract»Garcia-Tsao G, Lim JK; Members of Veterans Affairs Hepatitis C Resource Center Program. Management and treatment of patients with cirrhosis and portal hypertension: recommendations from the Department of Veterans Affairs Hepatitis C Resource Center Program and the National Hepatitis C Program. Am J Gastroenterol. 2009;104:1802-29.
PubMed Abstract»Ge PS, Runyon BA. Treatment of Patients with Cirrhosis. N Engl J Med. 2016;375:767-77.
PubMed Abstract»Hajarizadeh B, Grebely J, Dore GJ. Epidemiology and natural history of HCV infection. Nat Rev Gastroenterol Hepatol. 2013;10:553-62.
PubMed Abstract»Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. Am Fam Physician.2006;74:756-62.
PubMed Abstract»Liang TJ, Rehermann B, Seeff LB, Hoofnagle JH. Pathogenesis, natural history, treatment, and prevention of hepatitis C. Ann Intern Med. 2000;132:296-305.
PubMed Abstract»Lingala S, Ghany MG. Natural History of Hepatitis C. Gastroenterol Clin North Am. 2015;44:717-34.
PubMed Abstract»Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144-65.
PubMed Abstract»Planas R, Ballesté B, Alvarez MA, et al. Natural history of decompensated hepatitis C virus-related cirrhosis. J Hepatol. 2004;40:823-30.
PubMed Abstract»Starr SP, Raines D. Cirrhosis: diagnosis, management, and prevention. Am Fam Physician. 2011;84:1353-9.
PubMed Abstract»Zipprich A, Garcia-Tsao G, Rogowski S, Fleig WE, Seufferlein T, Dollinger MM. Prognostic indicators of survival in patients with compensated and decompensated cirrhosis. Liver Int. 2012;32:1407-14.
PubMed Abstract»Evaluation of Persons with Cirrhosis
Adinolfi LE, Nevola R, Rinaldi L, Romano C, Giordano M. Chronic Hepatitis C Virus Infection and Depression. Clin Liver Dis. 2017;21:517-534.
PubMed Abstract»Cattau EL Jr, Benjamin SB, Knuff TE, Castell DO. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982;247:1164-6.
PubMed Abstract»de Bruyn G, Graviss EA. A systematic review of the diagnostic accuracy of physical examination for the detection of cirrhosis. BMC Med Inform Decis Mak. 2001;1:6.
PubMed Abstract»Durand F, Valla D. Assessment of prognosis of cirrhosis. Semin Liver Dis. 2008;28:110-22.
PubMed Abstract»Freeman RB Jr, Wiesner RH, Harper A, et al. The new liver allocation system: moving toward evidence-based transplantation policy. Liver Transpl. 2002;8:851-8.
PubMed Abstract»Hézode C, Roudot-Thoraval F, Nguyen S, et al. Daily cannabis smoking as a risk factor for progression of fibrosis in chronic hepatitis C. Hepatology. 2005;42:63-71.
PubMed Abstract»Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. Am Fam Physician.2006;74:756-62.
PubMed Abstract»Leslie J, Geh D, Elsharkawy AM, Mann DA, Vacca M. Metabolic dysfunction and cancer in HCV: Shared pathways and mutual interactions. J Hepatol. 2022;77:219-36.
PubMed Abstract»Rinella ME, Lazarus JV, Ratziu V, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol. 2023;79:1542-56.
PubMed Abstract»Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015;313:2263-73.
PubMed Abstract»Starr SP, Raines D. Cirrhosis: diagnosis, management, and prevention. Am Fam Physician. 2011;84:1353-9.
PubMed Abstract»Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012;307:832-42.
PubMed Abstract»Vargas M, Cardoso Toniasso SC, Riedel PG, et al. Metabolic disease and the liver: A review. World J Hepatol. 2024;16:33-40.
PubMed Abstract»Wiley TE, McCarthy M, Breidi L, McCarthy M, Layden TJ. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology. 1998;28:805-9.
PubMed Abstract»Classification Systems for Persons with Cirrhosis
Bruno S, Zuin M, Crosignani A, et al. Predicting mortality risk in patients with compensated HCV-induced cirrhosis: a long-term prospective study. Am J Gastroenterol. 2009;104:1147-58.
PubMed Abstract»Child CG, Turcotte JG. Surgery and portal hypertension. Major Probl Clin Surg. 1964;1:1-85.
PubMed Abstract»D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-31.
PubMed Abstract»D'Amico G, Morabito A, Pagliaro L, Marubini E. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig Dis Sci. 1986;31:468-75.
PubMed Abstract»Durand F, Valla D. Assessment of prognosis of cirrhosis. Semin Liver Dis. 2008;28:110-22.
PubMed Abstract»Durand F, Valla D. Assessment of the prognosis of cirrhosis: Child-Pugh versus MELD. J Hepatol. 2005;42 Suppl:S100-7.
PubMed Abstract»Freeman RB Jr, Wiesner RH, Harper A, et al. The new liver allocation system: moving toward evidence-based transplantation policy. Liver Transpl. 2002;8:851-8.
PubMed Abstract»Kalra A, Wedd JP, Biggins SW. Changing prioritization for transplantation: MELD-Na, hepatocellular carcinoma exceptions, and more. Curr Opin Organ Transplant. 2016;21:120-6.
PubMed Abstract»Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464-70.
PubMed Abstract»Kim WR, Mannalithara A, Heimbach JK, et al. MELD 3.0: The Model for End-Stage Liver Disease Updated for the Modern Era. Gastroenterology. 2021;161:1887-95.
PubMed Abstract»Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864-71.
PubMed Abstract»Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144-65.
PubMed Abstract»Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646-9.
PubMed Abstract»Wiesner R, Edwards E, Freeman R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91-6.
PubMed Abstract»Compensated Cirrhosis
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»Asselah T, Kowdley KV, Zadeikis N, et al. Efficacy of Glecaprevir/Pibrentasvir for 8 or 12 Weeks in Patients With Hepatitis C Virus Genotype 2, 4, 5, or 6 Infection Without Cirrhosis. Clin Gastroenterol Hepatol. 2018;16:417-26.
PubMed Abstract»D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-31.
PubMed Abstract»D'Amico G, Morabito A, D'Amico M, et al. Clinical states of cirrhosis and competing risks. J Hepatol. 2018;68:563-576.
PubMed Abstract»Di Bisceglie AM, Shiffman ML, Everson GT, et al. Prolonged therapy of advanced chronic hepatitis C with low-dose peginterferon. N Engl J Med. 2008;359:2429-41.
PubMed Abstract»El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterol. 2007;132:2557-76.
PubMed Abstract»Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599-607.
PubMed Abstract»Forns X, Lee SS, Valdes J, et al. Glecaprevir plus pibrentasvir for chronic hepatitis C virus genotype 1, 2, 4, 5, or 6 infection in adults with compensated cirrhosis (EXPEDITION-1): a single-arm, open-label, multicentre phase 3 trial. Lancet Infect Dis. 2017;17:1062-1068.
PubMed Abstract»Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335.
PubMed Abstract»Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010;362:823-32.
PubMed Abstract»Ioannou GN. HCC surveillance after SVR in patients with F3/F4 fibrosis. J Hepatol. 2021;74:458-65.
PubMed Abstract»Lawitz E, Gane E, Pearlman B, et al. Efficacy and safety of 12 weeks versus 18 weeks of treatment with grazoprevir (MK-5172) and elbasvir (MK-8742) with or without ribavirin for hepatitis C virus genotype 1 infection in previously untreated patients with cirrhosis and patients with previous null response with or without cirrhosis (C-WORTHY): a randomised, open-label phase 2 trial. Lancet. 2015;385:1075-86.
PubMed Abstract»Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68:723-50.
PubMed Abstract»Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144-65.
PubMed Abstract»Morgan TR, Ghany MG, Kim HY, et al. Outcome of sustained virological responders with histologically advanced chronic hepatitis C. Hepatology. 2010;52:833-44.
PubMed Abstract»Singal AG, Volk ML, Jensen D, Di Bisceglie AM, Schoenfeld PS. A sustained viral response is associated with reduced liver-related morbidity and mortality in patients with hepatitis C virus. Clin Gastroenterol Hepatol. 2010;8:280-8.
PubMed Abstract»Thiele M, Johansen S, Israelsen M, et al. Non-invasive assessment of hepatic decompensation. Hepatology. 2023 Oct 6. Online ahead of print.
PubMed Abstract»van der Meer AJ, Veldt BJ, Feld JJ, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012 ;308:2584-93.
PubMed Abstract»Decompensated Cirrhosis
Angeli P, Gines P, Wong F, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: revised consensus recommendations of the International Club of Ascites. Gut. 2015;64:531-7.
PubMed Abstract»Baraldi O, Valentini C, Donati G, et al. Hepatorenal syndrome: Update on diagnosis and treatment. World J Nephrol. 2015;4:511-20.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Bunchorntavakul C, Reddy KR. Treat chronic hepatitis C virus infection in decompensated cirrhosis - pre- or post-liver transplantation? the ironic conundrum in the era of effective and well-tolerated therapy. J Viral Hepat. 2016;23:408-18.
PubMed Abstract»Cheung MCM, Walker AJ, Hudson BE, et al. Outcomes after successful direct-acting antiviral therapy for patients with chronic hepatitis C and decompensated cirrhosis. J Hepatol. 2016;65:741-747.
PubMed Abstract»Cholankeril G, Joseph-Talreja M, Perumpail BJ, et al. Timing of Hepatitis C Virus Treatment in Liver Transplant Candidates in the Era of Direct-acting Antiviral Agents. J Clin Transl Hepatol. 2017;5:363-367.
PubMed Abstract»Curry MP, O'Leary JG, Bzowej N, et al. Sofosbuvir and Velpatasvir for HCV in Patients with Decompensated Cirrhosis. N Engl J Med. 2015;373:2618-28.
PubMed Abstract»D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-31.
PubMed Abstract»D'Amico G, Morabito A, D'Amico M, et al. Clinical states of cirrhosis and competing risks. J Hepatol. 2018;68:563-576.
PubMed Abstract»D’Amico G, De Franchis R; Cooperative Study Group. Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology. 2003;38:599-612.
PubMed Abstract»Foster GR, Irving WL, Cheung MC, et al. Impact of direct acting antiviral therapy in patients with chronic hepatitis C and decompensated cirrhosis. J Hepatol. 2016;64:1224-31.
PubMed Abstract»Gadiparthi C, Cholankeril G, Perumpail BJ, et al. Use of direct-acting antiviral agents in hepatitis C virus-infected liver transplant candidates. World J Gastroenterol. 2018;24:315-322.
PubMed Abstract»Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335.
PubMed Abstract»Garcia-Tsao G, Lim JK; Members of Veterans Affairs Hepatitis C Resource Center Program. Management and treatment of patients with cirrhosis and portal hypertension: recommendations from the Department of Veterans Affairs Hepatitis C Resource Center Program and the National Hepatitis C Program. Am J Gastroenterol. 2009;104:1802-29.
PubMed Abstract»Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922-38.
AASLD Practice Guidelines»Garcia-Tsao G. Current management of the complications of cirrhosis and portal hypertension: variceal hemorrhage, ascites, and spontaneous bacterial peritonitis. Gastroenterology. 2001;120:726-48.
PubMed Abstract»Ge PS, Runyon BA. The changing role of beta-blocker therapy in patients with cirrhosis. J Hepatol. 2014;60:643-53.
PubMed Abstract»Haq I, Tripathi D. Recent advances in the management of variceal bleeding. Gastroenterol Rep (Oxf). 2017;5:113-126.
PubMed Abstract»Kaplan DE, Bosch J, Ripoll C, et al. AASLD practice guidance on risk stratification and management of portal hypertension and varices in cirrhosis. Hepatology. 2023 Oct 23. Online ahead of print.
PubMed Abstract»Krige JE, Kotze UK, Distiller G, Shaw JM, Bornman PC. Predictive factors for rebleeding and death in alcoholic cirrhotic patients with acute variceal bleeding: a multivariate analysis. World J Surg. 2009;33:2127-35.
PubMed Abstract»Mandorfer M, Bota S, Schwabl P, et al. Nonselective β blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology. 2014;146:1680-90.e1.
PubMed Abstract»Mandorfer M, Reiberger T. Beta blockers and cirrhosis, 2016. Dig Liver Dis. 2017;49:3-10.
PubMed Abstract»Manns M, Samuel D, Gane EJ, et al. Ledipasvir and sofosbuvir plus ribavirin in patients with genotype 1 or 4 hepatitis C virus infection and advanced liver disease: a multicentre, open-label, randomised, phase 2 trial. Lancet Infect Dis. 2016;16:685-97.
PubMed Abstract»Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144-65.
PubMed Abstract»Piano S, Singh V, Caraceni P, et al. Epidemiology and Effects of Bacterial Infections in Patients With Cirrhosis Worldwide. Gastroenterology. 2019;156:1368-80.
PubMed Abstract»Planas R, Ballesté B, Alvarez MA, et al. Natural history of decompensated hepatitis C virus-related cirrhosis. J Hepatol. 2004;40:823-30.
PubMed Abstract»Prakash R, Mullen KD. Mechanisms, diagnosis and management of hepatic encephalopathy. Nat Rev Gastroenterol Hepatol. 2010;7:515-25.
PubMed Abstract»Salerno F, Gerbes A, Ginès P, Wong F, Arroyo V. Diagnosis, prevention and treatment of hepatorenal syndrome in cirrhosis. Gut. 2007;56:1310-8.
PubMed Abstract»Shah N, Silva RG, Kowalski A, Desai C, Lerma E. Hepatorenal syndrome. Dis Mon. 2016;62:364-375.
PubMed Abstract»Wong F. The evolving concept of acute kidney injury in patients with cirrhosis. Nat Rev Gastroenterol Hepatol. 2015;12:711-9.
PubMed Abstract»Acharya C, Sahingur SE, Bajaj JS. Microbiota, cirrhosis, and the emerging oral-gut-liver axis. JCI Insight. 2017;2:e94416.
PubMed Abstract»Asselah T, Kowdley KV, Zadeikis N, et al. Efficacy of Glecaprevir/Pibrentasvir for 8 or 12 Weeks in Patients With Hepatitis C Virus Genotype 2, 4, 5, or 6 Infection Without Cirrhosis. Clin Gastroenterol Hepatol. 2018;16:417-26.
PubMed Abstract»Bini EJ, Bräu N, Currie S, et al. Prospective multicenter study of eligibility for antiviral therapy among 4,084 U.S. veterans with chronic hepatitis C virus infection. Am J Gastroenterol. 2005;100:1772-9.
PubMed Abstract»Cattau EL Jr, Benjamin SB, Knuff TE, Castell DO. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982;247:1164-6.
PubMed Abstract»D'Amico G, Morabito A, D'Amico M, et al. New concepts on the clinical course and stratification of compensated and decompensated cirrhosis. Hepatol Int. 2018;12:34-43.
PubMed Abstract»de Bruyn G, Graviss EA. A systematic review of the diagnostic accuracy of physical examination for the detection of cirrhosis. BMC Med Inform Decis Mak. 2001;1:6.
PubMed Abstract»Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599-607.
PubMed Abstract»Forns X, Lee SS, Valdes J, et al. Glecaprevir plus pibrentasvir for chronic hepatitis C virus genotype 1, 2, 4, 5, or 6 infection in adults with compensated cirrhosis (EXPEDITION-1): a single-arm, open-label, multicentre phase 3 trial. Lancet Infect Dis. 2017;17:1062-1068.
PubMed Abstract»Hézode C, Roudot-Thoraval F, Nguyen S, et al. Daily cannabis smoking as a risk factor for progression of fibrosis in chronic hepatitis C. Hepatology. 2005;42:63-71.
PubMed Abstract»Hajarizadeh B, Grebely J, Dore GJ. Epidemiology and natural history of HCV infection. Nat Rev Gastroenterol Hepatol. 2013;10:553-62.
PubMed Abstract»Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. Am Fam Physician.2006;74:756-62.
PubMed Abstract»Liang TJ, Rehermann B, Seeff LB, Hoofnagle JH. Pathogenesis, natural history, treatment, and prevention of hepatitis C. Ann Intern Med. 2000;132:296-305.
PubMed Abstract»Lingala S, Ghany MG. Natural History of Hepatitis C. Gastroenterol Clin North Am. 2015;44:717-34.
PubMed Abstract»Maier MM, He H, Schafer SD, Ward TT, Zaman A. Hepatitis C treatment eligibility among HIV-hepatitis C virus coinfected patients in Oregon: a population-based sample. AIDS Care. 2014;26:1178-85.
PubMed Abstract»Rinella ME, Lazarus JV, Ratziu V, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol. 2023;79:1542-56.
PubMed Abstract»Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015;313:2263-73.
PubMed Abstract»Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012;307:832-42.
PubMed Abstract»Wiley TE, McCarthy M, Breidi L, McCarthy M, Layden TJ. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology. 1998;28:805-9.
PubMed Abstract»Williams JW Jr, Simel DL. The rational clinical examination. Does this patient have ascites? How to divine fluid in the abdomen. JAMA. 1992;267:2645-8.
PubMed Abstract»Lesson 6. Surveillance for Hepatocellular Carcinoma
Epidemiology
Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol. 2009;27:1485-91.
PubMed Abstract»Axley P, Ahmed Z, Ravi S, Singal AK. Hepatitis C Virus and Hepatocellular Carcinoma: A Narrative Review. J Clin Transl Hepatol. 2018;6:79-84.
PubMed Abstract»Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020-2.
PubMed Abstract»Cao G, Liu J, Liu M. Global, Regional, and National Trends in Incidence and Mortality of Primary Liver Cancer and Its Underlying Etiologies from 1990 to 2019: Results from the Global Burden of Disease Study 2019. J Epidemiol Glob Health. 2023;13:344-60.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Hepatocellular carcinoma - United States, 2001-2006. MMWR Morb Mortal Wkly Rep. 2010;59:517-20.
CDC and MMWR»de Martel C, Maucort-Boulch D, Plummer M, Franceschi S. World-wide relative contribution of hepatitis B and C viruses in hepatocellular carcinoma. Hepatology. 2015;62:1190-200.
PubMed Abstract»Donato F, Tagger A, Gelatti U, et al. Alcohol and hepatocellular carcinoma: the effect of lifetime intake and hepatitis virus infections in men and women. Am J Epidemiol. 2002;155:323-31.
PubMed Abstract»El-Serag HB, Davila JA, Petersen NJ, McGlynn KA. The continuing increase in the incidence of hepatocellular carcinoma in the United States: an update. Ann Intern Med. 2003;139:817-23.
PubMed Abstract»El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterol. 2007;132:2557-76.
PubMed Abstract»El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142:1264-1273.e1.
PubMed Abstract»Hajarizadeh B, Grebely J, Dore GJ. Epidemiology and natural history of HCV infection. Nat Rev Gastroenterol Hepatol. 2013;10:553-62.
PubMed Abstract»Hedenstierna M, Nangarhari A, Weiland O, Aleman S. Diabetes and Cirrhosis Are Risk Factors for Hepatocellular Carcinoma After Successful Treatment of Chronic Hepatitis C. Clin Infect Dis. 2016;63:723-9.
PubMed Abstract»Innala E, Andersson C. Screening for hepatocellular carcinoma in acute intermittent porphyria: a 15-year follow-up in northern Sweden. J Intern Med. 2011;269:538-45.
PubMed Abstract»Ioannou GN, Splan MF, Weiss NS, McDonald GB, Beretta L, Lee SP. Incidence and predictors of hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol. 2007;5:938-45, 945.e1-4.
PubMed Abstract»Mitchell EL, Khan Z. Liver Disease in Alpha-1 Antitrypsin Deficiency: Current Approaches and Future Directions. Curr Pathobiol Rep. 2017;5:243-252.
PubMed Abstract»Momin BR, Pinheiro PS, Carreira H, Li C, Weir HK. Liver cancer survival in the United States by race and stage (2001-2009): Findings from the CONCORD-2 study. Cancer. 2017;123 Suppl 24:5059-5078.
PubMed Abstract»National Cancer Institute. Surveillance, Epidemiology, and End Results Program (SEER). Stat Facts: Liver and Intrahepatic Bile Duct Cancer
NCI»Njei B, Rotman Y, Ditah I, Lim JK. Emerging trends in hepatocellular carcinoma incidence and mortality. Hepatology. 2015;61:191-9.
PubMed Abstract»Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Recomm Rep. 2012;61:1-32.
PubMed Abstract»Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-49.
PubMed Abstract»Tanaka Y, Kurbanov F, Mano S, et al. Molecular tracing of the global hepatitis C virus epidemic predicts regional patterns of hepatocellular carcinoma mortality. Gastroenterology. 2006;130:703-14.
PubMed Abstract»Velázquez RF, Rodríguez M, Navascués CA, et al. Prospective analysis of risk factors for hepatocellular carcinoma in patients with liver cirrhosis. Hepatology. 2003;37:520-7.
PubMed Abstract»Villanueva A, Minguez B, Forner A, Reig M, Llovet JM. Hepatocellular carcinoma: novel molecular approaches for diagnosis, prognosis, and therapy. Annu Rev Med. 2010;61:317-28.
PubMed Abstract»White DL, Thrift AP, Kanwal F, Davila J, El-Serag HB. Incidence of Hepatocellular Carcinoma in All 50 United States, From 2000 Through 2012. Gastroenterology. 2017;152:812-820.e5.
PubMed Abstract»Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol. 2004;130:417-22.
PubMed Abstract»Benefit of HCC Surveillance with HCV Infection
Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020-2.
PubMed Abstract»Chen JG, Parkin DM, Chen QG, Lu JH, Shen QJ, Zhang BC, Zhu YR. Screening for liver cancer: results of a randomised controlled trial in Qidong, China. J Med Screen. 2003;10:204-9.
PubMed Abstract»Daher S, Massarwa M, Benson AA, Khoury T. Current and Future Treatment of Hepatocellular Carcinoma: An Updated Comprehensive Review. J Clin Transl Hepatol. 2018;6:69-78.
PubMed Abstract»Davila JA, Henderson L, Kramer JR, Kanwal F, Richardson PA, Duan Z, El-Serag HB. Utilization of surveillance for hepatocellular carcinoma among hepatitis C virus-infected veterans in the United States. Ann Intern Med. 2011;154:85-93.
PubMed Abstract»Di Bisceglie AM, Lyra AC, Schwartz M, et al. Hepatitis C-related hepatocellular carcinoma in the United States: influence of ethnic status. Am J Gastroenterol. 2003;98:2060-3.
PubMed Abstract»El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterol. 2007;132:2557-76.
PubMed Abstract»Fateen W, Ryder SD. Screening for hepatocellular carcinoma: patient selection and perspectives. J Hepatocell Carcinoma. 2017;4:71-9.
PubMed Abstract»Ioannou GN, Splan MF, Weiss NS, McDonald GB, Beretta L, Lee SP. Incidence and predictors of hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol. 2007;5:938-45, 945.e1-4.
PubMed Abstract»Kansagara D, Papak J, Pasha AS, et al. Screening for hepatocellular carcinoma in chronic liver disease: a systematic review. Ann Intern Med. 2014;161:261-9.
PubMed Abstract»Kanwal F, Kramer J, Asch SM, Chayanupatkul M, Cao Y, El-Serag HB. Risk of Hepatocellular Cancer in HCV Patients Treated With Direct-Acting Antiviral Agents. Gastroenterology. 2017;153:996-1005.e1.
PubMed Abstract»Lok AS, Seeff LB, Morgan TR, et al. Incidence of hepatocellular carcinoma and associated risk factors in hepatitis C related advanced liver disease. Gastroenterology. 2009;136:138-48.
PubMed Abstract»Przybyszewski EM, Chung RT. Unmet Needs in the Post-Direct-Acting Antiviral Era: Hepatocarcinogenesis After Hepatitis C Virus Eradication. J Infect Dis. 2023;228:S226-S231.
PubMed Abstract»Singal AG, Mittal S, Yerokun OA, et al. Hepatocellular Carcinoma Screening Associated with Early Tumor Detection and Improved Survival Among Patients with Cirrhosis in the US. Am J Med. 2017;130:1099-1106.e1.
PubMed Abstract»Singal AG, Pillai A, Tiro J. Early detection, curative treatment, and survival rates for hepatocellular carcinoma surveillance in patients with cirrhosis: a meta-analysis. PLoS Med. 2014;11:e1001624.
PubMed Abstract»Singal AG, Zhang E, Narasimman M, et al. HCC surveillance improves early detection, curative treatment receipt, and survival in patients with cirrhosis: A meta-analysis. J Hepatol. 2022;77:128-139.
PubMed Abstract»Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol. 2004;130:417-22.
PubMed Abstract»Indications for HCC Surveillance
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»Baumert TF, Jühling F, Ono A, Hoshida Y. Hepatitis C-related hepatocellular carcinoma in the era of new generation antivirals. BMC Med. 2017;15:52.
PubMed Abstract»Bruix J, Sherman M; Practice Guidelines Committee, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208-36.
PubMed Abstract»Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020-2.
PubMed Abstract»Davila JA, Henderson L, Kramer JR, Kanwal F, Richardson PA, Duan Z, El-Serag HB. Utilization of surveillance for hepatocellular carcinoma among hepatitis C virus-infected veterans in the United States. Ann Intern Med. 2011;154:85-93.
PubMed Abstract»de Martel C, Maucort-Boulch D, Plummer M, Franceschi S. World-wide relative contribution of hepatitis B and C viruses in hepatocellular carcinoma. Hepatology. 2015;62:1190-200.
PubMed Abstract»European Association for the Study of the Liver; European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908-43.
PubMed Abstract»Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-80.
PubMed Abstract»Institute of Medicine Report. “Hepatitis and Liver Cancer: A National Strategy for Prevention and Control of Hepatitis B and C.” January 11, 2010.
Institute of Medicine»Ioannou GN, Green PK, Berry K. HCV eradication induced by direct-acting antiviral agents reduces the risk of hepatocellular carcinoma. J Hepatol. 2017. pii: S0168-8278(17)32273-0.
PubMed Abstract»Konjeti VR, John BV. Interaction Between Hepatocellular Carcinoma and Hepatitis C Eradication With Direct-acting Antiviral Therapy. Curr Treat Options Gastroenterol. 2018;16:203-214.
PubMed Abstract»Lederle FA, Pocha C. Screening for liver cancer: the rush to judgment. Ann Intern Med. 2012;156:387-9.
PubMed Abstract»Li DK, Chung RT. Impact of hepatitis C virus eradication on hepatocellular carcinogenesis. Cancer. 2015;121:2874-82.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»PDQ® Screening and Prevention Editorial Board. PDQ Liver (Hepatocellular) Cancer Screening. Bethesda, MD: National Cancer Institute. Updated March 15, 2019.
National Cancer Institute»Sharma S, Khalili K, Nguyen GC. Non-invasive diagnosis of advanced fibrosis and cirrhosis. World J Gastroenterol. 2014;20:16820-30.
PubMed Abstract»Singal AG, Llovet JM, Yarchoan M, et al. AASLD Practice Guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology. 2023;78:1922-65.
AASLD»Talwalkar JA. Elastography for detecting hepatic fibrosis: options and considerations. Gastroenterology. 2008;135:299-302.
PubMed Abstract»Terrault NA, Lok ASF, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67:1560-99.
PubMed Abstract»Surveillance Testing Methods
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020-2.
PubMed Abstract»Carr BI, Pancoska P, Branch RA. Low alpha-fetoprotein hepatocellular carcinoma. J Gastroenterol Hepatol. 2010;25:1543-9.
PubMed Abstract»European Association for the Study of the Liver; European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908-43.
PubMed Abstract»Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-80.
PubMed Abstract»Lederle FA, Pocha C. Screening for liver cancer: the rush to judgment. Ann Intern Med. 2012;156:387-9.
PubMed Abstract»Leykum LK, El-Serag HB, Cornell J, Papadopoulos KP. Screening for hepatocellular carcinoma among veterans with hepatitis C on disease stage, treatment received, and survival. Clin Gastroenterol Hepatol. 2007;5:508-12.
PubMed Abstract»Liebman HA, Furie BC, Tong MJ, et al. Des-gamma-carboxy (abnormal) prothrombin as a serum marker of primary hepatocellular carcinoma. N Engl J Med. 1984;310:1427-31.
PubMed Abstract»Lok AS, Sterling RK, Everhart JE, et al. Des-gamma-carboxy prothrombin and alpha-fetoprotein as biomarkers for the early detection of hepatocellular carcinoma. Gastroenterology. 2010;138:493-502.
PubMed Abstract»Parikh A, Taouli B. Imaging of hepatocellular carcinoma: current concepts. Recent Results Cancer Res. 2013;190:33-55.
PubMed Abstract»Parikh ND, Singal AG, Hutton DW, Tapper EB. Cost-Effectiveness of Hepatocellular Carcinoma Surveillance: An Assessment of Benefits and Harms. Am J Gastroenterol. 2020;115:1642-9.
PubMed Abstract»Santi V, Trevisani F, Gramenzi A, et al. Semiannual surveillance is superior to annual surveillance for the detection of early hepatocellular carcinoma and patient survival. J Hepatol. 2010;53:291-7.
PubMed Abstract»Singal A, Volk ML, Waljee A, et al. Meta-analysis: surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis. Aliment Pharmacol Ther. 2009;30:37-47.
PubMed Abstract»Singal AG, Llovet JM, Yarchoan M, et al. AASLD Practice Guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology. 2023;78:1922-65.
AASLD»Stenflo J, Fernlund P, Egan W, Roepstorff P. Vitamin K dependent modifications of glutamic acid residues in prothrombin. Proc Natl Acad Sci U S A. 1974;71:2730-3.
PubMed Abstract»Tong MJ, Blatt LM, Kao VW. Surveillance for hepatocellular carcinoma in patients with chronic viral hepatitis in the United States of America. J Gastroenterol Hepatol. 2001;16:553-9.
PubMed Abstract»Trinchet JC, Chaffaut C, Bourcier V, et al. Ultrasonographic surveillance of hepatocellular carcinoma in cirrhosis: a randomized trial comparing 3- and 6-month periodicities. Hepatology. 2011;54:1987-97.
PubMed Abstract»Tzartzeva K, Obi J, Rich NE, et al. Surveillance Imaging and Alpha Fetoprotein for Early Detection of Hepatocellular Carcinoma in Patients With Cirrhosis: A Meta-analysis. Gastroenterology. 2018;154:1706-18.e1.
PubMed Abstract»Villanueva A, Minguez B, Forner A, Reig M, Llovet JM. Hepatocellular carcinoma: novel molecular approaches for diagnosis, prognosis, and therapy. Annu Rev Med. 2010;61:317-28.
PubMed Abstract»Wong RJ, Ahmed A, Gish RG. Elevated alpha-fetoprotein: differential diagnosis - hepatocellular carcinoma and other disorders. Clin Liver Dis. 2015;19:309-23.
PubMed Abstract»Guidance for HCC Surveillance
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»Bruix J, Sherman M; Practice Guidelines Committee, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208-36.
PubMed Abstract»Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020-2.
PubMed Abstract»Chen Q, Ayer T, Adee MG, Wang X, Kanwal F, Chhatwal J. Assessment of Incidence of and Surveillance Burden for Hepatocellular Carcinoma Among Patients With Hepatitis C in the Era of Direct-Acting Antiviral Agents. JAMA Netw Open. 2020;3:e2021173.
PubMed Abstract»Dalton-Fitzgerald E, Tiro J, Kandunoori P, Halm EA, Yopp A, Singal AG. Practice patterns and attitudes of primary care providers and barriers to surveillance of hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol. 2015;13:791-8.e1.
PubMed Abstract»Davila JA, Henderson L, Kramer JR, Kanwal F, Richardson PA, Duan Z, El-Serag HB. Utilization of surveillance for hepatocellular carcinoma among hepatitis C virus-infected veterans in the United States. Ann Intern Med. 2011;154:85-93.
PubMed Abstract»European Association for the Study of the Liver; European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908-43.
PubMed Abstract»Farvardin S, Patel J, Khambaty M, et al. Patient-reported barriers are associated with lower hepatocellular carcinoma surveillance rates in patients with cirrhosis. Hepatology. 2017;65:875-884.
PubMed Abstract»Goldberg DS, Taddei TH, Serper M, et al. Identifying barriers to hepatocellular carcinoma surveillance in a national sample of patients with cirrhosis. Hepatology. 2017;65:864-874.
PubMed Abstract»Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-80.
PubMed Abstract»Institute of Medicine Report. “Hepatitis and Liver Cancer: A National Strategy for Prevention and Control of Hepatitis B and C.” January 11, 2010.
Institute of Medicine»PDQ® Screening and Prevention Editorial Board. PDQ Liver (Hepatocellular) Cancer Screening. Bethesda, MD: National Cancer Institute. Updated March 15, 2019.
National Cancer Institute»Singal AG, Llovet JM, Yarchoan M, et al. AASLD Practice Guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology. 2023;78:1922-65.
AASLD»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»Arslanoglu A, Seyal AR, Sodagari F, et al. Current Guidelines for the Diagnosis and Management of Hepatocellular Carcinoma: A Comparative Review. AJR Am J Roentgenol. 2016;207:W88-W98.
PubMed Abstract»Borel F, Konstantinova P, Jansen PL. Diagnostic and therapeutic potential of miRNA signatures in patients with hepatocellular carcinoma. J Hepatol. 2012;56:1371-83.
PubMed Abstract»Calvaruso V, Cabibbo G, Cacciola I, et al. Incidence of Hepatocellular Carcinoma in Patients With HCV-Associated Cirrhosis Treated With Direct-Acting Antiviral Agents. Gastroenterology. 2018;155:411-21.e4.
PubMed Abstract»Donato F, Tagger A, Gelatti U, et al. Alcohol and hepatocellular carcinoma: the effect of lifetime intake and hepatitis virus infections in men and women. Am J Epidemiol. 2002;155:323-31.
PubMed Abstract»El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterol. 2007;132:2557-76.
PubMed Abstract»Girotra M, Soota K, Dhaliwal AS, Abraham RR, Garcia-Saenz-de-Sicilia M, Tharian B. Utility of endoscopic ultrasound and endoscopy in diagnosis and management of hepatocellular carcinoma and its complications: What does endoscopic ultrasonography offer above and beyond conventional cross-sectional imaging? World J Gastrointest Endosc. 2018;10:56-68.
PubMed Abstract»Hajarizadeh B, Grebely J, Dore GJ. Epidemiology and natural history of HCV infection. Nat Rev Gastroenterol Hepatol. 2013;10:553-62.
PubMed Abstract»Li L, Guo Z, Wang J, Mao Y, Gao Q. Serum miR-18a: a potential marker for hepatitis B virus-related hepatocellular carcinoma screening. Dig Dis Sci. 2012;57:2910-6.
PubMed Abstract»Marrero JA, Feng Z, Wang Y, et al. Alpha-fetoprotein, des-gamma carboxyprothrombin, and lectin-bound alpha-fetoprotein in early hepatocellular carcinoma. Gastroenterology. 2009;137:110-8.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Nahon P, Bourcier V, Layese R, et al. Eradication of Hepatitis C Virus Infection in Patients With Cirrhosis Reduces Risk of Liver and Non-Liver Complications. Gastroenterology. 2017;152:142-56.e2.
PubMed Abstract»Sharma S, Khalili K, Nguyen GC. Non-invasive diagnosis of advanced fibrosis and cirrhosis. World J Gastroenterol. 2014;20:16820-30.
PubMed Abstract»Talwalkar JA. Elastography for detecting hepatic fibrosis: options and considerations. Gastroenterology. 2008;135:299-302.
PubMed Abstract»Tang A, Hallouch O, Chernyak V, Kamaya A, Sirlin CB. Epidemiology of hepatocellular carcinoma: target population for surveillance and diagnosis. Abdom Radiol (NY). 2018;43:13-25.
PubMed Abstract»Tran SA, Le A, Zhao C, et al. Rate of hepatocellular carcinoma surveillance remains low for a large, real-life cohort of patients with hepatitis C cirrhosis. BMJ Open Gastroenterol. 2018;5:e000192.
PubMed Abstract»Yu NC, Chaudhari V, Raman SS, et al. CT and MRI improve detection of hepatocellular carcinoma, compared with ultrasound alone, in patients with cirrhosis. Clin Gastroenterol Hepatol. 2011;9:161-7.
PubMed Abstract»Zhou J, Yu L, Gao X, et al. Plasma microRNA panel to diagnose hepatitis B virus-related hepatocellular carcinoma. J Clin Oncol. 2011;29:4781-8.
PubMed Abstract»Lesson 7. Extrahepatic Conditions Related to HCV Infection
Overview of Extrahepatic Manifestations
Cacoub P, Buggisch P, Carrión JA, et al. Direct medical costs associated with the extrahepatic manifestations of hepatitis C infection in Europe. J Viral Hepat. 2018;25:811-17.
PubMed Abstract»Cacoub P, Poynard T, Ghillani P, et al. Extrahepatic manifestations of chronic hepatitis C. MULTIVIRC Group. Multidepartment Virus C. Arthritis Rheum. 1999;42:2204-12.
PubMed Abstract»Cacoub P, Renou C, Rosenthal E, et al. Extrahepatic manifestations associated with hepatitis C virus infection. A prospective multicenter study of 321 patients. The GERMIVIC. Groupe d'Etude et de Recherche en Medecine Interne et Maladies Infectieuses sur le Virus de l'Hepatite C. Medicine (Baltimore). 2000;79:47-56.
PubMed Abstract»Cacoub P, Saadoun D. Extrahepatic Manifestations of Chronic HCV Infection. N Engl J Med. 2021;384:1038-52.
PubMed Abstract»Dalrymple LS, Koepsell T, Sampson J, Louie T, Dominitz JA, Young B, Kestenbaum B. Hepatitis C virus infection and the prevalence of renal insufficiency. Clin J Am Soc Nephrol. 2007;2:715-21.
PubMed Abstract»El-Serag HB, Hampel H, Yeh C, Rabeneck L. Extrahepatic manifestations of hepatitis C among United States male veterans. Hepatology. 2002;36:1439-45.
PubMed Abstract»Giordano TP, Henderson L, Landgren O, Chiao EY, Kramer JR, El-Serag H, Engels EA. Risk of non-Hodgkin lymphoma and lymphoproliferative precursor diseases in US veterans with hepatitis C virus. JAMA 2007;297:2010-7.
PubMed Abstract»Gumber SC, Chopra S. Hepatitis C: a multifaceted disease. Review of extrahepatic manifestations. Ann Intern Med. 1995 Oct 15;123(8):615-20. Ann Intern Med. 1995;123:615-20.
PubMed Abstract»Jacobson IM, Cacoub P, Dal Maso L, Harrison SA, Younossi ZM. Manifestations of chronic hepatitis C virus infection beyond the liver. Clin Gastroenterol Hepatol. 2010;8:1017-29.
PubMed Abstract»Lodi G, Pellicano R, Carrozzo M. Hepatitis C virus infection and lichen planus: a systematic review with meta-analysis. Oral Dis. 2010;16:601-12.
PubMed Abstract»Negro F, Forton D, Craxì A, Sulkowski MS, Feld JJ, Manns MP. Extrahepatic morbidity and mortality of chronic hepatitis C. Gastroenterology. 2015;149:1345-60.
PubMed Abstract»Petti S, Rabiei M, De Luca M, Scully C. The magnitude of the association between hepatitis C virus infection and oral lichen planus: meta-analysis and case control study. Odontology. 2011;99:168-78.
PubMed Abstract»Sherman AC, Sherman KE. Extrahepatic manifestations of hepatitis C infection: navigating CHASM. Curr HIV/AIDS Rep. 2015;12:353-61.
PubMed Abstract»Songtanin B, Nugent K. Burden, Outcome, and Comorbidities of Extrahepatic Manifestations in Hepatitis C Virus Infection. Biology (Basel). 2022;12:23
PubMed Abstract»Tang L, Marcell L, Kottilil S. Systemic manifestations of hepatitis C infection. Infect Agent Cancer. 2016;11:29.
PubMed Abstract»Tsui JI, Vittinghoff E, Shlipak MG, Bertenthal D, Inadomi J, Rodriguez RA, O'Hare AM. Association of hepatitis C seropositivity with increased risk for developing end-stage renal disease. Arch Intern Med. 2007;167:1271-6.
PubMed Abstract»Younossi Z, Park H, Henry L, Adeyemi A, Stepanova M. Extrahepatic Manifestations of Hepatitis C: A Meta-analysis of Prevalence, Quality of Life, and Economic Burden. Gastroenterology. 2016;150:1599-1608.
PubMed Abstract»Zignego AL, Ferri C, Pileri SA, Caini P, Bianchi FB; Italian Association of the Study of Liver Commission on Extrahepatic Manifestations of HCV infection. Extrahepatic manifestations of hepatitis C virus infection: a general overview and guidelines for a clinical approach. Dig Liver Dis. 2007;39:2-17.
PubMed Abstract»Cryoglobulinemia
Agnello V, Chung RT, Kaplan LM. A role for hepatitis C virus infection in type II cryoglobulinemia. N Engl J Med. 1992;327:1490-5.
PubMed Abstract»Brouet JC, Clauvel JP, Danon F, Klein M, Seligmann M. Biologic and clinical significance of cryoglobulins. A report of 86 cases. Am J Med. 1974;57:775-88.
PubMed Abstract»Cacoub P, Comarmond C, Vieira M, Régnier P, Saadoun D. HCV-related lymphoproliferative disorders in the direct-acting antiviral era: From mixed cryoglobulinaemia to B-cell lymphoma. J Hepatol. 2022;76:174-85.
PubMed Abstract»Dammacco F, Lauletta G, Vacca A. The wide spectrum of cryoglobulinemic vasculitis and an overview of therapeutic advancements. Clin Exp Med. 2023;23:255-72.
PubMed Abstract»Dammacco F, Sansonno D. Therapy for hepatitis C virus-related cryoglobulinemic vasculitis. N Engl J Med. 2013;369:1035-45.
PubMed Abstract»Danishwar M, Jamil Z, Khan S, et al. Persistence of Cryoglobulinemic Vasculitis after DAA Induced HCV Cure. J Clin Med. 2022;11::984.
PubMed Abstract»David WS, Peine C, Schlesinger P, Smith SA. Nonsystemic vasculitic mononeuropathy multiplex, cryoglobulinemia, and hepatitis C. Muscle Nerve 1996;19:1596-602.
PubMed Abstract»De Vita S, Quartuccio L, Isola M, et al. A randomized controlled trial of rituximab for the treatment of severe cryoglobulinemic vasculitis. Arthritis Rheum. 2012;64:843-53.
PubMed Abstract»Emery JS, Kuczynski M, La D, et al. Efficacy and Safety of Direct Acting Antivirals for the Treatment of Mixed Cryoglobulinemia. Am J Gastroenterol. 2017;112:1298-1308.
PubMed Abstract»Iannuzzella F, Vaglio A, Garini G. Management of hepatitis C virus-related mixed cryoglobulinemia. Am J Med. 2010;123:400-8.
PubMed Abstract»Mahale P, Engels EA, Li R, et al. The effect of sustained virological response on the risk of extrahepatic manifestations of hepatitis C virus infection. Gut. 2018;67:553-561.
PubMed Abstract»Mazzaro C, Quartuccio L, Adinolfi LE, et al. A Review on Extrahepatic Manifestations of Chronic Hepatitis C Virus Infection and the Impact of Direct-Acting Antiviral Therapy. Viruses. 2021;13:2249.
PubMed Abstract»Misiani R, Bellavita P, Fenili D, et al. Hepatitis C virus infection in patients with essential mixed cryoglobulinemia. Ann Intern Med. 1992;117:573-7.
PubMed Abstract»Misiani R, Bellavita P, Fenili D, et al. Interferon alfa-2a therapy in cryoglobulinemia associated with hepatitis C virus. N Engl J Med. 1994;330:751-6.
PubMed Abstract»Moretti M, Ferro F, Baldini C, Mosca M, Talarico R. Cryoglobulinemic vasculitis: a 2023 update. Curr Opin Rheumatol. 2024;36:27-34.
PubMed Abstract»Ragab G, Hussein MA. Vasculitic syndromes in hepatitis C virus: A review. J Adv Res. 2017;8:99-111.
PubMed Abstract»Ramos-Casals M, Stone JH, Cid MC, Bosch X. The cryoglobulinaemias. Lancet. 2012;379:348-60.
PubMed Abstract»Roccatello D, Sciascia S, Rossi D, et al. The challenge of treating hepatitis C virus-associated cryoglobulinemic vasculitis in the era of anti-CD20 monoclonal antibodies and direct antiviral agents. Oncotarget. 2017 ;8:41764-41777.
PubMed Abstract»Rutledge SM, Chung RT, Sise ME. Treatment of hepatitis C virus infection in patients with mixed cryoglobulinemic syndrome and cryoglobulinemic glomerulonephritis. Hemodial Int. 2018;22 Suppl 1:S81-S96.
PubMed Abstract»Saadoun D, Delluc A, Piette JC, Cacoub P. Treatment of hepatitis C-associated mixed cryoglobulinemia vasculitis. Curr Opin Rheumatol. 2008;20:23-8.
PubMed Abstract»Saadoun D, Resche Rigon M, Sene D, et al. Rituximab plus Peg-interferon-alpha/ribavirin compared with Peg-interferon-alpha/ribavirin in hepatitis C-related mixed cryoglobulinemia. Blood. 2010;116:326-34.
PubMed Abstract»Sansonno D, Dammacco F. Hepatitis C virus, cryoglobulinemia, and vasculitis: immune complex relations. Lancet Infect Dis. 2005;5:227-36.
PubMed Abstract»Autoimmune Disorders
Antonelli A, Ferri C, Pampana A, et al. Thyroid disorders in chronic hepatitis C. Am J Med. 2004;117:10-3.
PubMed Abstract»Bianchi FB. Autoimmune hepatitis: the lesson of the discovery of hepatitis C virus. J Hepatol. 1993;18:273-5.
PubMed Abstract»Cacoub P, Musset L, Amoura Z, et al. Anticardiolipin, anti-beta2-glycoprotein I, and antinucleosome antibodies in hepatitis C virus infection and mixed cryoglobulinemia. Multivirc Group. J Rheumatol. 1997;24:2139-44.
PubMed Abstract»Cacoub P, Renou C, Rosenthal E, et al. Extrahepatic manifestations associated with hepatitis C virus infection. A prospective multicenter study of 321 patients. The GERMIVIC. Groupe d'Etude et de Recherche en Medecine Interne et Maladies Infectieuses sur le Virus de l'Hepatite C. Medicine (Baltimore). 2000;79:47-56.
PubMed Abstract»Clifford BD, Donahue D, Smith L, et al. High prevalence of serological markers of autoimmunity in patients with chronic hepatitis C. Hepatology. 1995;21:613-9.
PubMed Abstract»Haddad J, Deny P, Munz-Gotheil C, et al. Lymphocytic sialadenitis of Sjögren's syndrome associated with chronic hepatitis C virus liver disease. Lancet. 1992;339:321-3.
PubMed Abstract»Monti V, Aghemo A, Rumi MG, Donato MF, Del Ninno E, Colombo M. The prevalence, clinical features and response to antiviral therapy of patients with chronic hepatitis C who are seropositive for liver-kidney microsome type 1 antibodies. Antivir Ther. 2005;10:715-20.
PubMed Abstract»Ramos-Casals M, Muñoz S, Medina F, et al. Systemic autoimmune diseases in patients with hepatitis C virus infection: characterization of 1020 cases (The HISPAMEC Registry). J Rheumatol. 2009;36:1442-8.
PubMed Abstract»Reddy KR, Krawitt EL, Homberg JC, et al. Absence of anti-LKM-1 antibody in hepatitis C viral infection in the United States of America. J Viral Hepat. 1995;2:175-9.
PubMed Abstract»Tran A, Quaranta JF, Benzaken S, et al. High prevalence of thyroid autoantibodies in a prospective series of patients with chronic hepatitis C before interferon therapy. Hepatology. 1993;18:253-7.
PubMed Abstract»Wang Y, Dou H, Liu G, et al. Hepatitis C virus infection and the risk of Sjögren or sicca syndrome: a meta-analysis. Microbiol Immunol. 2014;58:675-87.
PubMed Abstract»Younossi Z, Park H, Henry L, Adeyemi A, Stepanova M. Extrahepatic Manifestations of Hepatitis C: A Meta-analysis of Prevalence, Quality of Life, and Economic Burden. Gastroenterology. 2016;150:1599-1608.
PubMed Abstract»Renal Disorders
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with renal impairment.
AASLD-IDSA Hepatitis C Guidance»Awan AAY, Berenguer MC, Bruchfeld A, et al. Prevention, Diagnosis, Evaluation, and Treatment of Hepatitis C in Chronic Kidney Disease: Synopsis of the Kidney Disease: Improving Global Outcomes 2022 Clinical Practice Guideline. Ann Intern Med. 2023;176:1648-55.
PubMed Abstract»Castillo I, Martinez-Ara J, Olea T, et al. High prevalence of occult hepatitis C virus infection in patients with primary and secondary glomerular nephropathies. Kidney Int. 2014;86:619-24.
PubMed Abstract»Dalrymple LS, Koepsell T, Sampson J, Louie T, Dominitz JA, Young B, Kestenbaum B. Hepatitis C virus infection and the prevalence of renal insufficiency. Clin J Am Soc Nephrol. 2007;2:715-21.
PubMed Abstract»Fabrizi F, Messa P, Martin P. Novel evidence on hepatitis C virus-associated glomerular disease. Kidney Int. 2014;86:466-9.
PubMed Abstract»Fabrizi F, Verdesca S, Messa P, Martin P. Hepatitis C Virus Infection Increases the Risk of Developing Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Dig Dis Sci. 2015;60:3801-13.
PubMed Abstract»Ferri C, Giuggioli D, Colaci M. Renal Manifestations of Hepatitis C Virus. Clin Liver Dis. 2017;21:487-497.
PubMed Abstract»Johnson RJ, Gretch DR, Yamabe H, et al. Membranoproliferative glomerulonephritis associated with hepatitis C virus infection. N Engl J Med. 1993;328:465-70.
PubMed Abstract»Kamar N, Rostaing L, Alric L. Treatment of hepatitis C virus-related glomerulonephritis. Kidney Int. 2006;69:436-9.
PubMed Abstract»Kidney Disease: Improving Global Outcomes (KDIGO). KDIGO clinical practice guidelines for the prevention, diagnosis, evaluation and treatment of hepatitis C in chronic kidney disease. Kidney Int Suppl. 2008;(109):S1-S99.
Kidney International»Latt N, Alachkar N, Gurakar A. Hepatitis C virus and its renal manifestations: a review and update. Gastroenterol Hepatol (N Y). 2012;8:434-45.
PubMed Abstract»Liangpunsakul S, Chalasani N. Relationship between hepatitis C and microalbuminuria: results from the NHANES III. Kidney Int. 2005;67:285-90.
PubMed Abstract»Morales JM, Kamar N, Rostaing L. Hepatitis C and renal disease: epidemiology, diagnosis, pathogenesis and therapy. Contrib Nephrol. 2012;176:10-23.
PubMed Abstract»Moyer VA; U.S. Preventive Services Task Force. Screening for hepatitis C virus infection in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:51-60.
PubMed Abstract»Pérez de José A, Carbayo J, Pocurull A, et al. Direct-acting antiviral therapy improves kidney survival in hepatitis C virus-associated cryoglobulinaemia: the RENALCRYOGLOBULINEMIC study. Clin Kidney J. 2021;14:586-92.
PubMed Abstract»Park H, Wang W, Henry L, Nelson DR. Impact of All-Oral Direct-Acting Antivirals on Clinical and Economic Outcomes in Patients With Chronic Hepatitis C in the United States. Hepatology. 2019;69:1032-45.
PubMed Abstract»Roccatello D, Fornasieri A, Giachino O, et al. Multicenter study on hepatitis C virus-related cryoglobulinemic glomerulonephritis. Am J Kidney Dis. 2007;49:69-82.
PubMed Abstract»Roccatello D, Sciascia S, Rossi D, et al. The challenge of treating hepatitis C virus-associated cryoglobulinemic vasculitis in the era of anti-CD20 monoclonal antibodies and direct antiviral agents. Oncotarget. 2017 ;8:41764-41777.
PubMed Abstract»Söderholm J, Millbourn C, Büsch K, et al. Higher risk of renal disease in chronic hepatitis C patients: Antiviral therapy survival benefit in patients on hemodialysis. J Hepatol. 2018;68:904-11.
PubMed Abstract»Saadoun D, Resche Rigon M, Sene D, et al. Rituximab plus Peg-interferon-alpha/ribavirin compared with Peg-interferon-alpha/ribavirin in hepatitis C-related mixed cryoglobulinemia. Blood. 2010;116:326-34.
PubMed Abstract»Sabry AA, Sobh MA, Irving WL, et al. A comprehensive study of the association between hepatitis C virus and glomerulopathy. Nephrol Dial Transplant. 2002;17:239-45.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Tsui JI, Vittinghoff E, Shlipak MG, Bertenthal D, Inadomi J, Rodriguez RA, O'Hare AM. Association of hepatitis C seropositivity with increased risk for developing end-stage renal disease. Arch Intern Med. 2007;167:1271-6.
PubMed Abstract»Tsui JI, Vittinghoff E, Shlipak MG, O’Hare AM. Relationship between hepatitis C and chronic kidney disease: results from the Third National Health and Nutrition Examination Survey. J Am Soc Nephrol. 2006;17:1168-74.
PubMed Abstract»Yamabe H, Johnson RJ, Gretch DR, et al. Hepatitis C virus infection and membranoproliferative glomerulonephritis in Japan. J Am Soc Nephrol. 1995;6:220-3.
PubMed Abstract»Younossi Z, Park H, Henry L, Adeyemi A, Stepanova M. Extrahepatic Manifestations of Hepatitis C: A Meta-analysis of Prevalence, Quality of Life, and Economic Burden. Gastroenterology. 2016;150:1599-1608.
PubMed Abstract»Dermatologic Manifestations
Ashton RE, Hawk JL, Magnus IA. Low-dose oral chloroquine in the treatment of porphyria cutanea tarda. Br J Dermatol. 1984;111:609-13.
PubMed Abstract»Berk DR, Mallory SB, Keeffe EB, Ahmed A. Dermatologic disorders associated with chronic hepatitis C: effect of interferon therapy. Clin Gastroenterol Hepatol 2007;5:142.
PubMed Abstract»David WS, Peine C, Schlesinger P, Smith SA. Nonsystemic vasculitic mononeuropathy multiplex, cryoglobulinemia, and hepatitis C. Muscle Nerve 1996;19:1596-602.
PubMed Abstract»Dedania B, Wu GY. Dermatologic Extrahepatic Manifestations of Hepatitis C. J Clin Transl Hepatol. 2015;3:127-33.
PubMed Abstract»Fargion S, Piperno A, Capellini MD, et al. Hepatitis C virus and porphyria cutanea tarda: evidence of a strong association. Hepatology 1992;16:1322-6.
PubMed Abstract»Gisbert JP, García-Buey L, Pajares JM, Moreno-Otero R. Prevalence of hepatitis C virus infection in porphyria cutanea tarda: systematic review and meta-analysis. J Hepatol 2003;39:620-7.
PubMed Abstract»Hatch MM, Nawas Z, Kollipara R, Tyring SK. Can curative antivirals benefit porphyria cutanea tarda in hepatitis C patients? J Eur Acad Dermatol Venereol. 2017;31:e194.
PubMed Abstract»Le Cleach L, Chosidow O. Clinical practice. Lichen planus. N Engl J Med. 2012;366:723-32.
PubMed Abstract»Lodi G, Pellicano R, Carrozzo M. Hepatitis C virus infection and lichen planus: a systematic review with meta-analysis. Oral Dis. 2010;16:601-12.
PubMed Abstract»Misaka K, Kishimoto T, Kawahigashi Y, Sata M, Nagao Y. Use of Direct-Acting Antivirals for the Treatment of Hepatitis C Virus-Associated Oral Lichen Planus: A Case Report. Case Rep Gastroenterol. 2016;10:617-622.
PubMed Abstract»Nagao Y, Kimura K, Kawahigashi Y, Sata M. Successful Treatment of Hepatitis C Virus-associated Oral Lichen Planus by Interferon-free Therapy with Direct-acting Antivirals. Clin Transl Gastroenterol. 2016;7:e179.
PubMed Abstract»Okano J, Horie Y, Kawasaki H, Kondo M. Interferon treatment of porphyria cutanea tarda associated with chronic hepatitis type C. Hepatogastroenterology 1997;44:525-8.
PubMed Abstract»Petti S, Rabiei M, De Luca M, Scully C. The magnitude of the association between hepatitis C virus infection and oral lichen planus: meta-analysis and case control study. Odontology. 2011;99:168-78.
PubMed Abstract»Pilli M, Penna A, Zerbini A, et al. Oral lichen planus pathogenesis: A role for the HCV-specific cellular immune response. Hepatology 2002;36:1446-52.
PubMed Abstract»Sayiner M, Golabi P, Farhat F, Younossi ZM. Dermatologic Manifestations of Chronic Hepatitis C Infection. Clin Liver Dis. 2017;21:555-564.
PubMed Abstract»Sherman AC, Sherman KE. Extrahepatic manifestations of hepatitis C infection: navigating CHASM. Curr HIV/AIDS Rep. 2015;12:353-61.
PubMed Abstract»Singal AK, Kormos-Hallberg C, Lee C, et al. Low-dose hydroxychloroquine is as effective as phlebotomy in treatment of patients with porphyria cutanea tarda. Clin Gastroenterol Hepatol. 2012;10:1402-9.
PubMed Abstract»To-Figueras J. Association between hepatitis C virus and porphyria cutanea tarda. Mol Genet Metab. 2019 Nov;128:282-287.
PubMed Abstract»Tong Y, Song YK, Tyring S. Resolution of Porphyria Cutanea Tarda in Patients With Hepatitis C Following Ledipasvir-Sofosbuvir Combination Therapy. JAMA Dermatol. 2016;152:1393-1395.
PubMed Abstract»Wiznia LE, Laird ME, Franks AG Jr. Hepatitis C virus and its cutaneous manifestations: treatment in the direct-acting antiviral era. J Eur Acad Dermatol Venereol. 2017;31:1260-1270.
PubMed Abstract»Insulin Resistance and Type 2 Diabetes
Arase Y, Suzuki F, Suzuki Y, et al. Sustained virological response reduces incidence of onset of type 2 diabetes in chronic hepatitis C. Hepatology. 2009;49:739-44.
PubMed Abstract»Bose SK, Ray R. Hepatitis C virus infection and insulin resistance. World J Diabetes. 2014;5:52-8.
PubMed Abstract»Butt AA, Yan P, Aslam S, Shaikh OS, Abou-Samra AB. Hepatitis C Virus (HCV) Treatment With Directly Acting Agents Reduces the Risk of Incident Diabetes: Results From Electronically Retrieved Cohort of HCV Infected Veterans (ERCHIVES). Clin Infect Dis. 2020;70:1153-60.
PubMed Abstract»Cacoub P, Desbois AC, Comarmond C, Saadoun D. Impact of sustained virological response on the extrahepatic manifestations of chronic hepatitis C: a meta-analysis. Gut. 2018;67:2025-34.
PubMed Abstract»Chaudhury CS, Sheehan J, Chairez C, et al. No Improvement in Hemoglobin A1c Following Hepatitis C Viral Clearance in Patients With and Without HIV. J Infect Dis. 2017;217:47-50.
PubMed Abstract»Doyle MA, Singer J, Lee T, Muir M, Cooper C. Improving treatment and liver fibrosis outcomes with metformin in HCV-HIV co-infected and HCV mono-infected patients with insulin resistance: study protocol for a randomized controlled trial. Trials. 2016;17:331.
PubMed Abstract»Fabiani S, Fallahi P, Ferrari SM, Miccoli M, Antonelli A. Hepatitis C virus infection and development of type 2 diabetes mellitus: Systematic review and meta-analysis of the literature. Rev Endocr Metab Disord. 2018;19:405-20.
PubMed Abstract»Giordanino C, Bugianesi E, Smedile A, et al. Incidence of type 2 diabetes mellitus and glucose abnormalities in patients with chronic hepatitis C infection by response to treatment: results of a cohort study. Am J Gastroenterol. 2008;103:2481-7.
PubMed Abstract»Hanouneh IA, Feldstein AE, Lopez R, Yerian L, Pillai A, Zein CO, Zein NN. Clinical significance of metabolic syndrome in the setting of chronic hepatitis C virus infection. Clin Gastroenterol Hepatol. 2008;6:584-9.
PubMed Abstract»Harrison SA, Hamzeh FM, Han J, Pandya PK, Sheikh MY, Vierling JM. Chronic hepatitis C genotype 1 patients with insulin resistance treated with pioglitazone and peginterferon alpha-2a plus ribavirin. Hepatology. 2012;56:464-73.
PubMed Abstract»Hickman IJ, Clouston AD, Macdonald GA, et al. Effect of weight reduction on liver histology and biochemistry in patients with chronic hepatitis C. Gut. 2002;51:89-94.
PubMed Abstract»Hui JM, Sud A, Farrell GC, et al. Insulin resistance is associated with chronic hepatitis C virus infection and fibrosis progression. Gastroenterology. 2003;125:1695-704.
PubMed Abstract»Kaddai V, Negro F. Current understanding of insulin resistance in hepatitis C. Expert Rev Gastroenterol Hepatol. 2011;5:503-16.
PubMed Abstract»Milner KL, van der Poorten D, Trenell M, et al. Chronic hepatitis C is associated with peripheral rather than hepatic insulin resistance. Gastroenterology. 2010;138:932-41.e1-3.
PubMed Abstract»Moucari R, Asselah T, Cazals-Hatem D, et al. Insulin resistance in chronic hepatitis C: association with genotypes 1 and 4, serum HCV RNA level, and liver fibrosis. Gastroenterology. 2008;134:416-23.
PubMed Abstract»Negro F, Alaei M. Hepatitis C virus and type 2 diabetes. World J Gastroenterol. 2009;15:1537-47.
PubMed Abstract»Negro F, Forton D, Craxì A, Sulkowski MS, Feld JJ, Manns MP. Extrahepatic morbidity and mortality of chronic hepatitis C. Gastroenterology. 2015;149:1345-60.
PubMed Abstract»Negro F. Mechanisms of hepatitis C virus-related insulin resistance. Clin Res Hepatol Gastroenterol. 2011;35:358-63.
PubMed Abstract»Ribaldone DG, Sacco M, Saracco GM. The Effect of Viral Clearance Achieved by Direct-Acting Antiviral Agents on Hepatitis C Virus Positive Patients with Type 2 Diabetes Mellitus: A Word of Caution after the Initial Enthusiasm. J Clin Med. 2020;9:563.
PubMed Abstract»Romero-Gómez M, Diago M, Andrade RJ, et al. Treatment of insulin resistance with metformin in naïve genotype 1 chronic hepatitis C patients receiving peginterferon alfa-2a plus ribavirin. Hepatology. 2009;50:1702-8.
PubMed Abstract»Sacco M, Saracco GM. The impact of direct-acting antiviral treatment on glycemic homeostasis in patients with chronic hepatitis C. Minerva Gastroenterol (Torino). 2021;67:264-72.
PubMed Abstract»Serfaty L, Forns X, Goeser T, et al. Insulin resistance and response to telaprevir plus peginterferon α and ribavirin in treatment-naive patients infected with HCV genotype 1. Gut. 2012;61:1473-80.
PubMed Abstract»Sherman AC, Sherman KE. Extrahepatic manifestations of hepatitis C infection: navigating CHASM. Curr HIV/AIDS Rep. 2015;12:353-61.
PubMed Abstract»Wang CS, Wang ST, Yao WJ, Chang TT, Chou P. Hepatitis C virus infection and the development of type 2 diabetes in a community-based longitudinal study. Am J Epidemiol. 2007;166:196-203.
PubMed Abstract»White DL, Ratziu V, El-Serag HB. Hepatitis C infection and risk of diabetes: a systematic review and meta-analysis. J Hepatol. 2008;49:831-44.
PubMed Abstract»Lymphomas
Alric L, Besson C, Lapidus N, et al. Antiviral Treatment of HCV-Infected Patients with B-Cell Non-Hodgkin Lymphoma: ANRS HC-13 Lympho-C Study. PLoS One. 2016;11:e0162965.
PubMed Abstract»Arcaini L, Bruno R. Hepatitis C virus infection and antiviral treatment in marginal zone lymphomas. Curr Clin Pharmacol. 2010;5:74-81.
PubMed Abstract»Armand M, Besson C, Hermine O, Davi F. Hepatitis C virus - Associated marginal zone lymphoma. Best Pract Res Clin Haematol. 2017;30:41-49.
PubMed Abstract»Chen TT, Chiu CF, Yang TY, et al. Hepatitis C infection is associated with hepatic toxicity but does not compromise the survival of patients with diffuse large B cell lymphoma treated with rituximab-based chemotherapy. Leuk Res. 2015;39:151-6.
PubMed Abstract»Dal Maso L, Franceschi S. Hepatitis C virus and risk of lymphoma and other lymphoid neoplasms: a meta-analysis of epidemiologic studies. Cancer Epidemiol Biomarkers Prev. 2006;15:2078-85.
PubMed Abstract»Ennishi D, Maeda Y, Niitsu N, et al. Hepatic toxicity and prognosis in hepatitis C virus-infected patients with diffuse large B-cell lymphoma treated with rituximab-containing chemotherapy regimens: a Japanese multicenter analysis. Blood. 2010;116:5119-25.
PubMed Abstract»Ferri C, Sebastiani M, Giuggioli D, et al. Mixed cryoglobulinemia: demographic, clinical, and serologic features and survival in 231 patients. Semin Arthritis Rheum. 2004;33:355-74.
PubMed Abstract»Giordano TP, Henderson L, Landgren O, Chiao EY, Kramer JR, El-Serag H, Engels EA. Risk of non-Hodgkin lymphoma and lymphoproliferative precursor diseases in US veterans with hepatitis C virus. JAMA 2007;297:2010-7.
PubMed Abstract»Gisbert JP, García-Buey L, Pajares JM, Moreno-Otero R. Prevalence of hepatitis C virus infection in B-cell non-Hodgkin's lymphoma: systematic review and meta-analysis. Gastroenterology. 2003;125:1723-32.
PubMed Abstract»Hartridge-Lambert SK, Stein EM, Markowitz AJ, Portlock CS. Hepatitis C and non-Hodgkin lymphoma: the clinical perspective. Hepatology. 2012;55:634-41.
PubMed Abstract»Hermine O, Lefrère F, Bronowicki JP, et al. Regression of splenic lymphoma with villous lymphocytes after treatment of hepatitis C virus infection. N Engl J Med. 2002;347:89-94.
PubMed Abstract»Hosry J, Mahale P, Turturro F, et al. Antiviral therapy improves overall survival in hepatitis C virus-infected patients who develop diffuse large B-cell lymphoma. Int J Cancer. 2016;139:2519-28.
PubMed Abstract»Kawamura Y, Ikeda K, Arase Y, et al. Viral elimination reduces incidence of malignant lymphoma in patients with hepatitis C. Am J Med. 2007;120:1034-41.
PubMed Abstract»Masarone M, Persico M. Hepatitis C virus infection and non-hepatocellular malignancies in the DAA era: A systematic review and meta-analysis. Liver Int. 2019;39:1292-1306.
PubMed Abstract»Merli M, Carli G, Arcaini L, Visco C. Antiviral therapy of hepatitis C as curative treatment of indolent B-cell lymphoma. World J Gastroenterol. 2016;22:8447-8458.
PubMed Abstract»Michot JM, Canioni D, Driss H, et al. Antiviral therapy is associated with a better survival in patients with hepatitis C virus and B-cell non-Hodgkin lymphomas, ANRS HC-13 lympho-C study. Am J Hematol. 2015;90:197-203.
PubMed Abstract»Monti G, Pioltelli P, Saccardo F, et al. Incidence and characteristics of non-Hodgkin lymphomas in a multicenter case file of patients with hepatitis C virus-related symptomatic mixed cryoglobulinemias. Arch Intern Med. 2005;165:101-5.
PubMed Abstract»Peveling-Oberhag J, Arcaini L, Bankov K, Zeuzem S, Herrmann E. The anti-lymphoma activity of antiviral therapy in HCV-associated B-cell non-Hodgkin lymphomas: a meta-analysis. J Viral Hepat. 2016;23:536-44.
PubMed Abstract»Peveling-Oberhag J, Arcaini L, Hansmann ML, Zeuzem S. Hepatitis C-associated B-cell non-Hodgkin lymphomas. Epidemiology, molecular signature and clinical management. J Hepatol. 2013;59:169-77.
PubMed Abstract»Pozzato G, Mazzaro C, Gattei V. Hepatitis C Virus-Associated Non-Hodgkin Lymphomas: Biology, Epidemiology, and Treatment. Clin Liver Dis. 2017;21:499-515.
PubMed Abstract»Rossotti R, Travi G, Pazzi A, Baiguera C, Morra E, Puoti M. Rapid clearance of HCV-related splenic marginal zone lymphoma under an interferon-free, NS3/NS4A inhibitor-based treatment. A case report. J Hepatol. 2015;62:234-7.
PubMed Abstract»Sultanik P, Klotz C, Brault P, Pol S, Mallet V. Regression of an HCV-associated disseminated marginal zone lymphoma under IFN-free antiviral treatment. Blood. 2015;125:2446-7.
PubMed Abstract»Tasleem S, Sood GK. Hepatitis C Associated B-cell Non-Hodgkin Lymphoma: Clinical Features and the Role of Antiviral Therapy. J Clin Transl Hepatol. 2015;3:134-9.
PubMed Abstract»Torres HA, Mahale P. Most patients with HCV-associated lymphoma present with mild liver disease: a call to revise antiviral treatment prioritization. Liver Int. 2015;35:1661-4.
PubMed Abstract»Zaky AH, Bakry R, El-sayed MI, Elwanis MA, Nabih O. Impact of treatment-related toxicity on outcome of HCV-positive diffuse large B-cell lymphoma in rituximab era. Hematology. 2014;19:412-6.
PubMed Abstract»Zignego AL, Ramos-Casals M, Ferri C, et al. International therapeutic guidelines for patients with HCV-related extrahepatic disorders. A multidisciplinary expert statement. Autoimmun Rev. 2017;16:523-541.
PubMed Abstract»Cardiovascular Events
Adinolfi LE, Petta S, Fracanzani AL, et al. Impact of hepatitis C virus clearance by direct-acting antiviral treatment on the incidence of major cardiovascular events: A prospective multicentre study. Atherosclerosis. 2020;296:40-7.
PubMed Abstract»Adinolfi LE, Restivo L, Guerrera B, et al. Chronic HCV infection is a risk factor of ischemic stroke. Atherosclerosis. 2013;231:22-6.
PubMed Abstract»Butt AA, Xiaoqiang W, Budoff M, Leaf D, Kuller LH, Justice AC. Hepatitis C virus infection and the risk of coronary disease. Clin Infect Dis. 2009;49:225-32.
PubMed Abstract»Butt AA, Yan P, Shuaib A, Abou-Samra AB, Shaikh OS, Freiberg MS. Direct-Acting Antiviral Therapy for HCV Infection Is Associated With a Reduced Risk of Cardiovascular Disease Events. Gastroenterology. 2019;156:987-96.e8.
PubMed Abstract»Cacoub P, Saadoun D. Extrahepatic Manifestations of Chronic HCV Infection. N Engl J Med. 2021;384:1038-52.
PubMed Abstract»Cacoub P. Hepatitis C Virus Infection, a New Modifiable Cardiovascular Risk Factor. Gastroenterology. 2019;156:862-4.
PubMed Abstract»Jaiswal V, Ang SP, Hanif M, et al. Cardioprotective effect of antiviral therapy among hepatitis C infected patients: A meta-analysis. Int J Cardiol Heart Vasc. 2023;49:101270.
PubMed Abstract»Li J, Gordon SC, Rupp LB, et al. Sustained virological response to hepatitis C treatment decreases the incidence of complications associated with type 2 diabetes. Aliment Pharmacol Ther. 2019;49:599-608.
PubMed Abstract»Nahon P, Bourcier V, Layese R, et al. Eradication of Hepatitis C Virus Infection in Patients With Cirrhosis Reduces Risk of Liver and Non-Liver Complications. Gastroenterology. 2017;152:142-56.e2.
PubMed Abstract»Oliveira CP, Kappel CR, Siqueira ER, et al. Effects of hepatitis C virus on cardiovascular risk in infected patients: a comparative study. Int J Cardiol. 2013;164:221-6.
PubMed Abstract»Petta S, Maida M, Macaluso FS, et al. Hepatitis C Virus Infection Is Associated With Increased Cardiovascular Mortality: A Meta-Analysis of Observational Studies. Gastroenterology. 2016;150:145-55.
PubMed Abstract»Pothineni NV, Delongchamp R, Vallurupalli S, et al. Impact of hepatitis C seropositivity on the risk of coronary heart disease events. Am J Cardiol. 2014;114:1841-5.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with renal impairment.
AASLD-IDSA Hepatitis C Guidance»Cacoub P, Comarmond C, Desbois AC, Saadoun D. Rheumatologic Manifestations of Hepatitis C Virus Infection. Clin Liver Dis. 2017;21:455-64.
PubMed Abstract»Cacoub P, Vautier M, Desbois AC, Lafuma A, Saadoun D. Effectiveness and cost of hepatitis C virus cryoglobulinaemia vasculitis treatment: From interferon-based to direct-acting antivirals era. Liver Int. 2017;37:1805-13.
PubMed Abstract»Ferri C, Ramos-Casals M, Zignego AL, et al. International diagnostic guidelines for patients with HCV-related extrahepatic manifestations. A multidisciplinary expert statement. Autoimmun Rev. 2016;15:1145-1160.
PubMed Abstract»Hui JM, Sud A, Farrell GC, et al. Insulin resistance is associated with chronic hepatitis C virus infection and fibrosis progression. Gastroenterology. 2003;125:1695-704.
PubMed Abstract»Lens S, Rodriguez-Tajes S, Llovet LP, Maduell F, Londoño MC. Treating Hepatitis C in Patients with Renal Failure. Dig Dis. 2017;35:339-346.
PubMed Abstract»Nahon P, Bourcier V, Layese R, et al. Eradication of Hepatitis C Virus Infection in Patients With Cirrhosis Reduces Risk of Liver and Non-Liver Complications. Gastroenterology. 2017;152:142-56.e2.
PubMed Abstract»Obata F, Murakami T, Miyagi J, et al. A case of rapid amelioration of hepatitis C virus-associated cryoglobulinemic membranoproliferative glomerulonephritis treated by interferon-free directly acting antivirals for HCV in the absence of immunosuppressant. CEN Case Rep. 2017;6:55-60.
PubMed Abstract»Polo ML, Laufer N. Extrahepatic manifestations of HCV: the role of direct acting antivirals. Expert Rev Anti Infect Ther. 2017;15:737-746.
PubMed Abstract»Ramos-Casals M, Zignego AL, Ferri C, et al. Evidence-based recommendations on the management of extrahepatic manifestations of chronic hepatitis C virus infection. J Hepatol. 2017;66:1282-1299.
PubMed Abstract»Roth D, Nelson DR, Bruchfeld A, et al. Grazoprevir plus elbasvir in treatment-naive and treatment-experienced patients with hepatitis C virus genotype 1 infection and stage 4-5 chronic kidney disease (the C-SURFER study): a combination phase 3 study. Lancet. 2015;386:1537-45.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Sherman AC, Sherman KE. Extrahepatic manifestations of hepatitis C infection: navigating CHASM. Curr HIV/AIDS Rep. 2015;12:353-61.
PubMed Abstract»Sise ME, Bloom AK, Wisocky J, et al. Treatment of hepatitis C virus-associated mixed cryoglobulinemia with direct-acting antiviral agents. Hepatology. 2016;63:408-17.
PubMed Abstract»Tsui JI, Vittinghoff E, Shlipak MG, Bertenthal D, Inadomi J, Rodriguez RA, O'Hare AM. Association of hepatitis C seropositivity with increased risk for developing end-stage renal disease. Arch Intern Med. 2007;167:1271-6.
PubMed Abstract»Younossi Z, Park H, Henry L, Adeyemi A, Stepanova M. Extrahepatic Manifestations of Hepatitis C: A Meta-analysis of Prevalence, Quality of Life, and Economic Burden. Gastroenterology. 2016;150:1599-1608.
PubMed Abstract»Module 3. Management of Cirrhosis-Related Complications
Lesson 1. Diagnosis and Management of Ascites
Background
Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Planas R, Montoliu S, Ballesté B, et al. Natural history of patients hospitalized for management of cirrhotic ascites. Clin Gastroenterol Hepatol. 2006;4:1385-94.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Evaluation of Ascites
Asrani SK, Larson JJ, Yawm B, Therneau TM, Kim WR. Underestimation of liver-related mortality in the United States. Gastroenterology. 2013;145:375-82.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Cattau EL Jr, Benjamin SB, Knuff TE, Castell DO. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982;247:1164-6.
PubMed Abstract»De Gottardi A, Thévenot T, Spahr L, Morard I, Bresson-Hadni S, Torres F, Giostra E, Hadengue A. Risk of complications after abdominal paracentesis in cirrhotic patients: a prospective study. Clin Gastroenterol Hepatol. 2009;7:206-9.
PubMed Abstract»Ginés P, Quintero E, Arroyo V, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1987;7:122-8.
PubMed Abstract»Gunawan B, Runyon B. The efficacy and safety of epsilon-aminocaproic acid treatment in patients with cirrhosis and hyperfibrinolysis. Aliment Pharmacol Ther. 2006;23:115-20.
PubMed Abstract»Northup PG, Garcia-Pagan JC, Garcia-Tsao G, et al. Vascular Liver Disorders, Portal Vein Thrombosis, and Procedural Bleeding in Patients With Liver Disease: 2020 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;73:366-413.
PubMed Abstract»Pache I, Bilodeau M. Severe haemorrhage following abdominal paracentesis or ascites in patients with liver failure. Aliment Pharmacol Ther. 2005;21:525-9.
PubMed Abstract»Planas R, Montoliu S, Ballesté B, et al. Natural history of patients hospitalized for management of cirrhotic ascites. Clin Gastroenterol Hepatol. 2006;4:1385-94.
PubMed Abstract»Runyon BA, Hoefs JC, Canawati HN. Polymicrobial bacterascites. A unique entity in the spectrum of infected ascitic fluid. Arch Intern Med. 1986;146:2173-5.
PubMed Abstract»Runyon BA, Montano AA, Akriviadis EA, Antillon MR, Irving MA, McHutchison JG. The serum-ascites albumin gradient is superior to the exudate-transudate concept in the differential diagnosis of ascites. Ann Intern Med. 1992;117:215-20.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Runyon BA. Paracentesis of ascitic fluid: a safe procedure. Arch Intern Med. 1986;146:2259-61.
PubMed Abstract»Sakai H, Sheer TA, Mendler MH, Runyon BA. Choosing the location for non-image guided abdominal paracentesis. Liver Int. 2005;25:984-6.
PubMed Abstract»Analysis of Ascitic Fluid
Akriviadis EA, Runyon BA. Utility of an algorithm in differentiating spontaneous from secondary bacterial peritonitis. Gastroenterology. 1990;98:127-33.
PubMed Abstract»Hillebrand DJ, Runyon BA, Yasmineh WG, Rynders GP. Ascitic fluid adenosine deaminase insensitivity in detecting tuberculous peritonitis in the United States. Hepatology. 1996;24:1408-12.
PubMed Abstract»Hoefs JC, Canawati HN, Sapico FL, Hopkins RR, Weiner J, Montgomerie JZ. Spontaneous bacterial peritonitis. Hepatology. 1982;2:399-407.
PubMed Abstract»Jeffries MA, Stern MA, Gunaratnam NT, Fontana RJ. Unsuspected infection is infrequent in asymptomatic outpatients with refractory ascites undergoing therapeutic paracentesis. Am J Gastroenterol. 1999;94:2972-6.
PubMed Abstract»Runyon BA, Antillon MR, Akriviadis EA, McHutchinson JG. Bedside inoculation of blood culture bottles is superior to delayed inoculation in the detection of spontaneous bacterial peritonitis. J Clin Microbiol. 1990;28:2811-2.
PubMed Abstract»Runyon BA, Canawati HN, Akriviadis EA. Optimization of ascitic fluid culture technique. Gastroenterology. 1988;95:1351-5.
PubMed Abstract»Runyon BA, Hoefs JC, Morgan TR. Ascitic fluid analysis in malignancy-related ascites. Hepatology. 1988;8:1104-9.
PubMed Abstract»Runyon BA, Hoefs JC. Ascitic fluid analysis in the differentiation of spontaneous bacterial peritonitis from gastrointestinal tract perforation into ascitic fluid. Hepatology. 1984;4:447-50.
PubMed Abstract»Runyon BA, Montano AA, Akriviadis EA, Antillon MR, Irving MA, McHutchison JG. The serum-ascites albumin gradient is superior to the exudate-transudate concept in the differential diagnosis of ascites. Ann Intern Med. 1992;117:215-20.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Runyon BA. Malignancy-related ascites and ascitic fluid “humoral tests of malignancy.” J Clin Gastroenterol. 1994;18:94-8.
PubMed Abstract»Runyon BA. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009;49:2087-107.
PubMed Abstract»Such J, Runyon BA. Spontaneous bacterial peritonitis. Clin Infect Dis. 1998;27:669-74.
PubMed Abstract»Wu SS, Lin OS, Chen Y-Y, Hwang KL, Soon MS, Keeffe EB. Ascitic fluid carcinoembryonic antigen and alkaline phosphatase levels for the differentiation of primary from secondary bacterial peritonitis with intestinal perforation. J Hepatol. 2001;34:215-21.
PubMed Abstract»Basic Management of Ascites
Angeli P, Dalla Pria M, De Bei E, Albino G, Caregaro L, Merkel C, Ceolotto G, Gatta A. Randomized clinical study of the efficacy of amiloride and potassium canrenoate in nonazotemic cirrhotic patients with ascites. Hepatology. 1994;19:72-9.
PubMed Abstract»Angeli P, Fasolato S, Mazza E, et al. Combined versus sequential diuretic treatment of ascites in non-azotaemic patients with cirrhosis: results of an open randomised clinical trial. Gut. 2010;59:98-104.
PubMed Abstract»Bernardi M, Caraceni P, Navickis RJ, Wilkes MM. Albumin infusion in patients undergoing large-volume paracentesis: a meta-analysis of randomized trials. Hepatology. 2012;55:1172-81.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Cárdenas A, Ginès P, Marotta P, et al. Tolvaptan, an oral vasopressin antagonist, in the treatment of hyponatremia in cirrhosis. J Hepatol. 2012;56:571-8.
PubMed Abstract»Dimitriadis G, Papadopoulos V, Mimidis K. Eplerenone reverses spironolactone-induced painful gynaecomastia in cirrhotics. Hepatol Int. 2011;5:738-9.
PubMed Abstract»Eisengmenger WJ, Blondheim SH, Bongiovanni AM, Kunkel HG. Electrolyte studies on patients with cirrhosis of the liver. J Clin Invest. 1950;29:1491-9.
PubMed Abstract»Ginès P, Arroyo V, Quintero E, et al. Comparison of paracentesis and diuretics in the treatment of cirrhotics with tense ascites. Results of a randomized study. Gastroenterology. 1987;93:234-41.
PubMed Abstract»Ohki T, Sato K, Yamada T, et al. Efficacy of tolvaptan in patients with refractory ascites in a clinical setting. World J Hepatol. 2015;7:1685-93.
PubMed Abstract»Pérez-Ayuso RM, Arroyo V, Planas R, et al. Randomized comparative study of efficacy of furosemide versus spironolactone in nonazotemic cirrhosis with ascites. Relationship between the diuretic response and the activity of the renin-aldosterone system. Gastroenterology. 1983;84:961-8.
PubMed Abstract»Peltekian KM, Wong F, Liu PP, Logan AG, Sherman M, Blendis LM. Cardiovascular, renal and neurohumoral responses to single large-volume paracentesis patients with cirrhosis and diuretic-resistant ascites. Am J Gastroenterol. 1997;92:394-9.
PubMed Abstract»Pockros PJ, Reynolds TB. Rapid diuresis in patients with ascites from chronic liver disease: the importance of peripheral edema. Gastroenterology. 1986;90:1827-33.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Santos J, Planas R, Pardo A, et al. Spironolactone alone or in combination with furosemide in the treatment of moderate ascites in nonazotemic cirrhosis. A randomized comparative study of efficacy and safety. J Hepatol. 2003;39:187-92.
PubMed Abstract»Schrier RW, Gross P, Gheorghiade M, et al. Tolvaptan, a selective oral vasopressin V2-receptor antagonist, for hyponatremia. N Engl J Med. 2006;355:2099-112.
PubMed Abstract»Sersté T, Melot C, Francoz C, et al. Deleterious effects of beta-blockers on survival in patients with cirrhosis and refractory ascites. Hepatology. 2010;52:1017-22.
PubMed Abstract»Titó L, Ginès P, Arroyo V, et al. Total paracentesis associated with intravenous albumin management of patients with cirrhosis and ascites. Gastroenterology. 1990;98:146-51.
PubMed Abstract»Veldt BJ, Lainé F, Guillygomarc’h A, et al. Indication of liver transplantation in severe alcoholic liver cirrhosis: quantitative evaluation and optimal timing. J Hepatol. 2002;36:93-8.
PubMed Abstract»Wong F, Blei AT, Blendis LM, Thuluvath PJ. A vasopressin receptor antagonist (VPA-985) improves serum sodium concentration in patients with hyponatremia: a multicenter, randomized, placebo-controlled trial. Hepatology. 2003;37:182-91.
PubMed Abstract»Wong F, Watson H, Gerbes A, et al. Satavaptan for the management of ascites in cirrhosis: efficacy and safety across the spectrum of ascites severity. Gut. 2012;61:108-16.
PubMed Abstract»Zhang X, Wang SZ, Zheng JF, et al. Clinical efficacy of tolvaptan for treatment of refractory ascites in liver cirrhosis patients. World J Gastroenterol. 2014;20:11400-5.
PubMed Abstract»Management of Refractory Ascites
Arroyo V, Ginès P, Gerbes AL, et al. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. International Ascites Club. Hepatology. 1996;23:164-76.
PubMed Abstract»Baltz JG, Argo CK, Al-Osaimi AM, Northup PG. Mortality after percutaneous endoscopic gastrostomy in patients with cirrhosis: a case series. Gastrointest Endscop. 2010;72:1072-5.
PubMed Abstract»Bernardi M, Caraceni P, Navickis RJ, Wilkes MM. Albumin infusion in patients undergoing large-volume paracentesis: a meta-analysis of randomized trials. Hepatology. 2012;55:1172-81.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Boyer TD, Haskal ZJ, American Association for the Study of Liver Diseases. The Role of Transjugular Intrahepatic Portosystemic Shunt (TIPS) in the Management of Portal Hypertension: update 2009. Hepatology. 2010;51:306.
PubMed Abstract»Ginès P, Arroyo V, Quintero E, et al. Comparison of paracentesis and diuretics in the treatment of cirrhotics with tense ascites. Results of a randomized study. Gastroenterology. 1987;93:234-41.
PubMed Abstract»Ginès P, Arroyo V, Vargas V, et al. Paracentesis with intravenous infusion of albumin as compared with peritoneovenous shunting in cirrhosis with refractory ascites. N Engl J Med. 1991;325:829-35.
PubMed Abstract»Ginès P, Titó L, Arroyo V, et al. Randomized comparative study of therapeutic paracentesis with and without intravenous albumin in cirrhosis. Gastroenterology. 1988;94;1493-502.
PubMed Abstract»Ginès P, Uriz J, Calahorra B, et al. Transjugular intrahepatic portosystemic shunting versus paracentesis plus albumin for refractory ascites in cirrhosis. Gastroenterology. 2002;123:1839-47.
PubMed Abstract»Guardiola J, Xiol X, Escribá JM, et al. Prognosis assessment of cirrhotic patients with refractory ascites treated with a peritoneovenous shunt. Am J Gastroenterol. 1995;90:2097-102.
PubMed Abstract»Heuman DM, Abou-Assi SG, Habib A, et al. Persistent ascites and low serum sodium to identify patients with cirrhosis and low MELD scores who are high risk for early death. Hepatology. 2004;40:802-10.
PubMed Abstract»Rössle M, Ochs A, Gülberg V, et al. A comparison of paracentesis and transjugular intrahepatic portosystemic shunting in patients with ascites. N Engl J Med. 2000;342:1701-7.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Salerno F, Cammà C, Enea M, Rössle M, Wong F. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology. 2007;133:825-34.
PubMed Abstract»Salerno F, Merli M, Riggio O, et al. Randomized controlled study of TIPS versus paracentesis plus albumin in cirrhosis with severe ascites. Hepatology. 2004;40:629-35.
PubMed Abstract»Sanyal AJ, Freedman AM, Shiffman ML, Purdum PP 3rd, Luketic VA, Cheatham AK. Portosystemic encephalopathy after transjugular intrahepatic portosystemic shunt: results of a prospective controlled study. Hepatology. 1994;20:46-55.
PubMed Abstract»Sanyal AJ, Genning C, Reddy KR, et al. The North American Study for the Treatment of Refractory Ascites. Gastroenterology. 2003;124:634-41.
PubMed Abstract»Sersté T, Melot C, Francoz C, et al. Deleterious effects of beta-blockers on survival in patients with cirrhosis and refractory ascites. Hepatology. 2010;52:1017-22.
PubMed Abstract»Singh V, Dheerendra PC, Singh B, et al. Midodrine versus albumin in the prevention of paracentesis-induced circulatory dysfunction in cirrhotics: a randomized pilot study. Am J Gastroenterol. 2008;103:1399-405.
PubMed Abstract»Singh V, Dhungana SP, Singh B, et al. Midodrine in patients with cirrhosis and refractory or recurrent ascites: a randomized pilot study. J Hepatol. 2012;56:348-54.
PubMed Abstract»Somberg KA, Lake JR, Tomlanovich SJ, LaBerge JM, Feldstein V, Bass NM. Transjugular intrahepatic portosystemic shunts for refractory ascites: assessment of clinical and hormonal response and renal function. Hepatology. 1995;21:709-16.
PubMed Abstract»Stanley MM, Ochi S, Lee KK, et al. Peritoneovenous shunting as compared with medical treatment in patients with alcoholic cirrhosis and massive ascites. Veterans Administration Cooperative Study on Treatment of Alcoholic Cirrhosis with Ascites. N Engl J Med. 1989;321:1632-8.
PubMed Abstract»Titó L, Ginès P, Arroyo V, et al. Total paracentesis associated with intravenous albumin management of patients with cirrhosis and ascites. Gastroenterology. 1990;98:146-51.
PubMed Abstract»Complications Associated with Ascites
Angeli P, Dalla Pria M, De Bei E, Albino G, Caregaro L, Merkel C, Ceolotto G, Gatta A. Randomized clinical study of the efficacy of amiloride and potassium canrenoate in nonazotemic cirrhotic patients with ascites. Hepatology. 1994;19:72-9.
PubMed Abstract»Angeli P, Wong F, Watson H, Ginès P; CAPPS Investigators. Hyponatremia in cirrhosis: Results of a patient population survey. Hepatology. 2006;44:1535-42.
PubMed Abstract»Bajaj JS, Tandon P, OʼLeary JG, et al. The Impact of Albumin Use on Resolution of Hyponatremia in Hospitalized Patients With Cirrhosis. Am J Gastroenterol. 2018;113:1339.
PubMed Abstract»Belghiti J, Durand F. Abdominal wall hernias in the setting of cirrhosis. Semin Liver Dis. 1997;17:219-26.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Duvoux C, Zanditenas D, Hézode C, et al. Effects of noradrenalin and albumin in patients with type I hepatorenal syndrome: a pilot study. Hepatology. 2002;36:374-80.
PubMed Abstract»Egerod Israelsen M, Gluud LL, Krag A. Acute kidney injury and hepatorenal syndrome in cirrhosis. J Gastroenterol Hepatol. 2015;30:236-43.
PubMed Abstract»Esrailian E, Pantangco ER, Kyulo NL, Hu KQ, Runyon BA. Octreotide/Midodrine therapy significantly improves renal function and 30-day survival in patients with type 1 hepatorenal syndrome. Dig Dis Sci. 2007;52:742-8.
PubMed Abstract»Felisart J, Rimola A, Arroyo V, Perez-Ayuso RM, Quintero E, Gines P, Rodes J. Cefotaxime is more effective than is ampicillin-tobramycin in cirrhotics with severe infections. Hepatology 1985;5:457-62.
PubMed Abstract»Gankam Kengne F, Decaux G. Hyponatremia and the Brain. Kidney Int Rep. 2018;3:24-35.
PubMed Abstract»Ginès P, Guevera M, Arroyo V, Rodés J. Hepatorenal syndrome. Lancet. 2003;362:1819-27.
PubMed Abstract»Ginès P, Rimola A, Plana R, et al. Norfloxacin prevents spontaneous bacterial peritonitis recurrence in cirrhosis: results of a double-blind, placebo-controlled trial. Hepatology. 1990;12:716-24.
PubMed Abstract»Ginès P, Solà E, Angeli P, Wong F, Nadim MK, Kamath PS. Author Correction: Hepatorenal syndrome. Nat Rev Dis Primers. 2018;4:33.
PubMed Abstract»Gluud LL, Christensen K, Christensen E, Krag A. Systematic review of randomized trials on vasoconstrictor drugs for hepatorenal syndrome. Hepatology. 2010;51:576-84.
PubMed Abstract»Greenberg A, Verbalis JG. Vasopressin receptor antagonists. Kidney Int. 2006;69:2124-30.
PubMed Abstract»Heuman DM, Abou-Assi SG, Habib A, et al. Persistent ascites and low serum sodium to identify patients with cirrhosis and low MELD scores who are high risk for early death. Hepatology. 2004;40:802-10.
PubMed Abstract»Hoefs JC, Canawati HN, Sapico FL, Hopkins RR, Weiner J, Montgomerie JZ. Spontaneous bacterial peritonitis. Hepatology. 1982;2:399-407.
PubMed Abstract»Martín-Llahí M, Pépin MN, Guevara M, et al. Terlipressin and albumin vs albumin in patients with cirrhosis and hepatorenal syndrome: a randomized study. Gastroenterology. 2008;134:1352-9.
PubMed Abstract»Miller PD, Linas SL, Schrier RW. Plasma demeclocycline levels and nephrotoxicity. Correlation in hyponatremic cirrhotic patients. JAMA. 1980;243;2513-5.
PubMed Abstract»Montoliu S, Ballesté B, Planas R, et al. Incidence and prognosis of different types of functional renal failure in cirrhotic patients with ascites. Clin Gastroenterol Hepatol. 2010;8:616-22.
PubMed Abstract»Orman ES, Lok AS. Outcomes of patients with chest tube insertion for hepatic hydrothorax. Hepatol Int. 2009;3:582-6.
PubMed Abstract»Planas R, Montoliu S, Ballesté B, et al. Natural history of patients hospitalized for management of cirrhotic ascites. Clin Gastroenterol Hepatol. 2006;4:1385-94.
PubMed Abstract»Rubinstein D, McInnes IE, Dudley FJ. Hepatic hydrothorax in the absence of clinical ascites: diagnosis and management. Gastroenterology. 1985;88:188-91.
PubMed Abstract»Runyon BA, Greenblatt M, Ming RH. Hepatic hydrothorax is a relative contraindication to chest tube insertion. Am J Gastroenterol. 1986;81:566-7.
PubMed Abstract»Runyon BA, Juler GL. Natural history of repaired umbilical hernias in patients with and without cirrhosis. Am J Gastroenterol. 1985;80:38-9.
PubMed Abstract»Runyon BA, McHutchinson JG, Antillon MR, Akriviadis EA, Montano A. Short-course versus long-course antibiotic treatment of spontaneous bacterial peritonitis: a randomized controlled trial of 100 patients. Gastroenterology. 1991;100:1737-42.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Runyon BA. Paracentesis of ascitic fluid: a safe procedure. Arch Intern Med. 1986;146:2259-61.
PubMed Abstract»Salerno F, Cammà C, Enea M, Rössle M, Wong F. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology. 2007;133:825-34.
PubMed Abstract»Salerno F, Gerbes A, Ginès P, Wong F, Arroyo V. Diagnosis, prevention and treatment of hepatorenal syndrome in cirrhosis. Gut. 2007;56:1310-8.
PubMed Abstract»Sanyal AJ, Boyer T, Garcia-Tsao G, et al. A randomized, prospective, double-blind, placebo-controlled trial of terlipressin for type 1 hepatorenal syndrome. Gastroenterology. 2008;134:1360-8.
PubMed Abstract»Sigal SH, Stanca CM, Fernandez J, Arroyo V, Navasa M. Restricted use of albumin for spontaneous bacterial peritonitis. Gut. 2007;56:597-9.
Gut»Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999;341:403-9.
PubMed Abstract»Telem DA, Schiano T, Divino CM. Complicated hernia presentation in patients with advanced cirrhosis and refractory ascites: management and outcome. Surgery. 2010;148:538-43.
PubMed Abstract»Triantos CK, Kehagias I, Nikolopoulou V, Burrhoughs AK. Surgical repair of umbilical hernias in cirrhosis with ascites. Am J Med Sci. 2011;341:222-6.
PubMed Abstract»Wong F. Recent advances in our understanding of hepatorenal syndrome. Nat Rev Gastroenterol Hepatol. 2012;9:382-91.
PubMed Abstract»Xiol X, Castellote J, Cortes-Beut R, Delgado M, Guardiola J, Sesé E. Usefulness and complications of thoracentesis in cirrhotic patients. Am J Med. 2001;111:67-9.
Elsevier»Xiol X, Castellví JM, Guardiola J, Sesé E, Castellote J, Perelló A, Cervantes X, Iborra MJ. Spontaneous bacterial empyema in cirrhotic patients: a prospective study. Hepatology. 1996;23: 719-23.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy has failed: DAA-experienced (including NS5A inhibitors except glecaprevir-pibrentasvir failures), genotype 5 or 6 patients, with or without compensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy has failed: peginterferon plus ribavirin-experienced, genotype 5 or 6 patients with or without compensated cirrhosis
AASLD-IDSA Hepatitis C Guidance»Abergel A, Asselah T, Metivier S, et al. Ledipasvir-sofosbuvir in patients with hepatitis C virus genotype 5 infection: an open-label, multicentre, single-arm, phase 2 study. Lancet Infect Dis. 2016;16:459-64.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Bourlière M, Gordon SC, Flamm SL, et al. Sofosbuvir, Velpatasvir, and Voxilaprevir for Previously Treated HCV Infection. N Engl J Med. 2017;376:2134-46.
PubMed Abstract»Cattau EL Jr, Benjamin SB, Knuff TE, Castell DO. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982;247:1164-6.
PubMed Abstract»Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599-607.
PubMed Abstract»Llach J, Ginès P, Arroyo V, et al. Prognostic value of arterial pressure, endogenous vasoactive systems, and renal function in cirrhotic patients admitted to the hospital for the treatment of ascites. Gastroenterology. 1988;94:482-7.
PubMed Abstract»Mauss S, Berger F, Vogel M, et al. Treatment results of chronic hepatitis C genotype 5 and 6 infections in Germany. Z Gastroenterol. 2012;50:441-4.
PubMed Abstract»McOmish F, Yap PL, Dow BC, et al. Geographical distribution of hepatitis C virus genotypes in blood donors: an international collaborative survey. J Clin Microbiol. 1994;32:884-92.
PubMed Abstract»Salerno F, Gerbes A, Ginès P, Wong F, Arroyo V. Diagnosis, prevention and treatment of hepatorenal syndrome in cirrhosis. Gut. 2007;56:1310-8.
PubMed Abstract»Wantuck JM, Ahmed A, Nguyen MH. Review article: the epidemiology and therapy of chronic hepatitis C genotypes 4, 5 and 6. Aliment Pharmacol Ther. 2014;39:137-47.
PubMed Abstract»Lesson 2. Recognition and Management of Spontaneous Bacterial Peritonitis
Background
Alaniz C, Regal RE. Spontaneous bacterial peritonitis: a review of treatment options. P T. 2009;34:204-10.
PubMed Abstract»Andreu M, Sola R, Sitges-Serra A, et al. Risk factors for spontaneous bacterial peritonitis in cirrhotic patients with ascites. Gastroenterology. 1993;104:1133-8.
PubMed Abstract»Dever JB, Sheikh MY. Review article: spontaneous bacterial peritonitis--bacteriology, diagnosis, treatment, risk factors and prevention. Aliment Pharmacol Ther. 2015;41:1116-31.
PubMed Abstract»Friedrich K, Nüssle S, Rehlen T, Stremmel W, Mischnik A, Eisenbach C. Microbiology and resistance in first episodes of spontaneous bacterial peritonitis: implications for management and prognosis. J Gastroenterol Hepatol. 2016;31:1191-5.
PubMed Abstract»Goel A, Biewald M, Huprikar S, Schiano T, Im GY. A Real-World Evaluation of Repeat Paracentesis-guided Management of Spontaneous Bacterial Peritonitis. J Clin Gastroenterol. 2017;51:278-284.
PubMed Abstract»Guarner C, Soriano G. Bacterial translocation and its consequences in patients with cirrhosis. Eur J Gastroenterol Hepatol. 2005;17:27-31.
PubMed Abstract»Hurwich DB, Lindor KD, Hay JE, Gross JB Jr, Kaese D, Rakela J. Prevalence of peritonitis and the ascitic fluid protein concentration among chronic liver disease patients. Am J Gastroenterol. 1993;88:1254-7.
PubMed Abstract»Khan MA, Kamal S, Khan S, Lee WM, Howden CW. Systematic review and meta-analysis of the possible association between pharmacological gastric acid suppression and spontaneous bacterial peritonitis. Eur J Gastroenterol Hepatol. 2015;27:1327-36.
PubMed Abstract»Llach J, Rimola A, Navasa M, et al. Incidence and predictive factors of first episode of spontaneous bacterial peritonitis in cirrhosis with ascites: relevance of ascitic fluid protein concentration. Hepatology. 1992;16:724-7.
PubMed Abstract»Runyon BA, Squier S, Borzio M. Translocation of gut bacteria in rats with cirrhosis to mesenteric lymph nodes partially explains the pathogenesis of spontaneous bacterial peritonitis. J Hepatol. 1994;21:792-6.
PubMed Abstract»Runyon BA. Low-protein-concentration ascitic fluid is predisposed to spontaneous bacterial peritonitis. Gastroenterology. 1986;91:1343-6.
PubMed Abstract»Scarpellini E, Valenza V, Gabrielli M, et al. Intestinal permeability in cirrhotic patients with and without spontaneous bacterial peritonitis: is the ring closed? Am J Gastroenterol. 2010;105:323-7.
PubMed Abstract»Titó L, Rimola A, Ginès P, Llach J, Arroyo V, Rodés J. Recurrence of spontaneous bacterial peritonitis in cirrhosis: frequency and predictive factors. Hepatology. 1988;8:27-31.
PubMed Abstract»Diagnosis of Spontaneous Bacterial Peritonitis
Akriviadis EA, Runyon BA. Utility of an algorithm in differentiating spontaneous from secondary bacterial peritonitis. Gastroenterology. 1990;98:127-33.
PubMed Abstract»Alaniz C, Regal RE. Spontaneous bacterial peritonitis: a review of treatment options. P T. 2009;34:204-10.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Borzio M, Salerno F, Piantoni L, et al. Bacterial infection in patients with advanced cirrhosis: a multicentre prospective study. Dig Liver Dis. 2001;33:41-8.
PubMed Abstract»Dever JB, Sheikh MY. Review article: spontaneous bacterial peritonitis--bacteriology, diagnosis, treatment, risk factors and prevention. Aliment Pharmacol Ther. 2015;41:1116-31.
PubMed Abstract»Evans LT, Kim WR, Poterucha JJ, Kamath PS. Spontaneous bacterial peritonitis in asymptomatic outpatients with cirrhotic ascites. Hepatology. 2003;37:897-901.
PubMed Abstract»Garcia-Tsao G. Current management of the complications of cirrhosis and portal hypertension: variceal hemorrhage, ascites, and spontaneous bacterial peritonitis. Gastroenterology. 2001;120:726-48.
PubMed Abstract»Garrison RN, Cryer HM, Howard DA, Polk HC Jr. Clarification of risk factors for abdominal operations in patients with hepatic cirrhosis. Ann Surg. 1984;199:648-55.
PubMed Abstract»Grabau CM, Crago SF, Hoff LK, Simon JA, Melton CA, Ott BJ, Kamath PS. Performance standards for therapeutic abdominal paracentesis. Hepatology. 2004;40:484-8.
PubMed Abstract»Lu MLR, Agarwal A, Sloan J, Kosmin A. Infected ascites: Distinguishing secondary peritonitis from spontaneous bacterial peritonitis in a cirrhotic patient with classic symptoms. IDCases. 2017;8:29-31.
PubMed Abstract»McVay PA, Toy PT. Lack of increased bleeding after paracentesis and thoracentesis in patients with mild coagulation abnormalities. Transfusion. 1991;31:164-71.
PubMed Abstract»Northup PG, Garcia-Pagan JC, Garcia-Tsao G, et al. Vascular Liver Disorders, Portal Vein Thrombosis, and Procedural Bleeding in Patients With Liver Disease: 2020 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;73:366-413.
PubMed Abstract»Rimola A, Garcia-Tsao G, Navasa M, Piddock LJ, Planas R, Bernard B, Inadomi JM. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus statement. International Ascites Club. J Hepatol. 2000;32:142-53.
PubMed Abstract»Runyon BA, Antillon MR, Akriviadis EA, McHutchinson JG. Bedside inoculation of blood culture bottles is superior to delayed inoculation in the detection of spontaneous bacterial peritonitis. J Clin Microbiol. 1990;28:2811-2.
PubMed Abstract»Runyon BA, Antillon MR. Ascitic fluid pH and lactate: insensitive and nonspecific tests in detecting ascitic fluid infection. Hepatology. 1991;13:929-35.
PubMed Abstract»Runyon BA, Hoefs JC. Culture-negative neutrocytic ascites: a variant of spontaneous bacterial peritonitis. Hepatology. 1984;4;1209-11.
PubMed Abstract»Runyon BA. Low-protein-concentration ascitic fluid is predisposed to spontaneous bacterial peritonitis. Gastroenterology. 1986;91:1343-6.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Soriano G, Castellote J, Alvarez C, et al. Secondary bacterial peritonitis in cirrhosis: a retrospective study of clinical and analytical characteristics, diagnosis and management. J Hepatol. 2010;52:39-44.
PubMed Abstract»Tandon P, Garcia-Tsao G. Bacterial infections, sepsis, and multiorgan failure in cirrhosis. Semin Liver Dis. 2008;28:26-42.
PubMed Abstract»Wu SS, Lin OS, Chen Y-Y, Hwang KL, Soon MS, Keeffe EB. Ascitic fluid carcinoembryonic antigen and alkaline phosphatase levels for the differentiation of primary from secondary bacterial peritonitis with intestinal perforation. J Hepatol. 2001;34:215-21.
PubMed Abstract»Treatment of Spontaneous Bacterial Peritonitis
Akriviadis EA, Runyon BA. Utility of an algorithm in differentiating spontaneous from secondary bacterial peritonitis. Gastroenterology. 1990;98:127-33.
PubMed Abstract»Baskol M, Gursoy S, Baskol G, Ozbakir O, Guven K, Yucesoy M. Five days of ceftriaxone to treat culture negative neutrocytic ascites in cirrhotic patients. J Clin Gastroenterol. 2003;37:403-5.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Dever JB, Sheikh MY. Review article: spontaneous bacterial peritonitis--bacteriology, diagnosis, treatment, risk factors and prevention. Aliment Pharmacol Ther. 2015;41:1116-31.
PubMed Abstract»European Association for the Study of the Liver, Ginès P, Angeli P, et al. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397-417.
PubMed Abstract»Felisart J, Rimola A, Arroyo V, Perez-Ayuso RM, Quintero E, Gines P, Rodes J. Cefotaxime is more effective than is ampicillin-tobramycin in cirrhotics with severe infections. Hepatology 1985;5:457-62.
PubMed Abstract»Fernández J, Navasa M, Gómez J, Colmenero J, Vila J, Arroyo V, Rodés J. Bacterial infections in cirrhosis: epidemiological changes with invasive procedures and norfloxacin prophlaxis. Hepatology. 2002;35:140-8.
PubMed Abstract»França A, Giordano HM, Sevá-Pereira T, Soares EC. Five days of ceftriaxone to treat spontaneous bacterial peritonitis in cirrhotic patients. J Gastroenterol. 2002;37:119-22.
PubMed Abstract»França AV, De Souza JB, Silva CM, Soares EC. Long-term prognosis of cirrhosis after spontaneous bacterial peritonitis treated with ceftriaxone. J Clin Gastroenterol. 2001;33:295-8.
PubMed Abstract»Mesquita MA, Balbino EP, Albuquerque RS, et al. Ceftriaxone in the treatment of spontaneous bacterial peritonitis: ascitic fluid polymorphonuclear count response and short-term prognosis. Hepatogastroenterology. 1997;44:1276-80.
PubMed Abstract»Navasa M, Follo A, Llovet JM, et al. Randomized, comparative study of oral ofloxacin versus intravenous cefotaxime in spontaneous bacterial peritonitis. Gastroenterology. 1996;111;1011-7.
PubMed Abstract»Rimola A, Garcia-Tsao G, Navasa M, Piddock LJ, Planas R, Bernard B, Inadomi JM. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus statement. International Ascites Club. J Hepatol. 2000;32:142-53.
PubMed Abstract»Rimola A, Salmerón, Clemente G, et al. Two different dosages of cefotaxime in the treatment of spontaneous bacterial peritonitis in cirrhosis: results of a prospective, randomized, multicenter study. Hepatology 1995; 21:674-9.
PubMed Abstract»Runyon BA, Akriviadis EA, Sattler FR, Cohen J. Ascitic fluid and serum cefotaxime and desacetyl cefotaxime levels in patients treated for bacterial peritonitis. Dig Dis Sci. 1991;36:1782-6.
PubMed Abstract»Runyon BA, Antillon MR. Ascitic fluid pH and lactate: insensitive and nonspecific tests in detecting ascitic fluid infection. Hepatology. 1991;13:929-35.
PubMed Abstract»Runyon BA, Hoefs JC. Culture-negative neutrocytic ascites: a variant of spontaneous bacterial peritonitis. Hepatology. 1984;4;1209-11.
PubMed Abstract»Runyon BA, McHutchinson JG, Antillon MR, Akriviadis EA, Montano A. Short-course versus long-course antibiotic treatment of spontaneous bacterial peritonitis: a randomized controlled trial of 100 patients. Gastroenterology. 1991;100:1737-42.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Sigal SH, Stanca CM, Fernandez J, Arroyo V, Navasa M. Restricted use of albumin for spontaneous bacterial peritonitis. Gut. 2007;56:597-9.
Gut»Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999;341:403-9.
PubMed Abstract»Terg R, Cobas S, Fassio E, et al. Oral ciprofloxacin after a short course of intravenous ciprofloxacin in the treatment of spontaneous bacterial peritonitis: results of a multicenter, randomized study. J Hepatol. 2000;33:564-9.
PubMed Abstract»Indications for Spontaneous Bacterial Peritonitis Prophylaxis
Bernard B, Grange JD, Khac EN, Amiot X, Opolon P, Poynard T. Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with gastrointestinal bleeding: a meta-analysis. Hepatology. 1999;29:1655-61.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Carbonnell N, Pauwels A, Serfaty L, Fourdan O, Levy VG, Poupon R. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology. 2004;40: 652-9.
PubMed Abstract»Deschenes M, Villenueve JP. Risk factors for the development of bacterial infections in hospitalized patients with cirrhosis. Am J Gastroenterol. 1999;94:2193-7.
PubMed Abstract»Dever JB, Sheikh MY. Review article: spontaneous bacterial peritonitis--bacteriology, diagnosis, treatment, risk factors and prevention. Aliment Pharmacol Ther. 2015;41:1116-31.
PubMed Abstract»Fernández J, Navasa M, Planas R, et al. Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology. 2007;133:818-24.
PubMed Abstract»Garcia-Tsao G. Current management of the complications of cirrhosis and portal hypertension: variceal hemorrhage, ascites, and spontaneous bacterial peritonitis. Gastroenterology. 2001;120:726-48.
PubMed Abstract»Guarner C, Soriano G. Bacterial translocation and its consequences in patients with cirrhosis. Eur J Gastroenterol Hepatol. 2005;17:27-31.
PubMed Abstract»Rimola A, Garcia-Tsao G, Navasa M, Piddock LJ, Planas R, Bernard B, Inadomi JM. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus statement. International Ascites Club. J Hepatol. 2000;32:142-53.
PubMed Abstract»Runyon BA, Squier S, Borzio M. Translocation of gut bacteria in rats with cirrhosis to mesenteric lymph nodes partially explains the pathogenesis of spontaneous bacterial peritonitis. J Hepatol. 1994;21:792-6.
PubMed Abstract»Runyon BA. Low-protein-concentration ascitic fluid is predisposed to spontaneous bacterial peritonitis. Gastroenterology. 1986;91:1343-6.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Scarpellini E, Valenza V, Gabrielli M, et al. Intestinal permeability in cirrhotic patients with and without spontaneous bacterial peritonitis: is the ring closed? Am J Gastroenterol. 2010;105:323-7.
PubMed Abstract»Regimens for Spontaneous Bacterial Peritonitis Prophylaxis
Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Campillo B, Dupeyron C, Richardet JP, Mangeney N, Leluan G. Epidemiology of severe hospital acquired infections in patients with liver cirrhosis: effect of long-term administration of norfloxacin. Clin Infect Dis. 1998;26:1066-70.
PubMed Abstract»European Association for the Study of the Liver, Ginès P, Angeli P, et al. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397-417.
PubMed Abstract»Fernández J, Navasa M, Gómez J, Colmenero J, Vila J, Arroyo V, Rodés J. Bacterial infections in cirrhosis: epidemiological changes with invasive procedures and norfloxacin prophlaxis. Hepatology. 2002;35:140-8.
PubMed Abstract»Fernández J, Navasa M, Planas R, et al. Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology. 2007;133:818-24.
PubMed Abstract»Fernández J, Ruiz del Arbol L, Gomez C, et al. Norfloxacin vs ceftriaxone in the prophylaxis of infections in patients with advanced cirrhosis and hemorrhage. Gastroenterology. 2006;131:1049-56.
PubMed Abstract»Garcia-Tsao G, Lim JK; Members of Veterans Affairs Hepatitis C Resource Center Program. Management and treatment of patients with cirrhosis and portal hypertension: recommendations from the Department of Veterans Affairs Hepatitis C Resource Center Program and the National Hepatitis C Program. Am J Gastroenterol. 2009;104:1802-29.
PubMed Abstract»Ginés P, Rimola A, Planas R, et al. Norfloxacin prevents spontaneous bacterial peritonitis recurrence in cirrhosis: results of a double-blind, placebo-controlled trial. Hepatology. 1990;12:716-24.
PubMed Abstract»Goel A, Rahim U, Nguyen LH, Stave C, Nguyen MH. Systematic review with meta-analysis: rifaximin for the prophylaxis of spontaneous bacterial peritonitis. Aliment Pharmacol Ther. 2017;46:1029-1036.
PubMed Abstract»Novella M, Sola R, Soriano G, et al. Continuous versus inpatient prophylaxis of the first episode of spontaneous bacterial peritonitis with norfloxacin. Hepatology. 1997;25:532-6.
PubMed Abstract»Rimola A, Garcia-Tsao G, Navasa M, Piddock LJ, Planas R, Bernard B, Inadomi JM. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus statement. International Ascites Club. J Hepatol. 2000;32:142-53.
PubMed Abstract»Rolachon A, Cordier L, Bacq Y, et al. Ciprofloxacin and long-term prevention of spontaneous bacterial peritonitis: results of a prospective controlled trial. Hepatology. 1995;22:1171-4.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Singh N, Gayowski T, Yu VL, Wagener MM. Trimethoprim-sulfamethoxazole for the prevention of spontaneous bacterial peritonitis in cirrhosis: a randomized trial. Ann Intern Med. 1995;122:595-8.
PubMed Abstract»Soriano G, Guarner C, Tomas A, et al. Norfloxacin prevents bacterial infection in cirrhotics with gastrointestinal hemorrhage. Gastroenterology. 1992;103;1267-72.
PubMed Abstract»Additional References
Akriviadis EA, Runyon BA. Utility of an algorithm in differentiating spontaneous from secondary bacterial peritonitis. Gastroenterology. 1990;98:127-33.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Garcia-Tsao G. Current Management of the Complications of Cirrhosis and Portal Hypertension: Variceal Hemorrhage, Ascites, and Spontaneous Bacterial Peritonitis. Dig Dis. 2016;34:382-6.
PubMed Abstract»Northup PG, Garcia-Pagan JC, Garcia-Tsao G, et al. Vascular Liver Disorders, Portal Vein Thrombosis, and Procedural Bleeding in Patients With Liver Disease: 2020 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;73:366-413.
PubMed Abstract»Runyon BA, Antillon MR, Akriviadis EA, McHutchinson JG. Bedside inoculation of blood culture bottles is superior to delayed inoculation in the detection of spontaneous bacterial peritonitis. J Clin Microbiol. 1990;28:2811-2.
PubMed Abstract»Runyon BA, McHutchinson JG, Antillon MR, Akriviadis EA, Montano A. Short-course versus long-course antibiotic treatment of spontaneous bacterial peritonitis: a randomized controlled trial of 100 patients. Gastroenterology. 1991;100:1737-42.
PubMed Abstract»Runyon BA. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009;49:2087-107.
PubMed Abstract»Sigal SH, Stanca CM, Fernandez J, Arroyo V, Navasa M. Restricted use of albumin for spontaneous bacterial peritonitis. Gut. 2007;56:597-9.
Gut»Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999;341:403-9.
PubMed Abstract»Wu SS, Lin OS, Chen Y-Y, Hwang KL, Soon MS, Keeffe EB. Ascitic fluid carcinoembryonic antigen and alkaline phosphatase levels for the differentiation of primary from secondary bacterial peritonitis with intestinal perforation. J Hepatol. 2001;34:215-21.
PubMed Abstract»Lesson 3. Screening for Varices and Prevention of Bleeding
Pathophysiology and Portal Dynamics
Bosch J, Abraldes JG, Berzigotti A, García-Pagan JC. The clinical use of HVPG measurements in chronic liver disease. Nat Rev Gastroenterol Hepatol. 2009;6:573-82.
PubMed Abstract»Brunner F, Berzigotti A, Bosch J. Prevention and treatment of variceal haemorrhage in 2017. Liver Int. 2017;37 Suppl 1:104-115.
PubMed Abstract»Burroughs AK, Triantos CK. Predicting failure to control bleeding and mortality in acute variceal bleeding. J Hepatol. 2008;48:185-8.
PubMed Abstract»Feu F, García-Pagán JC, Bosch J, et al. Relation between portal pressure response to pharmacotherapy and risk of recurrent variceal haemorrhage in patients with cirrhosis. Lancet. 1995;346:1056-9.
PubMed Abstract»Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335.
PubMed Abstract»Garcia-Tsao G, Bosch J, Groszmann RJ. Portal hypertension and variceal bleeding--unresolved issues. Summary of an American Association for the study of liver diseases and European Association for the study of the liver single-topic conference. Hepatology. 2008;47:1764-72.
AASLD & EASL Summary»Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010;362:823-32.
PubMed Abstract»Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922-38.
AASLD Practice Guidelines»Groszmann RJ, Wongcharatrawee S. The hepatic venous pressure gradient: anything worth doing should be done right. Hepatology. 2004;39:280-2.
PubMed Abstract»Haq I, Tripathi D. Recent advances in the management of variceal bleeding. Gastroenterol Rep (Oxf). 2017;5:113-126.
PubMed Abstract»Kaplan DE, Bosch J, Ripoll C, et al. AASLD practice guidance on risk stratification and management of portal hypertension and varices in cirrhosis. Hepatology. 2023 Oct 23. Online ahead of print.
PubMed Abstract»Diagnosing Clinically Significant Portal Hypertension and Predicting Varices
Chawla S, Katz A, Attar BM, Gupta A, Sandhu DS, Agarwal R. Platelet count/spleen diameter ratio to predict the presence of esophageal varices in patients with cirrhosis: a systematic review. Eur J Gastroenterol Hepatol. 2012;24:431-6.
PubMed Abstract»Colli A, Gana JC, Turner D, et al. Capsule endoscopy for the diagnosis of oesophageal varices in people with chronic liver disease or portal vein thrombosis. Cochrane Database Syst Rev. 2014;:CD008760.
PubMed Abstract»de Franchis R, Eisen GM, Laine L, et al. Esophageal capsule endoscopy for screening and surveillance of esophageal varices in patients with portal hypertension. Hepatology. 2008;47:1595-603.
PubMed Abstract»de Franchis R, Pascal JP, Ancona E, et al. Definitions, methodology and therapeutic strategies in portal hypertension. A Consensus Development Workshop, Baveno, Lake Maggiore, Italy, April 5 and 6, 1990. J Hepatol. 1992;15:256-61.
PubMed Abstract»de Franchis R. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63:743-52.
PubMed Abstract»de Franchis R. Updating consensus in portal hypertension: report of the Baveno III Consensus Workshop on definitions, methodology and therapeutic strategies in portal hypertension. J Hepatol. 2000;33:846-52.
PubMed Abstract»Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335.
PubMed Abstract»Garcia-Tsao G, Bosch J, Groszmann RJ. Portal hypertension and variceal bleeding--unresolved issues. Summary of an American Association for the study of liver diseases and European Association for the study of the liver single-topic conference. Hepatology. 2008;47:1764-72.
AASLD & EASL Summary»Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922-38.
AASLD Practice Guidelines»Groszmann RJ, Garcia-Tsao G, Bosch J, et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med. 2005;353:2254-61.
PubMed Abstract»Jakab SS, Garcia-Tsao G. Screening and Surveillance of Varices in Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2019;17:26-9.
PubMed Abstract»Kaplan DE, Bosch J, Ripoll C, et al. AASLD practice guidance on risk stratification and management of portal hypertension and varices in cirrhosis. Hepatology. 2023 Oct 23. Online ahead of print.
PubMed Abstract»Kovalak M, Lake J, Mattek N, Eisen G, Lieberman D, Zaman A. Endoscopic screening for varices in cirrhotic patients: data from a national endoscopic database. Gastrointest Endosc. 2007;65:82-8.
PubMed Abstract»Lim JK, Flamm SL, Singh S, Falck-Ytter YT. American Gastroenterological Association Institute Guideline on the Role of Elastography in the Evaluation of Liver Fibrosis. Gastroenterology. 2017;152:1536-1543.
PubMed Abstract»McCarty TR, Afinogenova Y, Njei B. Use of Wireless Capsule Endoscopy for the Diagnosis and Grading of Esophageal Varices in Patients With Portal Hypertension: A Systematic Review and Meta-Analysis. J Clin Gastroenterol. 2017;51:174-182.
PubMed Abstract»Merli M, Nicolini G, Angeloni S, et al. Incidence and natural history of small esophageal varices in cirrhotic patients. J Hepatol. 2003;38:266-72.
PubMed Abstract»Qu Y, Li T, Ye Q, Zhang L, Wang L. A Beginning or the End? A Meta-analysis to Assess the Diagnostic Accuracy of Transient Elastography for the Prediction of Esophageal Varices. Saudi J Gastroenterol. 2016;22:345-352.
PubMed Abstract»Schwarzenberger E, Meyer T, Golla V, Sahdala NP, Min AD. Utilization of platelet count spleen diameter ratio in predicting the presence of esophageal varices in patients with cirrhosis. J Clin Gastroenterol. 2010;44:146-50.
PubMed Abstract»Management of Compensated Cirrhosis with Clinically Significant Portal Hypertension
Kaplan DE, Bosch J, Ripoll C, et al. AASLD practice guidance on risk stratification and management of portal hypertension and varices in cirrhosis. Hepatology. 2023 Oct 23. Online ahead of print.
PubMed Abstract»Villanueva C, Albillos A, Genescà J, et al. β blockers to prevent decompensation of cirrhosis in patients with clinically significant portal hypertension (PREDESCI): a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2019;393:1597-1608.
PubMed Abstract»Villanueva C, Torres F, Sarin SK, et al. Carvedilol reduces the risk of decompensation and mortality in patients with compensated cirrhosis in a competing-risk meta-analysis. J Hepatol. 2022;77:1014-25.
PubMed Abstract»Prophylaxis of Variceal Bleeding
D’Amico G, Pagliaro L, Bosch J. Pharmacological treatment of portal hypertension: an evidence-based approach. Semin Liver Dis. 1999;19:475-505.
PubMed Abstract»de Franchis R, Pascal JP, Ancona E, et al. Definitions, methodology and therapeutic strategies in portal hypertension. A Consensus Development Workshop, Baveno, Lake Maggiore, Italy, April 5 and 6, 1990. J Hepatol. 1992;15:256-61.
PubMed Abstract»de Franchis R; Baveno V Faculty. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010;53:762-8.
PubMed Abstract»Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335.
PubMed Abstract»Garcia-Tsao G, Bosch J, Groszmann RJ. Portal hypertension and variceal bleeding--unresolved issues. Summary of an American Association for the study of liver diseases and European Association for the study of the liver single-topic conference. Hepatology. 2008;47:1764-72.
AASLD & EASL Summary»Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922-38.
AASLD Practice Guidelines»Gluud LL, Krag A. Banding ligation versus beta-blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012;8:CD004544.
PubMed Abstract»Groszmann RJ, Garcia-Tsao G, Bosch J, et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med. 2005;353:2254-61.
PubMed Abstract»Haq I, Tripathi D. Recent advances in the management of variceal bleeding. Gastroenterol Rep (Oxf). 2017;5:113-126.
PubMed Abstract»Kaplan DE, Bosch J, Ripoll C, et al. AASLD practice guidance on risk stratification and management of portal hypertension and varices in cirrhosis. Hepatology. 2023 Oct 23. Online ahead of print.
PubMed Abstract»Li T, Ke W, Sun P, et al. Carvedilol for portal hypertension in cirrhosis: systematic review with meta-analysis. BMJ Open. 2016;6:e010902.
PubMed Abstract»Merkel C, Marin R, Angeli P, et al. A placebo-controlled clinical trial of nadolol in the prophylaxis of growth of small esophageal varices in cirrhosis. Gastroenterology. 2004; 127:476-84.
PubMed Abstract»Merli M, Nicolini G, Angeloni S, et al. Incidence and natural history of small esophageal varices in cirrhotic patients. J Hepatol. 2003;38:266-72.
PubMed Abstract»North Italian Endoscopic Club for the Study and Treatment of Esophageal Varices. Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter study. N Engl J Med. 1988;319:983-9.
PubMed Abstract»Reiberger T, Ulbrich G, Ferlitsch A, et al. Carvedilol for primary prophylaxis of variceal bleeding in cirrhotic patients with haemodynamic non-response to propranolol. Gut. 2013;62:1634-41.
PubMed Abstract»Sarin SK, Wadhawan M, Agarwal SR, Tyagi P, Sharma BC. Endoscopic variceal ligation plus propranolol versus endoscopic variceal ligation alone in primary prophylaxis of variceal bleeding. Am J Gastroenterol. 2005;100:797-804.
PubMed Abstract»Tripathi D, Ferguson JW, Kochar N, et al. Randomized controlled trial of carvedilol versus band ligation for the prevention of the first variceal bleed. Hepatology 2009;50:825-33.
PubMed Abstract»Treatment of Acute Variceal Bleeding
Akahoshi T, Hashizume M, Tomikawa M, et al. Long-term results of balloon-occluded retrograde transvenous obliteration for gastric variceal bleeding and risky gastric varices: a 10-year experience. J Gastroenterol Hepatol. 2008;23:1702-9.
PubMed Abstract»Altamirano J, Augustin S, Muntaner L, et al. [Predicting very early rebleeding after acute variceal bleeding based in classification and regression tree analysis (CRTA).]. Rev Gastroenterol Mex. 2010;75:12-21.
PubMed Abstract»Augustin S, Muntaner L, Altamirano JT, et al. Predicting early mortality after acute variceal hemorrhage based on classification and regression tree analysis. Clin Gastroenterol Hepatol. 2009;7:1347-54.
PubMed Abstract»Bañares R, Albillos A, Rincón D, et al. Endoscopic treatment versus endoscopic plus pharmacologic treatment for acute variceal bleeding: a meta-analysis. Hepatology. 2002;35:609-15.
PubMed Abstract»Ben-Ari Z, Cardin F, McCormick AP, Wannamethee G, Burroughs AK. A predictive model for failure to control bleeding during acute variceal haemorrhage. J Hepatol. 1999;31:443-50.
PubMed Abstract»Bhutta AQ, Garcia-Tsao G. The Role of Medical Therapy for Variceal Bleeding. Gastrointest Endosc Clin N Am. 2015;25:479-90.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Bosch J, Thabut D, Albillos A, et al. Recombinant factor VIIa for variceal bleeding in patients with advanced cirrhosis: A randomized, controlled trial. Hepatology. 2008;47:1604-14.
PubMed Abstract»Bosch J, Thabut D, Bendtsen F, et al. Recombinant factor VIIa for upper gastrointestinal bleeding in patients with cirrhosis: a randomized, double-blind trial. Gastroenterology. 2004;127:1123-30.
PubMed Abstract»Carbonell N, Pauwels A, Serfaty L, Fourdan O, Lévy VG, Poupon R. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology. 2004;40:652-9.
PubMed Abstract»Chau TN, Patch D, Chan YW, Nagral A, Dick R, Burroughs AK. “Salvage” transjugular intrahepatic portosystemic shunts: gastric fundal compared with esophageal variceal bleeding. Gastroenterology. 1998;114:981-7.
PubMed Abstract»D'Amico G, Pagliaro L, Bosch J. The treatment of portal hypertension: a meta-analytic review. Hepatology. 1995;22:332-54.
PubMed Abstract»D’Amico G, De Franchis R; Cooperative Study Group. Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology. 2003;38:599-612.
PubMed Abstract»D’Amico G, Pagliaro L, Bosch J. Pharmacological treatment of portal hypertension: an evidence-based approach. Semin Liver Dis. 1999;19:475-505.
PubMed Abstract»Dave P, Romeu J, Messer J. Upper gastrointestinal bleeding in patients with portal hypertension: a reappraisal. J Clin Gastroenterol. 1983;5:113-5.
PubMed Abstract»de Franchis R, Pascal JP, Ancona E, et al. Definitions, methodology and therapeutic strategies in portal hypertension. A Consensus Development Workshop, Baveno, Lake Maggiore, Italy, April 5 and 6, 1990. J Hepatol. 1992;15:256-61.
PubMed Abstract»de Franchis R; Baveno V Faculty. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010;53:762-8.
PubMed Abstract»Escorsell À, Pavel O, Cárdenas A, et al. Esophageal balloon tamponade versus esophageal stent in controlling acute refractory variceal bleeding: A multicenter randomized, controlled trial. Hepatology. 2016;63:1957-67.
PubMed Abstract»Fernández J, Ruiz del Arbol L, Gomez C, et al. Norfloxacin vs ceftriaxone in the prophylaxis of infections in patients with advanced cirrhosis and hemorrhage. Gastroenterology. 2006;131:1049-56.
PubMed Abstract»García-Pagán JC, Caca K, Bureau C, et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362:2370-9.
PubMed Abstract»Garcia-Pagán JC, Di Pascoli M, Caca K, et al. Use of early-TIPS for high-risk variceal bleeding: results of a post-RCT surveillance study. J Hepatol. 2013;58:45-50.
PubMed Abstract»Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335.
PubMed Abstract»Garcia-Tsao G, Bosch J, Groszmann RJ. Portal hypertension and variceal bleeding--unresolved issues. Summary of an American Association for the study of liver diseases and European Association for the study of the liver single-topic conference. Hepatology. 2008;47:1764-72.
AASLD & EASL Summary»Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010;362:823-32.
PubMed Abstract»Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922-38.
AASLD Practice Guidelines»Haq I, Tripathi D. Recent advances in the management of variceal bleeding. Gastroenterol Rep (Oxf). 2017;5:113-126.
PubMed Abstract»Hung TH, Tsai CC, Tseng CW, Tseng KC, Hsieh YH, Tsai CC. No difference in mortality between terlipressin and somatostatin treatments in cirrhotic patients with esophageal variceal bleeding and renal functional impairment. Eur J Gastroenterol Hepatol. 2016;28:1275-9.
PubMed Abstract»Ioannou G, Douse J, Rockey DC. Terlipressin for acute variceal hemorrhage. Cochrane Database Syst Rev 2003;(1):CD002147.
PubMed Abstract»Kaplan DE, Bosch J, Ripoll C, et al. AASLD practice guidance on risk stratification and management of portal hypertension and varices in cirrhosis. Hepatology. 2023 Oct 23. Online ahead of print.
PubMed Abstract»Krige JE, Kotze UK, Distiller G, Shaw JM, Bornman PC. Predictive factors for rebleeding and death in alcoholic cirrhotic patients with acute variceal bleeding: a multivariate analysis. World J Surg. 2009;33:2127-35.
PubMed Abstract»Laine L, Cook D. Endoscopic ligation compared with sclerotherapy for treatment of esophageal variceal bleeding. A meta-analysis. Ann Intern Med. 1995;123:280-7.
PubMed Abstract»Lo GH, Lai KH, Cheng JS, Chen MH, Chiang HT. A prospective, randomized trial of butyl cyanoacrylate injection versus band ligation in the management of bleeding gastric varices. Hepatology. 2001;33:1060-4.
PubMed Abstract»Moitinho E, Escorsell A, Bandi JC, et al. Prognostic value of early measurements of portal pressure in acute variceal bleeding. Gastroenterology. 1999;117:626-31.
PubMed Abstract»Monescillo A, Martínez-Lagares F, Ruiz-del-Arbol L, et al. Influence of portal hypertension and its early decompression by TIPS placement on the outcome of variceal bleeding. Hepatology. 2004;40:793-801.
PubMed Abstract»Nadler J, Stankovic N, Uber A, et al. Outcomes in variceal hemorrhage following the use of a balloon tamponade device. Am J Emerg Med. 2017;35:1500-1502.
PubMed Abstract»Naparstek Y, Rachmilewitz D. UGI bleeding in a nonalcoholic population with portal hypertension. J Clin Gastroenterol. 1980;2:239-41.
PubMed Abstract»Rimola A, Garcia-Tsao G, Navasa M, Piddock LJ, Planas R, Bernard B, Inadomi JM. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus statement. International Ascites Club. J Hepatol. 2000;32:142-53.
PubMed Abstract»Rudler M, Cluzel P, Corvec TL, et al. Early-TIPSS placement prevents rebleeding in high-risk patients with variceal bleeding, without improving survival. Aliment Pharmacol Ther. 2014;40:1074-80.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Ryan BM, Stockbrugger RW, Ryan JM. A pathophysiologic, gastroenterologic, and radiologic approach to the management of gastric varices. Gastroenterology. 2004;126:1175-89.
PubMed Abstract»Saad WE, Wagner CC, Lippert A, et al. Protective value of TIPS against the development of hydrothorax/ascites and upper gastrointestinal bleeding after balloon-occluded retrograde transvenous obliteration (BRTO). Am J Gastroenterol. 2013;108:1612-9.
PubMed Abstract»Schoppe LE, Roark GD, Patterson M. Acute upper gastrointestinal bleeding in patients with portal hypertension: a correlation of endoscopic findings with etiology. South Med J. 1983;76:475-6.
PubMed Abstract»Seo YS, Park SY, Kim MY, et al. Lack of difference among terlipressin, somatostatin, and octreotide in the control of acute gastroesophageal variceal hemorrhage. Hepatology. 2014;60:954-63.
PubMed Abstract»Simpson E, Lin Y, Stanworth S, Birchall J, Doree C, Hyde C. Recombinant factor VIIa for the prevention and treatment of bleeding in patients without haemophilia. Cochrane Database Syst Rev. 2012;:CD005011.
PubMed Abstract»Tan PC, Hou MC, Lin HC, Liu TT, Lee FY, Chang FY, Lee SD. A randomized trial of endoscopic treatment of acute gastric variceal hemorrhage: N-butyl-2-cyanoacrylate injection versus band ligation. Hepatology. 2006;43:690-7.
PubMed Abstract»Villanueva C, Colomo A, Bosch A, et al. Transfusion strategies for acute gastrointestinal bleeding. N Engl J Med. 2013;368:11-21.
PubMed Abstract»Wells M, Chande N, Adams P, et al. Meta-analysis: vasoactive medications for the management of acute variceal bleeds. Aliment Pharmacol Ther. 2012;35:1267-78.
PubMed Abstract»Secondary Prophylaxis of Variceal Bleeding
Bosch J, García-Pagán JC. Prevention of variceal rebleeding. Lancet. 2003;361:952-4.
PubMed Abstract»Boyer TD, Haskal ZJ. The Role of Transjugular Intrahepatic Portosystemic Shunt (TIPS) in the Management of Portal Hypertension: update 2009. Hepatology. 2010;51:306.
PubMed Abstract»D’Amico G, Pagliaro L, Bosch J. Pharmacological treatment of portal hypertension: an evidence-based approach. Semin Liver Dis. 1999;19:475-505.
PubMed Abstract»García-Pagán JC, Caca K, Bureau C, et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362:2370-9.
PubMed Abstract»Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335.
PubMed Abstract»Garcia-Tsao G, Bosch J, Groszmann RJ. Portal hypertension and variceal bleeding--unresolved issues. Summary of an American Association for the study of liver diseases and European Association for the study of the liver single-topic conference. Hepatology. 2008;47:1764-72.
AASLD & EASL Summary»Garcia-Tsao G, Bosch J. Varices and Variceal Hemorrhage in Cirrhosis: A New View of an Old Problem. Clin Gastroenterol Hepatol. 2015;13:2109-17.
PubMed Abstract»Gluud LL, Langholz E, Krag A. Meta-analysis: isosorbide-mononitrate alone or with either beta-blockers or endoscopic therapy for the management of oesophageal varices. Aliment Pharmacol Ther. 2010;32:859-71.
PubMed Abstract»Gonzalez R, Zamora J, Gomez-Camarero J, Molinero LM, Bañares R, Albillos A. Meta-analysis: Combination endoscopic and drug therapy to prevent variceal rebleeding in cirrhosis. Ann Intern Med. 2008;149:109-22.
PubMed Abstract»Gournay J, Masliah C, Martin T, Perrin D, Galmiche JP. Isosorbide mononitrate and propranolol compared with propranolol alone for the prevention of variceal rebleeding. Hepatology 2000;31:1239-45.
PubMed Abstract»Haq I, Tripathi D. Recent advances in the management of variceal bleeding. Gastroenterol Rep (Oxf). 2017;5:113-126.
PubMed Abstract»Hayes PC, Davis JM, Lewis JA, Bouchier IA. Meta-analysis of value of propranolol in prevention of variceal haemorrhage. Lancet. 1990;336:153-6.
PubMed Abstract»Kravetz D. Prevention of recurrent esophageal variceal hemorrhage: review and current recommendations. J Clin Gastroenterol. 2007;41 Suppl 3:S318-22.
PubMed Abstract»Laine L, Cook D. Endoscopic ligation compared with sclerotherapy for treatment of esophageal variceal bleeding. A meta-analysis. Ann Intern Med. 1995;123:280-7.
PubMed Abstract»Lebrec D, Poynard T, Hillon P, Benhamou JP. Propranolol for prevention of recurrent gastrointestinal bleeding in patients with cirrhosis: a controlled study. N Engl J Med. 1981;305:1371-4.
PubMed Abstract»Lo GH, Lai KH, Cheng JS, Chen MH, Huang HC, Hsu PI, Lin CK. Endoscopic variceal ligation plus nadolol and sucralfate compared with ligation alone for the prevention of variceal rebleeding: a prospective, randomized trial. Hepatology. 2000;32:461-5.
PubMed Abstract»Lo GH, Liang HL, Chen WC, et al. A prospective, randomized controlled trial of transjugular intrahepatic portosystemic shunt versus cyanoacrylate injection in the prevention of gastric variceal rebleeding. Endoscopy. 2007;39:679-85.
PubMed Abstract»Pérez-Ayuso RM, Piqué JM, Bosch J, et al. Propranolol in prevention of recurrent bleeding from severe portal hypertensive gastropathy in cirrhosis. Lancet. 1991;337:1431-4.
PubMed Abstract»Saad WE. Balloon-occluded retrograde transvenous obliteration of gastric varices: concept, basic techniques, and outcomes. Semin Intervent Radiol. 2012;29:118-28.
PubMed Abstract»Sarin SK, Wadhawan M, Agarwal SR, Tyagi P, Sharma BC. Endoscopic variceal ligation plus propranolol versus endoscopic variceal ligation alone in primary prophylaxis of variceal bleeding. Am J Gastroenterol. 2005;100:797-804.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Brunner F, Berzigotti A, Bosch J. Prevention and treatment of variceal haemorrhage in 2017. Liver Int. 2017;37 Suppl 1:104-115.
PubMed Abstract»Fernández J, Ruiz del Arbol L, Gomez C, et al. Norfloxacin vs ceftriaxone in the prophylaxis of infections in patients with advanced cirrhosis and hemorrhage. Gastroenterology. 2006;131:1049-56.
PubMed Abstract»Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335.
PubMed Abstract»Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010;362:823-32.
PubMed Abstract»Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922-38.
AASLD Practice Guidelines»Haq I, Tripathi D. Recent advances in the management of variceal bleeding. Gastroenterol Rep (Oxf). 2017;5:113-126.
PubMed Abstract»Holster IL, Tjwa ET, Moelker A, et al. Covered transjugular intrahepatic portosystemic shunt versus endoscopic therapy + β-blocker for prevention of variceal rebleeding. Hepatology. 2016;63:581-9.
PubMed Abstract»Kaplan DE, Bosch J, Ripoll C, et al. AASLD practice guidance on risk stratification and management of portal hypertension and varices in cirrhosis. Hepatology. 2023 Oct 23. Online ahead of print.
PubMed Abstract»Krige JE, Kotze UK, Distiller G, Shaw JM, Bornman PC. Predictive factors for rebleeding and death in alcoholic cirrhotic patients with acute variceal bleeding: a multivariate analysis. World J Surg. 2009;33:2127-35.
PubMed Abstract»Mandorfer M, Reiberger T. Beta blockers and cirrhosis, 2016. Dig Liver Dis. 2017;49:3-10.
PubMed Abstract»Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-3.
PubMed Abstract»Lesson 4. Diagnosis and Management of Hepatic Encephalopathy
Background
Bajaj BS. Review article: the modern management of hepatic encephalopathy. Aliment Pharmacol Ther. 2010;31:537-47.
PubMed Abstract»Bajaj JS, Cordoba J, Mullen KD, Amodio P, Shawcross DL, Butterworth RF, Morgan MY. Review article: the design of clinical trials in hepatic encephalopathy – an International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN) consensus statement. Aliment Pharmacol Ther. 2011;33:739-47.
PubMed Abstract»Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT. Hepatic encephalopathy--definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology. 2002;35:716-21.
PubMed Abstract»Fichet J, Mercier E, Genée O, et al. Prognosis and 1-year mortality of intensive care unit patients with severe hepatic encephalopathy. J Crit Care. 2009;24:364-70.
PubMed Abstract»García-Martínez R, Simón-Talero M, Córdoba J. Prognostic assessment in patients with hepatic encephalopathy. Dis Markers. 2011;31:171-9.
PubMed Abstract»Hadjihambi A, Arias N, Sheikh M, Jalan R. Hepatic encephalopathy: a critical current review. Hepatol Int. 2018;12:135-147.
PubMed Abstract»Liere V, Sandhu G, DeMorrow S. Recent advances in hepatic encephalopathy. F1000Res. 2017;6:1637.
PubMed Abstract»Prakash R, Mullen KD. Mechanisms, diagnosis and management of hepatic encephalopathy. Nat Rev Gastroenterol Hepatol. 2010;7:515-25.
PubMed Abstract»Tapper EB, Parikh ND. Diagnosis and Management of Cirrhosis and Its Complications: A Review. JAMA. 2023;329:1589-1602.
PubMed Abstract»Thornburg B. Hepatic Encephalopathy following Transjugular Intrahepatic Portosystemic Shunt Placement. Semin Intervent Radiol. 2023;40:262-8.
PubMed Abstract»Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60:715-35.
PubMed Abstract»Clinical Features
Atterbury CE, Maddrey WC, Conn HO. Neomycin-sorbitol and lactulose in the treatment of acute portal-systemic encephalopathy. A controlled, double-blind clinical trial. Am J Dig Dis. 1978;23:398-406.
PubMed Abstract»Bajaj BS. Review article: the modern management of hepatic encephalopathy. Aliment Pharmacol Ther. 2010;31:537-47.
PubMed Abstract»Bajaj JS, Cordoba J, Mullen KD, Amodio P, Shawcross DL, Butterworth RF, Morgan MY. Review article: the design of clinical trials in hepatic encephalopathy – an International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN) consensus statement. Aliment Pharmacol Ther. 2011;33:739-47.
PubMed Abstract»Bajaj JS, Wade JB, Sanyal AJ. Spectrum of neurocognitive impairment in cirrhosis: Implications for the assessment of hepatic encephalopathy. Hepatology. 2009;50:2014-21.
PubMed Abstract»Conn HO, Leevy CM, Vlahcevic ZR, Rodgers JB, Maddrey WC, Seeff L, Levy LL. Comparison of lactulose and neomycin in the treatment of chronic portal-systemic encephalopathy. A double blind controlled trial. Gastroenterology. 1977;72:573-83.
PubMed Abstract»Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT. Hepatic encephalopathy--definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology. 2002;35:716-21.
PubMed Abstract»Hassanein T, Blei AT, Perry W, et al. Performance of the hepatic encephalopathy scoring algorithm in a clinical trial of patients with cirrhosis and severe hepatic encephalopathy. Am J Gastroenterol. 2009;104:1392-400.
PubMed Abstract»Hassanein TI, Hilsabeck RC, Perry W. Introduction to the Hepatic Encephalopathy Scoring Algorithm (HESA). Dig Dis Sci. 2008;53:529-38.
PubMed Abstract»Liere V, Sandhu G, DeMorrow S. Recent advances in hepatic encephalopathy. F1000Res. 2017;6:1637.
PubMed Abstract»Mouri S, Tripon S, Rudler M, et al. FOUR score, a reliable score for assessing overt hepatic encephalopathy in cirrhotic patients. Neurocrit Care. 2015;22:251-7.
PubMed Abstract»Ortiz M, Córdoba J, Doval E, et al. Development of a clinical hepatic encephalopathy staging scale. Aliment Pharmacol Ther. 2007;26:859-67.
PubMed Abstract»Poordad FF. Review articles: the burden of hepatic encephalopathy. Aliment Pharmacol Ther. 2007; 25 Suppl 1:3-9.
PubMed Abstract»Prakash R, Mullen KD. Mechanisms, diagnosis and management of hepatic encephalopathy. Nat Rev Gastroenterol Hepatol. 2010;7:515-25.
PubMed Abstract»Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81-4.
PubMed Abstract»Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60:715-35.
PubMed Abstract»Wijdicks EF, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a new coma scale: The FOUR score. Ann Neurol. 2005;58:585-93.
PubMed Abstract»Wijdicks EF, Rabinstein AA, Bamlet WR, Mandrekar JN. FOUR score and Glasgow Coma Scale in predicting outcome of comatose patients: a pooled analysis. Neurology. 2011;77:84-5.
PubMed Abstract»Diagnosis and Testing
Amodio P, Del Piccolo F, Marchetti P, et al. Clinical features and survivial of cirrhotic patients with subclinical cognitive alterations detected by the number connection test and computerized psychometric tests. Hepatology. 1999;29:1662-7.
PubMed Abstract»Amodio P, Ridola L, Schiff S, et al. Improving the inhibitory control task to detect minimal hepatic encephalopathy. Gastroenterology. 2010;139:510-8, 518.e1-2.
PubMed Abstract»Bajaj BS. Review article: the modern management of hepatic encephalopathy. Aliment Pharmacol Ther. 2010;31:537-47.
PubMed Abstract»Bajaj JS, Cordoba J, Mullen KD, Amodio P, Shawcross DL, Butterworth RF, Morgan MY. Review article: the design of clinical trials in hepatic encephalopathy – an International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN) consensus statement. Aliment Pharmacol Ther. 2011;33:739-47.
PubMed Abstract»Bajaj JS, Hafeezullah M, Franco J, et al. Inhibitory control test for the diagnosis of minimal hepatic encephalopathy. Gastroenterology. 2008;135:1591-1600.e1.
PubMed Abstract»Bajaj JS, Heuman DM, Hylemon PB, et al. Randomised clinical trial: Lactobacillus GG modulates gut microbiome, metabolome and endotoxemia in patients with cirrhosis. Aliment Pharmacol Ther. 2014;39:1113-25.
PubMed Abstract»Bajaj JS, Heuman DM, Sterling RK, et al. Validation of EncephalApp, Smartphone-Based Stroop Test, for the Diagnosis of Covert Hepatic Encephalopathy. Clin Gastroenterol Hepatol. 2015;13:1828-1835.e1.
PubMed Abstract»Bajaj JS, Pinkerton SD, Sanyal AJ, Heuman DM. Diagnosis and treatment of minimal hepatic encephalopathy to prevent motor vehicle accidents: a cost-effectiveness analysis. Hepatology. 2012;55:1164-71.
PubMed Abstract»Bajaj JS, Saeian K, Schubert CM, et al. Minimal hepatic encephalopathy is associated with motor vehicle crashes: the reality beyond the driving test. Hepatology. 2009;50:1175-83.
PubMed Abstract»Bajaj JS, Saeian K, Verber MD, et al. Inhibitory control test is a simple method to diagnose minimal hepatic encephalopathy and predict development of overt hepatic encephalopathy. Am J Gastroenterol. 2007;102:754-60.
PubMed Abstract»Bajaj JS, Thacker LR, Heuman DM, et al. The Stroop smartphone application is a short and valid method to screen for minimal hepatic encephalopathy. Hepatology. 2013;58:1122-32.
PubMed Abstract»Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT. Hepatic encephalopathy--definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology. 2002;35:716-21.
PubMed Abstract»Kircheis G, Hilger N, Häussinger D. Value of critical flicker frequency and psychometric hepatic encephalopathy score in diagnosis of low-grade hepatic encephalopathy. Gastroenterology. 2014;146:961-9.
PubMed Abstract»Kircheis G, Wettstein M, Timmermann L, Schnitzler A, Häussinger D. Critical flicker frequency for quantification of low-grade hepatic encephalopathy. Hepatology. 2002;35:357-66.
PubMed Abstract»Kramer L, Tribl B, Gendo A, Zauner C, Schneider B, Ferenci P, Madl C. Partial pressure of ammonia versus ammonia in hepatic encephalopathy. Hepatology. 2000;31:30-4.
PubMed Abstract»Krieger S, Jauss M, Jansen O, Theilmann L, Geissler M, Krieger D. Neuropsychiatric profile and hyperintense globus pallidus on T1-weighted magnetic resonance images in liver cirrhosis. Gastroenterology. 1996;111:147-55.
PubMed Abstract»Lauridsen MM, Mikkelsen S, Svensson T, et al. The continuous reaction time test for minimal hepatic encephalopathy validated by a randomized controlled multi-modal intervention-A pilot study. PLoS One. 2017;12:e0185412.
PubMed Abstract»Lauridsen MM, Thiele M, Kimer N, Vilstrup H. The continuous reaction times method for diagnosing, grading, and monitoring minimal/covert hepatic encephalopathy. Metab Brain Dis. 2013;28:231-4.
PubMed Abstract»Morris H, Kaplan PW, Kane N. Electroencephalography in encephalopathy and encephalitis. Pract Neurol. 2024;24:2-10.
PubMed Abstract»Nabi E, Bajaj JS. Useful tests for hepatic encephalopathy in clinical practice. Curr Gastroenterol Rep. 2014;16:362.
PubMed Abstract»Ong JP, Aggarwal A, Krieger D, et al. Correlation between ammonia levels and the severity of hepatic encephalopathy. Am J Med. 2003;15;114:188-93.
PubMed Abstract»Prakash R, Mullen KD. Mechanisms, diagnosis and management of hepatic encephalopathy. Nat Rev Gastroenterol Hepatol. 2010;7:515-25.
PubMed Abstract»Randolph C, Hilsabeck R, Kato A, et al. Neuropsychological assessment of hepatic encephalopathy: ISHEN practice guidelines. Liver Int. 2009;29:629-35.
PubMed Abstract»Sotil EU, Gottstein J, Ayala E, Randolph C, Blei AT. Impact of preoperative overt hepatic encephalopathy on neurocognitive function after liver transplantation. Liver Transpl. 2009;15:184-92.
PubMed Abstract»Tapper EB, Parikh ND, Waljee AK, Volk M, Carlozzi NE, Lok AS. Diagnosis of Minimal Hepatic Encephalopathy: A Systematic Review of Point-of-Care Diagnostic Tests. Am J Gastroenterol. 2018;113:529-538.
PubMed Abstract»Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60:715-35.
PubMed Abstract»Weissenborn K, Ennen JC, Schomerus H, Rückert N, Hecker H. Neuropsychological characterization of hepatic encephalopathy. J Hepatol. 2001;34:768-73.
PubMed Abstract»Weissenborn K. Diagnosis of minimal hepatic encephalopathy. J Clin Exp Hepatol. 2015;5:S54-9.
PubMed Abstract»Weissenborn K. Psychometric tests for diagnosing minimal hepatic encephalopathy. Metab Brain Dis. 2013;28:227-9.
PubMed Abstract»Zeegen R, Drinkwater JE, Dawson AM. Method for measuring cerebral dysfunction in patients with liver disease. Br Med J. 1970;2(5710):633-6.
PubMed Abstract»Approach to the Management of Hepatic Encephalopathy
Bajaj BS. Review article: the modern management of hepatic encephalopathy. Aliment Pharmacol Ther. 2010;31:537-47.
PubMed Abstract»Bustamante J, Rimola A, Ventura PJ, Navasa M, Cirera I, Reggiardo V, Rodés J. Prognostic significance of hepatic encephalopathy in patients with cirrhosis. J Hepatol. 1999;30:890-5.
PubMed Abstract»Laleman W, Simon-Talero M, Maleux G, et al. Embolization of large spontaneous portosystemic shunts for refractory hepatic encephalopathy: a multicenter survey on safety and efficacy. Hepatology. 2013;57:2448-57.
PubMed Abstract»Lv Y, Chen H, Luo B, et al. Concurrent large spontaneous portosystemic shunt embolization for the prevention of overt hepatic encephalopathy after TIPS: A randomized controlled trial. Hepatology. 2022;76:676-88.
PubMed Abstract»Prakash R, Mullen KD. Mechanisms, diagnosis and management of hepatic encephalopathy. Nat Rev Gastroenterol Hepatol. 2010;7:515-25.
PubMed Abstract»Strauss E, da Costa MF. The importance of bacterial infections as precipating factors of chronic hepatic encephalopathy in cirrhosis. Hepatogastroenterology. 1998;45:900-4.
PubMed Abstract»Strauss E, Gomes de Sá Ribeiro Mde F. Bacterial infections associated with hepatic encephalopathy: prevalence and outcome. Ann Hepatol. 2003;2:41-5.
PubMed Abstract»Strauss E, Tramote R, Silva EP, et al. Double-blind randomized clinical trial comparing neomycin and placebo in the treatment of exogenous hepatic encephalopathy. Hepatogastroenterology. 1992;39:542-5.
PubMed Abstract»Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60:715-35.
PubMed Abstract»Medical Therapy for Overt Hepatic Encephalopathy
Agrawal A, Sharma BC, Sharma P, Sarin SK. Secondary prophylaxis of hepatic encephalopathy in cirrhosis: an open-label, randomized controlled trial of lactulose, probiotics, and no therapy. Am J Gastroenterol. 2012;107:1043-50.
PubMed Abstract»Als-Nielsen B, Gluud LL, Gluud C. Non-absorbable disaccharides for hepatic encephalopathy: a systematic review of randomized trials. BMJ. 2004;328:1046.
PubMed Abstract»Als-Nielsen B, Koretz RL, Kjaergard LL, Gluud C. Branched-chain amino acids for hepatic encephalopathy. Cochrane Database Syst Rev. 2003;(2):CD001939.
PubMed Abstract»Alter MJ, Kuhnert WL, Finelli L. Guidelines for laboratory testing and result reporting of antibody to hepatitis C virus. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2003;52:1-13, 15.
PubMed Abstract»Amodio P, Bemeur C, Butterworth R, et al. The nutritional management of hepatic encephalopathy in patients with cirrhosis: International Society for Hepatic Encephalopathy and Nitrogen Metabolism Consensus. Hepatology. 2013;58:325-36.
PubMed Abstract»Atterbury CE, Maddrey WC, Conn HO. Neomycin-sorbitol and lactulose in the treatment of acute portal-systemic encephalopathy. A controlled, double-blind clinical trial. Am J Dig Dis. 1978;23:398-406.
PubMed Abstract»Bajaj BS. Review article: the modern management of hepatic encephalopathy. Aliment Pharmacol Ther. 2010;31:537-47.
PubMed Abstract»Bass NM, Mullen KD, Sanyal A, et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362:1071-81.
PubMed Abstract»Córdoba J, López-Hellín J, Planas M, et al. Normal protein diet for episodic hepatic encephalopathy: results of a randomized study. J Hepatol. 2004;41:38-43.
PubMed Abstract»Cascino A, Cangiano C, Calcaterra V, Rossi-Fanelli F, Capocaccia L. Plasma amino acids imbalance in patients with liver disease. Am J Dig Dis. 1978;23:591-8.
PubMed Abstract»Chadalavada R, Sappati Biyyani RS, Maxwell, J, Mullen K. Nutrition in hepatic encephalopathy. Nutr Clin Pract. 2010;25:257-64.
PubMed Abstract»Chavez-Tapia NC, Cesar-Arce A, Barrientos-Gutiérrez T, Villegas-López FA, Méndez-Sanchez N, Uribe M. A systematic review and meta-analysis of the use of oral zinc in the treatment of hepatic encephalopathy. Nutr J. 2013;12:74.
PubMed Abstract»Conn HO, Leevy CM, Vlahcevic ZR, Rodgers JB, Maddrey WC, Seeff L, Levy LL. Comparison of lactulose and neomycin in the treatment of chronic portal-systemic encephalopathy. A double blind controlled trial. Gastroenterology. 1977;72:573-83.
PubMed Abstract»Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT. Hepatic encephalopathy--definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology. 2002;35:716-21.
PubMed Abstract»Gluud LL, Dam G, Les I, et al. Branched-chain amino acids for people with hepatic encephalopathy. Cochrane Database Syst Rev. 2017;5:CD001939.
PubMed Abstract»Hadjihambi A, Arias N, Sheikh M, Jalan R. Hepatic encephalopathy: a critical current review. Hepatol Int. 2018;12:135-147.
PubMed Abstract»Hawkins RA, Jessy J, Mans AM, Chedid A, DeJoseph MR. Neomycin reduces the intestinal production of ammonia from glutamine. Adv Exp Med Biol. 1994;368:125-34.
PubMed Abstract»Jawaro T, Yang A, Dixit D, Bridgeman MB. Management of Hepatic Encephalopathy: A Primer. Ann Pharmacother. 2016;50:569-77.
PubMed Abstract»Kircheis G, Nilius R, Held C, et al. Therapeutic efficacy of L-ornithine-L-aspartate infusions in patients with cirrhosis and hepatic encephalopathy: results of a placebo-controlled, double-blind study. Hepatology. 1997;25:1351-60.
PubMed Abstract»Knorr JP, Javed I, Sahni N, Cankurtaran CZ, Ortiz JA. Metronidazole-induced encephalopathy in a patient with end-stage liver disease. Case Reports Hepatol. 2012;2012:209258.
PubMed Abstract»Marchesini G, Fabbri A, Bianchi G, Brizi M, Zoli M. Zinc supplementation and amino acid-nitrogen metabolism in patients with advanced cirrhosis. Hepatology. 1996;23:1084-92.
PubMed Abstract»Mohammad RA, Regal RE, Alaniz C. Combination therapy for the treatment and prevention of hepatic encephalopathy. Ann Pharmacother. 2012;46:1559-63.
PubMed Abstract»Morgan MH, Read AE, Speller DC. Treatment of hepatic encephalopathy with metronidazole. Gut. 1982;23:1-7.
PubMed Abstract»Morgan MY, Marshall AW, Milsom JP, Sherlock S. Plasma amino-acid patterns in liver disease. Gut. 1982;23:362-70.
PubMed Abstract»Patel VC, Lee S, McPhail MJW, et al. Rifaximin-α reduces gut-derived inflammation and mucin degradation in cirrhosis and encephalopathy: RIFSYS randomised controlled trial. J Hepatol. 2022;76:332-42.
PubMed Abstract»Plauth M, Cabré E, Riggio O, et al. ESPEN Guidelines on Enteral Nutrition: Liver disease. Clin Nutr. 2006;25:285-94.
PubMed Abstract»Prakash R, Mullen KD. Mechanisms, diagnosis and management of hepatic encephalopathy. Nat Rev Gastroenterol Hepatol. 2010;7:515-25.
PubMed Abstract»Rahimi RS, Singal AG, Cuthbert JA, Rockey DC. Lactulose vs polyethylene glycol 3350--electrolyte solution for treatment of overt hepatic encephalopathy: the HELP randomized clinical trial. JAMA Intern Med. 2014;174:1727-33.
PubMed Abstract»Sanyal A, Younossi ZM, Bass NM, et al. Randomised clinical trial: rifaximin improves health-related quality of life in cirrhotic patients with hepatic encephalopathy - a double-blind placebo-controlled study. Aliment Pharmacol Ther. 2011;34:853-61.
PubMed Abstract»Sharma BC, Sharma P, Agrawal A, Sarin SK. Secondary prophylaxis of hepatic encephalopathy: an open-label randomized controlled trial of lactulose versus placebo. Gastroenterology. 2009;137:885-91, 891.e1.
PubMed Abstract»Sharma BC, Sharma P, Lunia MK, Srivastava S, Goyal R, Sarin SK. A randomized, double-blind, controlled trial comparing rifaximin plus lactulose with lactulose alone in treatment of overt hepatic encephalopathy. Am J Gastroenterol. 2013;108:1458-63.
PubMed Abstract»Swansson WD, Anderson BM, Yeoh SW, Lewis DJ. Management of minimal and overt hepatic encephalopathy with branched-chain amino acids: a review of the evidence. Eur J Gastroenterol Hepatol. 2023;35:812-21.
PubMed Abstract»Takuma Y, Nouso K, Makino Y, Hayashi M, Takahashi J. Clinical trial: oral zinc in hepatic encephalopathy. Aliment Pharmacol Ther. 2010; 32:1080-90.
PubMed Abstract»Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60:715-35.
PubMed Abstract»Watanabe A, Takesue A, Higashi T, Nagashima N. Serum amino acids in hepatic encephalopathy--effects of branched chain amino acid infusion on serum aminogram. Acta Hepatogastroenterol (Stuttg). 1979;26:346-57.
PubMed Abstract»Elwir S, Rahimi RS. Hepatic Encephalopathy: An Update on the Pathophysiology and Therapeutic Options. J Clin Transl Hepatol. 2017;5:142-151.
PubMed Abstract»European Association for the Study of the Liver. EASL Clinical Practice Guidelines on the management of hepatic encephalopathy. J Hepatol. 2022;77:807-24.
PubMed Abstract»Lyon KC, Likar E, Martello JL, Regier M. Retrospective cross-sectional pilot study of rifaximin dosing for the prevention of recurrent hepatic encephalopathy. J Gastroenterol Hepatol. 2017;32:1548-1552.
PubMed Abstract»Prakash R, Mullen KD. Mechanisms, diagnosis and management of hepatic encephalopathy. Nat Rev Gastroenterol Hepatol. 2010;7:515-25.
PubMed Abstract»Rahimi RS, Safadi R, Thabut D, et al. Efficacy and Safety of Ornithine Phenylacetate for Treating Overt Hepatic Encephalopathy in a Randomized Trial. Clin Gastroenterol Hepatol. 2021;19:2626-35.e7.
PubMed Abstract»Safadi R, Rahimi RS, Thabut D, et al. Pharmacokinetics/pharmacodynamics of L-ornithine phenylacetate in overt hepatic encephalopathy and the effect of plasma ammonia concentration reduction on clinical outcomes. Clin Transl Sci. 2022;15:1449-59.
PubMed Abstract»Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60:715-35.
PubMed Abstract»Lesson 5. Referral for Liver Transplantation
Background
Dultz G, Graubard BI, Martin P, et al. Liver transplantation for chronic hepatitis C virus infection in the United States 2002-2014: An analysis of the UNOS/OPTN registry. PLoS One. 2017;12:e0186898.
PubMed Abstract»Fayek SA, Quintini C, Chavin KD, Marsh CL. The Current State of Liver Transplantation in the United States: Perspective From American Society of Transplant Surgeons (ASTS) Scientific Studies Committee and Endorsed by ASTS Council. Am J Transplant. 2016;16:3093-3104.
PubMed Abstract»Flemming JA, Kim WR, Brosgart CL, Terrault NA. Reduction in liver transplant wait-listing in the era of direct-acting antiviral therapy. Hepatology. 2017;65:804-12.
PubMed Abstract»Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2016 Annual Data Report: Liver. Am J Transplant. 2018;18 Suppl 1:172-253.
PubMed Abstract»Kwong A, Kim WR, Lake JR, et al. OPTN/SRTR 2018 Annual Data Report: Liver. Am J Transplant. 2020;20 Suppl s1:193-299.
PubMed Abstract»Kwong AJ, Kim WR, Lake JR, et al. OPTN/SRTR 2022 Annual Data Report: Liver. Scientific Registry of Transplant Recipients. U.S. Department of Health and Human Resources
SRTR»O’Leary JG, Lepe R, Davis GL. Indications for liver transplantation. Gastroenterology. 2008. 134;1764-76.
PubMed Abstract»Organ Procurement and Transplantation Network (OPTN). National Data: Liver Transplantation in the United States. U.S. Department of Health and Human Services.
OPTN»The Scientific Registry of Transplant Recipients. OPTN/SRTR 2018 Annual Data Report: Liver. U.S. Department of Health and Human Services.
HRSA»Thuluvath PJ, Krok KL, Segev DL, Yoo HY. Trends in post-liver transplant survival in patients with hepatitis C between 1991 and 2001 in the United States. Liver Transpl. 2007;13:719-24.
PubMed Abstract»Indications for Liver Transplantation
Ahmad A, Torrazza-Perez E, Schilsky ML. Liver transplantation for Wilson disease. Handb Clin Neurol. 2017;142:193-204.
PubMed Abstract»Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020-2.
PubMed Abstract»Cha CH, Ruo L, Fong Y, Jarnagin WR, Shia J, Blumgart LH, DeMatteo RP. Resection of hepatocellular carcinoma in patients otherwise eligible for transplantation. Ann Surg. 2003;238:315-21.
PubMed Abstract»Charlton MR, Burns JM, Pedersen RA, Watt KD, Heimbach JK, Dierkhising RA. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology. 2011;141:1249-53.
PubMed Abstract»Cosarderelioglu C, Cosar AM, Gurakar M, Dagher NN, Gurakar A. Hepatopulmonary Syndrome and Liver Transplantation: A Recent Review of the Literature. J Clin Transl Hepatol. 2016;4:47-53.
PubMed Abstract»Cosarderelioglu C, Cosar AM, Gurakar M, et al. Portopulmonary Hypertension and Liver Transplant: Recent Review of the Literature. Exp Clin Transplant. 2016;14:113-20.
PubMed Abstract»D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-31.
PubMed Abstract»Darwish Murad S, Kim WR, Harnois DM, et al. Efficacy of neoadjuvant chemoradiation, followed by liver transplantation, for perihilar cholangiocarcinoma at 12 US centers. Gastroenterology. 2012;143:88-98.e3.
PubMed Abstract»Diehl AM, Day C. Cause, Pathogenesis, and Treatment of Nonalcoholic Steatohepatitis. N Engl J Med. 2017;377:2063-2072.
PubMed Abstract»Dienstag JL, Ghany MG, Morgan TR, et al. A prospective study of the rate of progression in compensated, histologically advanced chronic hepatitis C. Hepatology. 2011;54:396-405.
PubMed Abstract»Fattovich G, Giustina G, Degos F, et al. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology. 1997;112:463-72.
PubMed Abstract»Fayek SA, Quintini C, Chavin KD, Marsh CL. The Current State of Liver Transplantation in the United States: Perspective From American Society of Transplant Surgeons (ASTS) Scientific Studies Committee and Endorsed by ASTS Council. Am J Transplant. 2016;16:3093-3104.
PubMed Abstract»Ginés P, Quintero E, Arroyo V, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1987;7:122-8.
PubMed Abstract»Iqbal S, Smith KA, Khungar V. Hepatopulmonary Syndrome and Portopulmonary Hypertension: Implications for Liver Transplantation. Clin Chest Med. 2017;38:785-795.
PubMed Abstract»Kalra A, Wedd JP, Biggins SW. Changing prioritization for transplantation: MELD-Na, hepatocellular carcinoma exceptions, and more. Curr Opin Organ Transplant. 2016;21:120-6.
PubMed Abstract»Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2016 Annual Data Report: Liver. Am J Transplant. 2018;18 Suppl 1:172-253.
PubMed Abstract»Kwong A, Kim WR, Lake JR, et al. OPTN/SRTR 2018 Annual Data Report: Liver. Am J Transplant. 2020;20 Suppl s1:193-299.
PubMed Abstract»Kwong AJ, Kim WR, Lake JR, et al. OPTN/SRTR 2022 Annual Data Report: Liver. Scientific Registry of Transplant Recipients. U.S. Department of Health and Human Resources
SRTR»Lee WM, Stravitz RT, Larson AM. Introduction to the revised American Association for the Study of Liver Diseases Position Paper on acute liver failure 2011. Hepatology. 2012;55:965-7.
PubMed Abstract»Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144-65.
PubMed Abstract»Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693-9.
PubMed Abstract»Mehta N, Dodge JL, Grab JD, Yao FY. National Experience on Down-Staging of Hepatocellular Carcinoma Before Liver Transplant: Influence of Tumor Burden, Alpha-Fetoprotein, and Wait Time. Hepatology. 2020;71:943-54.
PubMed Abstract»Murray KF, Carithers RL Jr. AASLD practice guidelines: Evaluation of the patient for liver transplantation. Hepatology. 2005;41:1407-32.
PubMed Abstract»O’Leary JG, Lepe R, Davis GL. Indications for liver transplantation. Gastroenterology. 2008. 134;1764-76.
PubMed Abstract»Ostapowicz G, Fontana RJ, Schiødt FV, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137:947-54.
PubMed Abstract»Pelletier SJ, Fu S, Thyagarajan V, et al. An intention-to-treat analysis of liver transplantation for hepatocellular carcinoma using organ procurement transplant network data. Liver Transpl. 2009;15:859-68.
PubMed Abstract»Porres-Aguilar M, Zuckerman MJ, Figueroa-Casas JB, Krowka MJ. Portopulmonary hypertension: state of the art. Ann Hepatol. 2008;7:321-30.
PubMed Abstract»Propst A, Propst T, Zangerl G, Ofner D, Judmaier G, Vogel W. Prognosis and life expectancy in chronic liver disease. Dig Dis Sci. 1995;40:1805-15.
PubMed Abstract»Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646-9.
PubMed Abstract»Rodríguez-Roisin R, Krowka MJ. Hepatopulmonary syndrome--a liver-induced lung vascular disorder. N Engl J Med. 2008;358:2378-87.
PubMed Abstract»Silverman EK, Sandhaus RA. Clinical practice. Alpha1-antitrypsin deficiency. N Engl J Med. 2009;360:2749-57.
PubMed Abstract»Swanson KL, Wiesner RH, Krowka MJ. Natural history of hepatopulmonary syndrome: Impact of liver transplantation. Hepatology. 2005;41:1122-9.
PubMed Abstract»Swanson KL, Wiesner RH, Nyberg SL, Rosen CB, Krowka MJ. Survival in portopulmonary hypertension: Mayo Clinic experience categorized by treatment subgroups. Am J Transplant. 2008;8:2445-53.
PubMed Abstract»Thuluvath PJ, Krok KL, Segev DL, Yoo HY. Trends in post-liver transplant survival in patients with hepatitis C between 1991 and 2001 in the United States. Liver Transpl. 2007;13:719-24.
PubMed Abstract»United Network for Organ Sharing (UNOS). Transplants by Organ Type—2017. Data: Transplant Trends.
UNOS»Yang JD, Larson JJ, Watt KD, et al. Hepatocellular Carcinoma Is the Most Common Indication for Liver Transplantation and Placement on the Waitlist in the United States. Clin Gastroenterol Hepatol. 2017;15:767-775.e3.
PubMed Abstract»Yao FY, Xiao L, Bass NM, Kerlan R, Ascher NL, Roberts JP. Liver transplantation for hepatocellular carcinoma: validation of the UCSF-expanded criteria based on preoperative imaging. Am J Transplant. 2007;7:2587-96.
PubMed Abstract»Yu L, Ioannou GN. Survival of liver transplant recipients with hemochromatosis in the United States. Gastroenterology. 2007;133:489-95.
PubMed Abstract»Zardi EM, Zardi DM, Giorgi C, Chin D, Dobrina A. Portopulmonary hypertension and hepatorenal syndrome. Two faces of the same coin. Eur J Intern Med. 2017;43:22-27.
PubMed Abstract»Timing for Cirrhosis-Related Liver Transplantation
Child CG, Turcotte JG. Surgery and portal hypertension. Major Probl Clin Surg. 1964;1:1-85.
PubMed Abstract»D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-31.
PubMed Abstract»Fattovich G, Giustina G, Degos F, et al. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology. 1997;112:463-72.
PubMed Abstract»Freeman RB, Wiesner RH, Edwards E, Harper A, Merion R, Wolfe R; United Network for Organ Sharing Organ Procurement and Transplantation Network Liver and Transplantation Committee. Results of the first year of the new liver allocation plan. Liver Transpl. 2004;10:7-15.
PubMed Abstract»Ginés P, Quintero E, Arroyo V, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1987;7:122-8.
PubMed Abstract»Infante-Rivard C, Esnaola S, Villeneuve JP. Clinical and statistical validity of conventional prognostic factors in predicting short-term survival among cirrhotics. Hepatology. 1987;7:660-4.
PubMed Abstract»Kalra A, Wedd JP, Biggins SW. Changing prioritization for transplantation: MELD-Na, hepatocellular carcinoma exceptions, and more. Curr Opin Organ Transplant. 2016;21:120-6.
PubMed Abstract»Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464-70.
PubMed Abstract»Kim WR, Mannalithara A, Heimbach JK, et al. MELD 3.0: The Model for End-Stage Liver Disease Updated for the Modern Era. Gastroenterology. 2021;161:1887-95.
PubMed Abstract»Lucey MR, Brown KA, Everson GT, et al. Minimal criteria for placement of adults on the liver transplant waiting list: a report of a national conference organized by the American Society of Transplant Physicians and the American Association for the Study of Liver Diseases. Liver Transpl Surg. 1997;3:628-37.
PubMed Abstract»Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864-71.
PubMed Abstract»Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144-65.
PubMed Abstract»McDiarmid SV, Merion RM, Dykstra DM, Harper AM. Selection of pediatric candidates under the PELD system. Liver Transpl. 2004;10:S23-30.
PubMed Abstract»Murray KF, Carithers RL Jr. AASLD practice guidelines: Evaluation of the patient for liver transplantation. Hepatology. 2005;41:1407-32.
PubMed Abstract»O’Leary JG, Lepe R, Davis GL. Indications for liver transplantation. Gastroenterology. 2008. 134;1764-76.
PubMed Abstract»Oellerich M, Burdelski M, Lautz HU, Binder L, Pichlmayr R. Predictors of one-year pretransplant survival in patients with cirrhosis. Hepatology. 1991;14:1029-34.
PubMed Abstract»Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646-9.
PubMed Abstract»Wiesner R, Edwards E, Freeman R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91-6.
PubMed Abstract»Contraindications to Liver Transplantation
Cotter TG, Sandıkçı B, Paul S, et al. Liver transplantation for alcoholic hepatitis in the United States: Excellent outcomes with profound temporal and geographic variation in frequency. Am J Transplant. 2020 Jun 12. Online ahead of print.
PubMed Abstract»Lee BP, Chen PH, Haugen C, et al. Three-year Results of a Pilot Program in Early Liver Transplantation for Severe Alcoholic Hepatitis. Ann Surg. 2017;265:20-9.
PubMed Abstract»Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144-65.
PubMed Abstract»O’Leary JG, Lepe R, Davis GL. Indications for liver transplantation. Gastroenterology. 2008. 134;1764-76.
PubMed Abstract»Finding Information About Liver Transplant Centers
Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2016 Annual Data Report: Liver. Am J Transplant. 2018;18 Suppl 1:172-253.
PubMed Abstract»Transplantation Evaluation
Formica RN, Aeder M, Boyle G, et al. Simultaneous Liver-Kidney Allocation Policy: A Proposal to Optimize Appropriate Utilization of Scarce Resources. Am J Transplant. 2016;16:758-66.
PubMed Abstract»Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144-65.
PubMed Abstract»Murray KF, Carithers RL Jr. AASLD practice guidelines: Evaluation of the patient for liver transplantation. Hepatology. 2005;41:1407-32.
PubMed Abstract»O’Leary JG, Lepe R, Davis GL. Indications for liver transplantation. Gastroenterology. 2008. 134;1764-76.
PubMed Abstract»Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014-48.
PubMed Abstract»Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020-2.
PubMed Abstract»Child CG, Turcotte JG. Surgery and portal hypertension. Major Probl Clin Surg. 1964;1:1-85.
PubMed Abstract»Cholankeril G, Ahmed A. Alcoholic Liver Disease Replaces Hepatitis C Virus Infection as the Leading Indication for Liver Transplantation in the United States. Clin Gastroenterol Hepatol. 2018;16:1356-8.
PubMed Abstract»Diehl AM, Day C. Cause, Pathogenesis, and Treatment of Nonalcoholic Steatohepatitis. N Engl J Med. 2017;377:2063-2072.
PubMed Abstract»Durand F, Francoz C. The future of liver transplantation for viral hepatitis. Liver Int. 2017;37 Suppl 1:130-135.
PubMed Abstract»Gallegos-Orozco JF, Charlton MR. Alcoholic Liver Disease and Liver Transplantation. Clin Liver Dis. 2016;20:521-34.
PubMed Abstract»Ginés P, Quintero E, Arroyo V, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1987;7:122-8.
PubMed Abstract»Kalra A, Wedd JP, Biggins SW. Changing prioritization for transplantation: MELD-Na, hepatocellular carcinoma exceptions, and more. Curr Opin Organ Transplant. 2016;21:120-6.
PubMed Abstract»Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464-70.
PubMed Abstract»Kaplan DE, Bosch J, Ripoll C, et al. AASLD practice guidance on risk stratification and management of portal hypertension and varices in cirrhosis. Hepatology. 2023 Oct 23. Online ahead of print.
PubMed Abstract»Kim WR, Mannalithara A, Heimbach JK, et al. MELD 3.0: The Model for End-Stage Liver Disease Updated for the Modern Era. Gastroenterology. 2021;161:1887-95.
PubMed Abstract»Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864-71.
PubMed Abstract»Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144-65.
PubMed Abstract»Njei B, McCarty TR, Fortune BE, Lim JK. Optimal timing for hepatitis C therapy in US patients eligible for liver transplantation: a cost-effectiveness analysis. Aliment Pharmacol Ther. 2016;44:1090-1101.
PubMed Abstract»Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646-9.
PubMed Abstract»Shirazi F, Wang J, Wong RJ. Nonalcoholic Steatohepatitis Becomes the Leading Indication for Liver Transplant Registrants Among US Adults Born Between 1945 and 1965. J Clin Exp Hepatol. 2020;10:30-36.
PubMed Abstract»Wiesner R, Edwards E, Freeman R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91-6.
PubMed Abstract»Wong RJ, Singal AK. Trends in Liver Disease Etiology Among Adults Awaiting Liver Transplantation in the United States, 2014-2019. JAMA Netw Open. 2020;3:e1920294.
PubMed Abstract»Module 4. Evaluation and Preparation for Hepatitis C Treatment
Lesson 1. Goals and Benefits with HCV Treatment
Background
Asselah T, Marcellin P, Schinazi RF. Treatment of hepatitis C virus infection with direct-acting antiviral agents: 100% cure? Liver Int. 2018;38 Suppl 1:7-13.
PubMed Abstract»Cacoub P, Desbois AC, Comarmond C, Saadoun D. Impact of sustained virological response on the extrahepatic manifestations of chronic hepatitis C: a meta-analysis. Gut. 2018;67:2025-34.
PubMed Abstract»Marcellin F, Roux P, Protopopescu C, Duracinsky M, Spire B, Carrieri MP. Patient-reported outcomes with direct-acting antivirals for the treatment of chronic hepatitis C: current knowledge and outstanding issues. Expert Rev Gastroenterol Hepatol. 2017;11:259-268.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Tada T, Kumada T, Toyoda H, et al. Viral eradication reduces all-cause mortality, including non-liver-related disease, in patients with progressive hepatitis C virus-related fibrosis. J Gastroenterol Hepatol. 2017;32:687-694.
PubMed Abstract»van der Meer AJ, Veldt BJ, Feld JJ, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012;308:2584-93.
PubMed Abstract»Virologic Cure and Sustained Virologic Response
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Andersen ES, Moessner BK, Christensen PB, et al. Lower liver stiffness in patients with sustained virological response 4 years after treatment for chronic hepatitis C. Eur J Gastroenterol Hepatol. 2011;23:41-4.
PubMed Abstract»Arase Y, Suzuki F, Suzuki Y, et al. Sustained virological response reduces incidence of onset of type 2 diabetes in chronic hepatitis C. Hepatology. 2009;49:739-44.
PubMed Abstract»Backus LI, Boothroyd DB, Phillips BR, Belperio P, Halloran J, Mole LA. A sustained virologic response reduces risk of all-cause mortality in patients with hepatitis C. Clin Gastroenterol Hepatol. 2011;9:509-516.e1.
PubMed Abstract»Berenguer J, Rodríguez E, Miralles P, et al. Sustained virological response to interferon plus ribavirin reduces non-liver-related mortality in patients coinfected with HIV and Hepatitis C virus. Clin Infect Dis. 2012;55:728-36.
PubMed Abstract»Burgess SV, Hussaini T, Yoshida EM. Concordance of sustained virologic response at weeks 4, 12 and 24 post-treatment of hepatitis c in the era of new oral direct-acting antivirals: A concise review. Ann Hepatol. 2016;15:154-9.
PubMed Abstract»Butt AA, Wang X, Moore CG. Effect of hepatitis C virus and its treatment on survival. Hepatology. 2009;50:387-92.
PubMed Abstract»Chan J, Gogela N, Zheng H, et al. Direct-Acting Antiviral Therapy for Chronic HCV Infection Results in Liver Stiffness Regression Over 12 Months Post-treatment. Dig Dis Sci. 2018;63:486-492.
PubMed Abstract»Conjeevaram HS, Wahed AS, Afdhal N, Howell CD, Everhart JE, Hoofnagle JH. Changes in insulin sensitivity and body weight during and after peginterferon and ribavirin therapy for hepatitis C. Gastroenterology. 2010;140:469-77.
PubMed Abstract»Dieperink E, Pocha C, Thuras P, Knott A, Colton S, Ho SB. All-cause mortality and liver-related outcomes following successful antiviral treatment for chronic hepatitis C. Dig Dis Sci. 2014;59:872-80.
PubMed Abstract»Gane E, de Ledinghen V, Dylla DE, et al. Positive predictive value of sustained virologic response 4 weeks posttreatment for achieving sustained virologic response 12 weeks posttreatment in patients receiving glecaprevir/pibrentasvir in Phase 2 and 3 clinical trials. J Viral Hepat. 2021;28:1635-42.
PubMed Abstract»George SL, Bacon BR, Brunt EM, Mihindukulasuriya KL, Hoffmann J, Di Bisceglie AM. Clinical, virologic, histologic, and biochemical outcomes after successful HCV therapy: a 5-year follow-up of 150 patients. Hepatology. 2009;49:729-38.
PubMed Abstract»Ghany MG, Strader DB, Thomas DL, Seeff LB; American Association for the Study of Liver Diseases. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335-74.
AASLD Practice Guidelines»Innes H, Goldberg D, Dusheiko G, et al. Patient-important benefits of clearing the hepatitis C virus through treatment: a simulation model. J Hepatol. 2014;60:1118-26.
PubMed Abstract»Kutala BK, Guedj J, Asselah T, et al. Impact of treatment against hepatitis C virus on overall survival of naive patients with advanced liver disease. Antimicrob Agents Chemother. 2014;59:803-10.
PubMed Abstract»Lin CP, Liang PC, Huang CI, et al. Concordance of SVR12, SVR24 and SVR durability in Taiwanese chronic hepatitis C patients with direct-acting antivirals. PLoS One. 2021;16:e0245479.
PubMed Abstract»Marcellin P, Boyer N, Gervais A, et al. Long-term histologic improvement and loss of detectable intrahepatic HCV RNA in patients with chronic hepatitis C and sustained virologic response to interferon-alfa therapy. Ann Intern Med. 1997;127:875-81.
PubMed Abstract»Martinot-Peignoux M, Stern C, Maylin S, et al. Twelve weeks posttreatment follow-up is as relevant as 24 weeks to determine the sustained virologic response in patients with hepatitis C virus receiving pegylated interferon and ribavirin. Hepatology. 2010;51:1122-6.
PubMed Abstract»Maylin S, Martinot-Peignoux M, Moucari R, et al. Eradication of hepatitis C virus in patients successfully treated for chronic hepatitis C. Gastroenterology. 2008;135:821-9.
PubMed Abstract»Mira JA, Rivero-Juárez A, López-Cortés LF, et al. Benefits from sustained virologic response to pegylated interferon plus ribavirin in HIV/hepatitis C virus-coinfected patients with compensated cirrhosis. Clin Infect Dis. 2013;56:1646-53.
PubMed Abstract»Morisco F, Granata R, Stroffolini T, et al. Sustained virological response: a milestone in the treatment of chronic hepatitis C. World J Gastroenterol. 2013;19:2793-8.
PubMed Abstract»Page K, Hahn JA, Evans J, et al. Acute hepatitis C virus infection in young adult injection drug users: a prospective study of incident infection, resolution, and reinfection. J Infect Dis. 2009;200:1216-26.
PubMed Abstract»Pearlman BL, Traub N. Sustained virologic response to antiviral therapy for chronic hepatitis C virus infection: a cure and so much more. Clin Infect Dis. 2011;52:889-900.
PubMed Abstract»Pockros PJ, Hamzeh FM, Martin P, et al. Histologic outcomes in hepatitis C-infected patients with varying degrees of virologic response to interferon-based treatments. Hepatology. 2010;52:1193-200.
PubMed Abstract»Poynard T, McHutchison J, Manns M, et al. Impact of pegylated interferon alfa-2b and ribavirin on liver fibrosis in patients with chronic hepatitis C. Gastroenterology. 2002;122:1303-13.
PubMed Abstract»Simmons B, Saleem J, Heath K, Cooke GS, Hill A. Long-Term Treatment Outcomes of Patients Infected With Hepatitis C Virus: A Systematic Review and Meta-analysis of the Survival Benefit of Achieving a Sustained Virological Response. Clin Infect Dis. 2015;61:730-40.
PubMed Abstract»Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of Late Relapse or Reinfection With Hepatitis C Virus After Achieving a Sustained Virological Response: A Systematic Review and Meta-analysis. Clin Infect Dis. 2016;62:683-694.
PubMed Abstract»Singh S, Facciorusso A, Loomba R, Falck-Ytter YT. Magnitude and Kinetics of Decrease in Liver Stiffness After Antiviral Therapy in Patients With Chronic Hepatitis C: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2018;16:27-38.e4.
PubMed Abstract»Toccaceli F, Laghi V, Capurso L, Koch M, Sereno S, Scuderi M, Italian Hepanet Group. Long-term liver histology improvement in patients with chronic hepatitis C and sustained response to interferon. J Viral Hepat. 2003;10:126-33.
PubMed Abstract»van der Meer AJ, Veldt BJ, Feld JJ, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012;308:2584-93.
PubMed Abstract»Veldt BJ, Heathcote EJ, Wedemeyer H, et al. Sustained virologic response and clinical outcomes in patients with chronic hepatitis C and advanced fibrosis. Ann Intern Med. 2007;147:677-84.
PubMed Abstract»Yoshida EM, Sulkowski MS, Gane EJ, et al. Concordance of sustained virological response 4, 12, and 24 weeks post-treatment with sofosbuvir-containing regimens for hepatitis C virus. Hepatology. 2015;61:41-5.
PubMed Abstract»Impact of HCV Treatment on Clinical Outcomes
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»ANRS collaborative study group on hepatocellular carcinoma (ANRS CO22 HEPATHER, CO12 CirVir and CO23 CUPILT cohorts). . Lack of evidence of an effect of direct-acting antivirals on the recurrence of hepatocellular carcinoma: Data from three ANRS cohorts. J Hepatol. 2016;65:734-40.
PubMed Abstract»Arase Y, Suzuki F, Suzuki Y, et al. Sustained virological response reduces incidence of onset of type 2 diabetes in chronic hepatitis C. Hepatology. 2009;49:739-44.
PubMed Abstract»Arora SS, Axley P, Ahmed Z, et al. Decreasing frequency and improved outcomes of hepatitis C-related liver transplantation in the era of direct-acting antivirals - a retrospective cohort study. Transpl Int. 2019;32:854-64.
PubMed Abstract»Backus LI, Belperio PS, Shahoumian TA, Mole LA. Direct-acting antiviral sustained virologic response: Impact on mortality in patients without advanced liver disease. Hepatology. 2018;68:827-38.
PubMed Abstract»Backus LI, Belperio PS, Shahoumian TA, Mole LA. Impact of Sustained Virologic Response with Direct-Acting Antiviral Treatment on Mortality in Patients with Advanced Liver Disease. Hepatology. 2019;69:487-97.
PubMed Abstract»Backus LI, Boothroyd DB, Phillips BR, Belperio P, Halloran J, Mole LA. A sustained virologic response reduces risk of all-cause mortality in patients with hepatitis C. Clin Gastroenterol Hepatol. 2011;9:509-516.e1.
PubMed Abstract»Berenguer J, Rodríguez E, Miralles P, et al. Sustained virological response to interferon plus ribavirin reduces non-liver-related mortality in patients coinfected with HIV and Hepatitis C virus. Clin Infect Dis. 2012;55:728-36.
PubMed Abstract»Butt AA, Wang X, Moore CG. Effect of hepatitis C virus and its treatment on survival. Hepatology. 2009;50:387-92.
PubMed Abstract»Cabibbo G, Celsa C, Calvaruso V, et al. Direct-acting antivirals after successful treatment of early hepatocellular carcinoma improve survival in HCV-cirrhotic patients. J Hepatol. 2019;71:265-73.
PubMed Abstract»Cabibbo G, Petta S, Calvaruso V, et al. Is early recurrence of hepatocellular carcinoma in HCV cirrhotic patients affected by treatment with direct-acting antivirals? A prospective multicentre study. Aliment Pharmacol Ther. 2017;46:688-695.
PubMed Abstract»Cacoub P, Desbois AC, Comarmond C, Saadoun D. Impact of sustained virological response on the extrahepatic manifestations of chronic hepatitis C: a meta-analysis. Gut. 2018;67:2025-34.
PubMed Abstract»Calvaruso V, Cabibbo G, Cacciola I, et al. Incidence of Hepatocellular Carcinoma in Patients With HCV-Associated Cirrhosis Treated With Direct-Acting Antiviral Agents. Gastroenterology. 2018;155:411-21.e4.
PubMed Abstract»Chan J, Gogela N, Zheng H, et al. Direct-Acting Antiviral Therapy for Chronic HCV Infection Results in Liver Stiffness Regression Over 12 Months Post-treatment. Dig Dis Sci. 2018;63:486-492.
PubMed Abstract»Conjeevaram HS, Wahed AS, Afdhal N, Howell CD, Everhart JE, Hoofnagle JH. Changes in insulin sensitivity and body weight during and after peginterferon and ribavirin therapy for hepatitis C. Gastroenterology. 2010;140:469-77.
PubMed Abstract»Dieperink E, Pocha C, Thuras P, Knott A, Colton S, Ho SB. All-cause mortality and liver-related outcomes following successful antiviral treatment for chronic hepatitis C. Dig Dis Sci. 2014;59:872-80.
PubMed Abstract»El-Serag HB, Hampel H, Yeh C, Rabeneck L. Extrahepatic manifestations of hepatitis C among United States male veterans. Hepatology. 2002;36:1439-45.
PubMed Abstract»Ioannou GN, Feld JJ. What Are the Benefits of a Sustained Virologic Response to Direct-Acting Antiviral Therapy for Hepatitis C Virus Infection? Gastroenterology. 2019;156:446-460.e2.
PubMed Abstract»Ioannou GN, Green PK, Berry K. HCV eradication induced by direct-acting antiviral agents reduces the risk of hepatocellular carcinoma. J Hepatol. 2017. pii: S0168-8278(17)32273-0.
PubMed Abstract»Jacobson IM, Cacoub P, Dal Maso L, Harrison SA, Younossi ZM. Manifestations of chronic hepatitis C virus infection beyond the liver. Clin Gastroenterol Hepatol. 2010;8:1017-29.
PubMed Abstract»Kanwal F, Kramer J, Asch SM, Chayanupatkul M, Cao Y, El-Serag HB. Risk of Hepatocellular Cancer in HCV Patients Treated With Direct-Acting Antiviral Agents. Gastroenterology. 2017;153:996-1005.e1.
PubMed Abstract»Kim D, Li AA, Perumpail BJ, et al. Changing Trends in Etiology-Based and Ethnicity-Based Annual Mortality Rates of Cirrhosis and Hepatocellular Carcinoma in the United States. Hepatology. 2019;69:1064-74.
PubMed Abstract»Konjeti VR, John BV. Interaction Between Hepatocellular Carcinoma and Hepatitis C Eradication With Direct-acting Antiviral Therapy. Curr Treat Options Gastroenterol. 2018;16:203-214.
PubMed Abstract»Kutala BK, Guedj J, Asselah T, et al. Impact of treatment against hepatitis C virus on overall survival of naive patients with advanced liver disease. Antimicrob Agents Chemother. 2014;59:803-10.
PubMed Abstract»Laursen TL, Siggaard CB, Kazankov K, et al. Time-dependent improvement of liver inflammation, fibrosis and metabolic liver function after successful direct-acting antiviral therapy of chronic hepatitis C. J Viral Hepat. 2020;27:28-35.
PubMed Abstract»Li J, Gordon SC, Zhou Y, et al. Sex Differences in Extrahepatic Outcomes After Antiviral Treatment for Hepatitis C. Am J Gastroenterol. 2021;116:576-83.
PubMed Abstract»Mahale P, Engels EA, Li R, et al. The effect of sustained virological response on the risk of extrahepatic manifestations of hepatitis C virus infection. Gut. 2018;67:553-561.
PubMed Abstract»Mira JA, Rivero-Juárez A, López-Cortés LF, et al. Benefits from sustained virologic response to pegylated interferon plus ribavirin in HIV/hepatitis C virus-coinfected patients with compensated cirrhosis. Clin Infect Dis. 2013;56:1646-53.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Nahon P, Bourcier V, Layese R, et al. Eradication of Hepatitis C Virus Infection in Patients With Cirrhosis Reduces Risk of Liver and Non-Liver Complications. Gastroenterology. 2017;152:142-156.e2.
PubMed Abstract»Pearlman BL, Traub N. Sustained virologic response to antiviral therapy for chronic hepatitis C virus infection: a cure and so much more. Clin Infect Dis. 2011;52:889-900.
PubMed Abstract»Reig M, Mariño Z, Perelló C, et al. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J Hepatol. 2016;65:719-726.
PubMed Abstract»Saraiya N, Yopp AC, Rich NE, Odewole M, Parikh ND, Singal AG. Systematic review with meta-analysis: recurrence of hepatocellular carcinoma following direct-acting antiviral therapy. Aliment Pharmacol Ther. 2018;48:127-37.
PubMed Abstract»Singal AG, Lim JK, Kanwal F. AGA Clinical Practice Update on Interaction Between Oral Direct-Acting Antivirals for Chronic Hepatitis C Infection and Hepatocellular Carcinoma: Expert Review. Gastroenterology. 2019;156:2149-57.
PubMed Abstract»Singal AG, Rich NE, Mehta N, et al. Direct-Acting Antiviral Therapy for Hepatitis C Virus Infection Is Associated With Increased Survival in Patients With a History of Hepatocellular Carcinoma. Gastroenterology. 2019;157:1253-63.e2.
PubMed Abstract»Singal AG, Rich NE, Mehta N, et al. Direct-Acting Antiviral Therapy Not Associated With Recurrence of Hepatocellular Carcinoma in a Multicenter North American Cohort Study. Gastroenterology. 2019;156:1683-92.e1.
PubMed Abstract»Tang L, Marcell L, Kottilil S. Systemic manifestations of hepatitis C infection. Infect Agent Cancer. 2016;11:29.
PubMed Abstract»van der Meer AJ, Veldt BJ, Feld JJ, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012;308:2584-93.
PubMed Abstract»Veldt BJ, Heathcote EJ, Wedemeyer H, et al. Sustained virologic response and clinical outcomes in patients with chronic hepatitis C and advanced fibrosis. Ann Intern Med. 2007;147:677-84.
PubMed Abstract»Impact of HCV Treatment on Quality of Life
Asselah T, Bourgeois S, Pianko S, et al. Sofosbuvir/velpatasvir in patients with hepatitis C virus genotypes 1-6 and compensated cirrhosis or advanced fibrosis. Liver Int. 2018;38:443-450.
PubMed Abstract»Benhammou JN, Dong TS, May FP, et al. Race affects SVR12 in a large and ethnically diverse hepatitis C-infected patient population following treatment with direct-acting antivirals: Analysis of a single-center Department of Veterans Affairs cohort. Pharmacol Res Perspect. 2018;6:e00379.
PubMed Abstract»Curry MP, O'Leary JG, Bzowej N, et al. Sofosbuvir and Velpatasvir for HCV in Patients with Decompensated Cirrhosis. N Engl J Med. 2015;373:2618-28.
PubMed Abstract»Forns X, Lee SS, Valdes J, et al. Glecaprevir plus pibrentasvir for chronic hepatitis C virus genotype 1, 2, 4, 5, or 6 infection in adults with compensated cirrhosis (EXPEDITION-1): a single-arm, open-label, multicentre phase 3 trial. Lancet Infect Dis. 2017;17:1062-1068.
PubMed Abstract»Foster GR, Afdhal N, Roberts SK, et al. Sofosbuvir and velpatasvir for HCV genotype 2 and 3 infection. N Engl J Med. 2015;373:2608-17.
PubMed Abstract»Foster GR, Irving WL, Cheung MC, et al. Impact of direct acting antiviral therapy in patients with chronic hepatitis C and decompensated cirrhosis. J Hepatol. 2016;64:1224-31.
PubMed Abstract»Ge D, Fellay J, Thompson AJ, et al. Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature. 2009;461:399-401.
PubMed Abstract»Huang CF, Yang JF, Dai CY, et al. Efficacy and safety of pegylated interferon combined with ribavirin for the treatment of older patients with chronic hepatitis C. J Infect Dis. 2010;201:751-9.
PubMed Abstract»Huang CF, Yu ML. Treating hepatitis C in the elderly: pharmacotherapeutic considerations and developments. Expert Opin Pharmacother. 2017;18:1867-1874.
PubMed Abstract»Ioannou GN, Beste LA, Chang MF, et al. Effectiveness of Sofosbuvir, Ledipasvir/Sofosbuvir, or Paritaprevir/Ritonavir/Ombitasvir and Dasabuvir Regimens for Treatment of Patients With Hepatitis C in the Veterans Affairs National Health Care System. Gastroenterology. 2016;151:457-471.e5.
PubMed Abstract»Jacobson IM, Cacoub P, Dal Maso L, Harrison SA, Younossi ZM. Manifestations of chronic hepatitis C virus infection beyond the liver. Clin Gastroenterol Hepatol. 2010;8:1017-29.
PubMed Abstract»Kanwal F, Kramer JR, El-Serag HB, et al. Race and Gender Differences in the Use of Direct Acting Antiviral Agents for Hepatitis C Virus. Clin Infect Dis. 2016;63:291-9.
PubMed Abstract»Lawitz E, Gane E, Pearlman B, et al. Efficacy and safety of 12 weeks versus 18 weeks of treatment with grazoprevir (MK-5172) and elbasvir (MK-8742) with or without ribavirin for hepatitis C virus genotype 1 infection in previously untreated patients with cirrhosis and patients with previous null response with or without cirrhosis (C-WORTHY): a randomised, open-label phase 2 trial. Lancet. 2015;385:1075-86.
PubMed Abstract»Muir AJ, Bornstein JD, Killenberg PG. Peginterferon alfa-2b and ribavirin for the treatment of chronic hepatitis C in blacks and non-Hispanic whites. N Engl J Med. 2004;350:2265-71.
PubMed Abstract»Poordad F, Bronowicki JP, Gordon SC, et al. Factors that predict response of patients with hepatitis C virus infection to boceprevir. Gastroenterology. 2012;143:608-18.
PubMed Abstract»Rheem J, Sundaram V, Saab S. Antiviral Therapy in Elderly Patients With Hepatitis C Virus Infection. Gastroenterol Hepatol (N Y). 2015;11:294-346.
PubMed Abstract»Rodriguez-Torres M, Jeffers LJ, Sheikh MY, et al. Peginterferon alfa-2a and ribavirin in Latino and non-Latino whites with hepatitis C. N Engl J Med. 2009;360:257-67.
PubMed Abstract»Roth D, Nelson DR, Bruchfeld A, et al. Grazoprevir plus elbasvir in treatment-naive and treatment-experienced patients with hepatitis C virus genotype 1 infection and stage 4-5 chronic kidney disease (the C-SURFER study): a combination phase 3 study. Lancet. 2015;386:1537-45.
PubMed Abstract»Snyder HS, Ali B, Gonzalez HC, Nair S, Satapathy SK. Efficacy and Safety of Sofosbuvir-Based Direct Acting Antivirals for Hepatitis C in Septuagenarians and Octogenarians. J Clin Exp Hepatol. 2017;7:93-96.
PubMed Abstract»Stättermayer AF, Stauber R, Hofer H, et al. Impact of IL28B genotype on the early and sustained virologic response in treatment-naïve patients with chronic hepatitis C. Clin Gastroenterol Hepatol. 2011;9:344-50.
PubMed Abstract»Su F, Beste LA, Green PK, Berry K, Ioannou GN. Direct-acting antivirals are effective for chronic hepatitis C treatment in elderly patients: a real-world study of 17 487 patients. Eur J Gastroenterol Hepatol. 2017;29:686-693.
PubMed Abstract»Su F, Green PK, Berry K, Ioannou GN. The association between race/ethnicity and the effectiveness of direct antiviral agents for hepatitis C virus infection. Hepatology. 2017;65:426-438.
PubMed Abstract»Wilder JM, Jeffers LJ, Ravendhran N, et al. Safety and efficacy of ledipasvir-sofosbuvir in black patients with hepatitis C virus infection: A retrospective analysis of phase 3 data. Hepatology. 2016;63:437-44.
PubMed Abstract»Wilder JM, Muir A. Direct acting antivirals for the treatment of hepatitis C in ethnic minority populations. Expert Opin Pharmacother. 2018;19:451-456.
PubMed Abstract»Wyles D, Poordad F, Wang S, et al. Glecaprevir/pibrentasvir for hepatitis C virus genotype 3 patients with cirrhosis and/or prior treatment experience: A partially randomized phase 3 clinical trial. Hepatology. 2018;67:514-23.
PubMed Abstract»Younossi ZM, Stepanova M, Afdhal N, et al. Improvement of health-related quality of life and work productivity in chronic hepatitis C patients with early and advanced fibrosis treated with ledipasvir and sofosbuvir. J Hepatol. 2015;63:337-45.
PubMed Abstract»Younossi ZM, Stepanova M, Feld J, et al. Sofosbuvir/velpatasvir improves patient-reported outcomes in HCV patients: Results from ASTRAL-1 placebo-controlled trial. J Hepatol. 2016;65:33-9.
PubMed Abstract»Younossi ZM, Stepanova M, Jacobson IM, et al. Sofosbuvir and velpatasvir with or without voxilaprevir in direct-acting antiviral-naïve chronic hepatitis C: patient-reported outcomes from POLARIS 2 and 3. Aliment Pharmacol Ther. 2018;47:259-67.
PubMed Abstract»Younossi ZM, Stepanova M, Sulkowski M, Wyles D, Kottilil S, Hunt S. Patient-reported outcomes in patients co-infected with hepatitis C virus and human immunodeficiency virus treated with sofosbuvir and velpatasvir: The ASTRAL-5 study. Liver Int. 2017;37:1796-1804.
PubMed Abstract»Zeuzem S, Ghalib R, Reddy KR, et al. Grazoprevir-Elbasvir Combination Therapy for Treatment-Naive Cirrhotic and Noncirrhotic Patients With Chronic Hepatitis C Virus Genotype 1, 4, or 6 Infection: A Randomized Trial. Ann Intern Med. 2015;163:1-13.
PubMed Abstract»Impact of HCV Treatment on Survival
Arora SS, Axley P, Ahmed Z, et al. Decreasing frequency and improved outcomes of hepatitis C-related liver transplantation in the era of direct-acting antivirals - a retrospective cohort study. Transpl Int. 2019;32:854-64.
PubMed Abstract»Falade-Nwulia O, Suarez-Cuervo C, Nelson DR, Fried MW, Segal JB, Sulkowski MS. Oral Direct-Acting Agent Therapy for Hepatitis C Virus Infection: A Systematic Review. Ann Intern Med. 2017;166:637-48.
PubMed Abstract»Feld JJ, Foster GR. Second generation direct-acting antivirals - Do we expect major improvements? J Hepatol. 2016;65:S130-S142.
PubMed Abstract»Foster GR, Afdhal N, Roberts SK, et al. Sofosbuvir and velpatasvir for HCV genotype 2 and 3 infection. N Engl J Med. 2015;373:2608-17.
PubMed Abstract»Fried MW, Shiffman ML, Reddy KR, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med. 2002;347:975-82.
PubMed Abstract»Hadziyannis SJ, Sette H Jr, Morgan TR, et al. Peginterferon-alfa2a and ribavirin combination therapy in chronic hepatitis C: a randomized study of treatment duration and ribavirin dose. Ann Intern Med. 2004;140:346–55.
PubMed Abstract»Jacobson IM, McHutchison JG, Dusheiko G, et al. Telaprevir for previously untreated chronic hepatitis C virus infection. N Engl J Med. 2011;364:2405-16.
PubMed Abstract»Kim D, Li AA, Perumpail BJ, et al. Changing Trends in Etiology-Based and Ethnicity-Based Annual Mortality Rates of Cirrhosis and Hepatocellular Carcinoma in the United States. Hepatology. 2019;69:1064-74.
PubMed Abstract»Kim D, Perumpail BJ, Alshuwaykh O, Dennis BB, Cholankeril G, Ahmed A. Changing trends in aetiology-based hospitalizations with end-stage liver disease in the United States from 2016 to 2019. Liver Int. 2022;42:2390-5.
PubMed Abstract»Kowdley KV, Gordon SC, Reddy KR, et al. Ledipasvir and sofosbuvir for 8 or 12 weeks for chronic HCV without cirrhosis. N Engl J Med. 2014;370:1879-88.
PubMed Abstract»Manns MP, McHutchison JG, Gordon SC, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet. 2001;358:958-65.
PubMed Abstract»Poordad F, McCone J Jr, Bacon BR, et al. Boceprevir for untreated chronic HCV genotype 1 infection. N Engl J Med. 2011;364:1195-206.
PubMed Abstract»Scott JD, Gretch DR. Molecular diagnostics of hepatitis C virus infection: a systematic review. JAMA. 2007;297:724-32.
PubMed Abstract»Simmons B, Saleem J, Heath K, Cooke GS, Hill A. Long-Term Treatment Outcomes of Patients Infected With Hepatitis C Virus: A Systematic Review and Meta-analysis of the Survival Benefit of Achieving a Sustained Virological Response. Clin Infect Dis. 2015;61:730-40.
PubMed Abstract»Terrault NA, Zeuzem S, Di Bisceglie AM, et al. Effectiveness of Ledipasvir-Sofosbuvir Combination in Patients With Hepatitis C Virus Infection and Factors Associated With Sustained Virologic Response. Gastroenterology. 2016;151:1131-1140.e5.
PubMed Abstract»Wyles D, Poordad F, Wang S, et al. Glecaprevir/pibrentasvir for hepatitis C virus genotype 3 patients with cirrhosis and/or prior treatment experience: A partially randomized phase 3 clinical trial. Hepatology. 2018;67:514-23.
PubMed Abstract»Zeuzem S, Foster GR, Wang S, et al. Glecaprevir-Pibrentasvir for 8 or 12 Weeks in HCV Genotype 1 or 3 Infection. N Engl J Med. 2018;378:354-369.
PubMed Abstract»Zeuzem S, Rodríguez-Torres M, Rajender Reddy K, et al. Optimized threshold for serum HCV RNA to predict treatment outcomes in hepatitis C patients receiving peginterferon alfa-2a/ribavirin. J Viral Hepat. 2012;19:766-74.
PubMed Abstract»Population-Level Benefits of HCV Elimination
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy has failed: peginterferon plus ribavirin-experienced, genotype 5 or 6 patients with or without compensated cirrhosis
AASLD-IDSA Hepatitis C Guidance»Bacon BR, Gordon SC, Lawitz E, et al. Boceprevir for previously treated chronic HCV genotype 1 infection. N Engl J Med. 2011;364:1207-17.
PubMed Abstract»Charlton M, Everson GT, Flamm SL, et al. Ledipasvir and sofosbuvir plus ribavirin for treatment of HCV infection in patients with advanced liver disease. Gastroenterology. 2015;149:649-59.
PubMed Abstract»Chhatwal J, He T, Hur C, Lopez-Olivo MA. Direct-Acting Antiviral Agents for Patients With Hepatitis C Virus Genotype 1 Infection Are Cost-Saving. Clin Gastroenterol Hepatol. 2017;15:827-837.e8.
PubMed Abstract»Dhiman RK, Grover GS, Premkumar M, et al. Outcomes of Real-World Integrated HCV Microelimination for People Who Inject Drugs: An expansion of the Punjab Model. EClinicalMedicine. 2021;41:101148.
PubMed Abstract»Doyle JS, van Santen DK, Iser D, et al. Microelimination of Hepatitis C Among People With Human Immunodeficiency Virus Coinfection: Declining Incidence and Prevalence Accompanying a Multicenter Treatment Scale-up Trial. Clin Infect Dis. 2021;73:e2164-e2172.
PubMed Abstract»Fraser H, Martin NK, Brummer-Korvenkontio H, et al. Model projections on the impact of HCV treatment in the prevention of HCV transmission among people who inject drugs in Europe. J Hepatol. 2018;68:402-11.
PubMed Abstract»Fried MW, Shiffman ML, Reddy KR, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med. 2002;347:975-82.
PubMed Abstract»Goel A, Chen Q, Chhatwal J, Aggarwal R. Cost-effectiveness of generic pan-genotypic sofosbuvir/velpatasvir versus genotype-dependent direct-acting antivirals for hepatitis C treatment. J Gastroenterol Hepatol. 2018;33:2029-36.
PubMed Abstract»Hadziyannis SJ, Sette H Jr, Morgan TR, et al. Peginterferon-alfa2a and ribavirin combination therapy in chronic hepatitis C: a randomized study of treatment duration and ribavirin dose. Ann Intern Med. 2004;140:346–55.
PubMed Abstract»Hajarizadeh B, Grebely J, Byrne M, et al. Evaluation of hepatitis C treatment-as-prevention within Australian prisons (SToP-C): a prospective cohort study. Lancet Gastroenterol Hepatol. 2021;6:533-46.
PubMed Abstract»He T, Lopez-Olivo MA, Hur C, Chhatwal J. Systematic review: cost-effectiveness of direct-acting antivirals for treatment of hepatitis C genotypes 2-6. Aliment Pharmacol Ther. 2017;46:711-721.
PubMed Abstract»Ioannou GN, Beste LA, Chang MF, et al. Effectiveness of Sofosbuvir, Ledipasvir/Sofosbuvir, or Paritaprevir/Ritonavir/Ombitasvir and Dasabuvir Regimens for Treatment of Patients With Hepatitis C in the Veterans Affairs National Health Care System. Gastroenterology. 2016;151:457-471.e5.
PubMed Abstract»Jacobson IM, McHutchison JG, Dusheiko G, et al. Telaprevir for previously untreated chronic hepatitis C virus infection. N Engl J Med. 2011;364:2405-16.
PubMed Abstract»Kwo PY, Badshah MB. Treatment of HCV in Patients who Failed First-Generation PI Therapy: a Review of Current Literature. Curr Gastroenterol Rep. 2015;17:462.
PubMed Abstract»Manns MP, McHutchison JG, Gordon SC, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet. 2001;358:958-65.
PubMed Abstract»Martin NK, Vickerman P, Grebely J, et al. Hepatitis C virus treatment for prevention among people who inject drugs: Modeling treatment scale-up in the age of direct-acting antivirals. Hepatology. 2013;58:1598-609.
PubMed Abstract»Olafsson S, Fridriksdottir RH, Love TJ, et al. Cascade of care during the first 36 months of the treatment as prevention for hepatitis C (TraP HepC) programme in Iceland: a population-based study. Lancet Gastroenterol Hepatol. 2021;6:628-37.
PubMed Abstract»Padula WV, Levin JS, Lee J, Anderson GF. Cost-effectiveness of total state coverage for hepatitis C medications. Am J Manag Care. 2021;27:e171-e177.
PubMed Abstract»Poordad F, Bronowicki JP, Gordon SC, et al. Factors that predict response of patients with hepatitis C virus infection to boceprevir. Gastroenterology. 2012;143:608-18.
PubMed Abstract»Poordad F, McCone J Jr, Bacon BR, et al. Boceprevir for untreated chronic HCV genotype 1 infection. N Engl J Med. 2011;364:1195-206.
PubMed Abstract»Roebuck MC. Impact of direct-acting antiviral use for chronic hepatitis C on health care costs in Medicaid: economic model update. Am J Manag Care. 2022;28:630-1.
PubMed Abstract»Sterling RK, Kuo A, Rustgi VK, et al. Virological outcomes and treatment algorithms utilisation in observational study of patients with chronic hepatitis C treated with boceprevir or telaprevir. Aliment Pharmacol Ther. 2015;41:671-85.
PubMed Abstract»Wyles DL. Resistance to DAAs: When to Look and When It Matters. Curr HIV/AIDS Rep. 2017;14:229-237.
PubMed Abstract»Yang TH, Fang YJ, Hsu SJ, et al. Microelimination of Chronic Hepatitis C by Universal Screening Plus Direct-Acting Antivirals for Incarcerated Persons in Taiwan. Open Forum Infect Dis. 2020;7:ofaa301.
PubMed Abstract»Zelenev A, Li J, Mazhnaya A, Basu S, Altice FL. Hepatitis C virus treatment as prevention in an extended network of people who inject drugs in the USA: a modelling study. Lancet Infect Dis. 2018;18:215-24.
PubMed Abstract»Zelenev A, Li J, Shea P, Hecht R, Altice FL. Modeling Combination Hepatitis C Virus Treatment and Prevention Strategies in a Network of People Who Inject Drugs in the United States. Clin Infect Dis. 2021;72:755-63.
PubMed Abstract»Zeuzem S, Andreone P, Pol S, et al. Telaprevir for retreatment of HCV infection. N Engl J Med. 2011;364:2417-28.
PubMed Abstract»Zeuzem S, Rodríguez-Torres M, Rajender Reddy K, et al. Optimized threshold for serum HCV RNA to predict treatment outcomes in hepatitis C patients receiving peginterferon alfa-2a/ribavirin. J Viral Hepat. 2012;19:766-74.
PubMed Abstract»Zuckerman A, Chastain CA, Naggie S. Retreatment Options Following HCV Direct Acting Antiviral Failure. Curr Treat Options Infect Dis. 2017;9:389-402.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Akhtar E, Manne V, Saab S. Cirrhosis regression in hepatitis C patients with sustained virological response after antiviral therapy: a meta-analysis. Liver Int. 2014;35:30-6.
PubMed Abstract»Arase Y, Suzuki F, Suzuki Y, et al. Sustained virological response reduces incidence of onset of type 2 diabetes in chronic hepatitis C. Hepatology. 2009;49:739-44.
PubMed Abstract»Benvegnù L, Chemello L, Noventa F, Fattovich G, Pontisso P, Alberti A. Retrospective analysis of the effect of interferon therapy on the clinical outcome of patients with viral cirrhosis. Cancer. 1998;83:901-9.
PubMed Abstract»Cabibbo G, Petta S, Calvaruso V, et al. Is early recurrence of hepatocellular carcinoma in HCV cirrhotic patients affected by treatment with direct-acting antivirals? A prospective multicentre study. Aliment Pharmacol Ther. 2017;46:688-95.
PubMed Abstract»Cacoub P, Desbois AC, Comarmond C, Saadoun D. Impact of sustained virological response on the extrahepatic manifestations of chronic hepatitis C: a meta-analysis. Gut. 2018;67:2025-34.
PubMed Abstract»Calvaruso V, Cabibbo G, Cacciola I, et al. Incidence of Hepatocellular Carcinoma in Patients With HCV-Associated Cirrhosis Treated With Direct-Acting Antiviral Agents. Gastroenterology. 2018;155:411-21.e4.
PubMed Abstract»Cardoso AC, Moucari R, Figueiredo-Mendes C, et al. Impact of peginterferon and ribavirin therapy on hepatocellular carcinoma: incidence and survival in hepatitis C patients with advanced fibrosis. J Hepatol. 2010;52:652-7.
PubMed Abstract»Dohmen K, Kawano A, Takahashi K, et al. The incidence and risk factors for the development of hepatocellular carcinoma after peginterferon plus ribavirin therapy for chronic hepatitis C. Hepatogastroenterology. 2013;60:2034-8.
PubMed Abstract»Dufour JF, DeLellis R, Kaplan MM. Regression of hepatic fibrosis in hepatitis C with long-term interferon treatment. Dig Dis Sci. 1998;43:2573-6.
PubMed Abstract»El-Serag HB, Hampel H, Yeh C, Rabeneck L. Extrahepatic manifestations of hepatitis C among United States male veterans. Hepatology. 2002;36:1439-45.
PubMed Abstract»El-Sherif O, Jiang ZG, Tapper EB, et al. Baseline Factors Associated With Improvements in Decompensated Cirrhosis After Direct-Acting Antiviral Therapy for Hepatitis C Virus Infection. Gastroenterology. 2018;154:2111-2121.e8.
PubMed Abstract»Fernández-Montero JV, Aspinall EJ, Burns JE. Treatment as Prevention: Should Hepatitis C Learn the Lessons from HIV? AIDS Rev. 2017;19:212-218.
PubMed Abstract»Fraser H, Martin NK, Brummer-Korvenkontio H, et al. Model projections on the impact of HCV treatment in the prevention of HCV transmission among people who inject drugs in Europe. J Hepatol. 2018;68:402-11.
PubMed Abstract»Ioannou GN, Green PK, Berry K. HCV eradication induced by direct-acting antiviral agents reduces the risk of hepatocellular carcinoma. J Hepatol. 2017. pii: S0168-8278(17)32273-0.
PubMed Abstract»Jacobson IM, Cacoub P, Dal Maso L, Harrison SA, Younossi ZM. Manifestations of chronic hepatitis C virus infection beyond the liver. Clin Gastroenterol Hepatol. 2010;8:1017-29.
PubMed Abstract»Kanwal F, Kramer J, Asch SM, Chayanupatkul M, Cao Y, El-Serag HB. Risk of Hepatocellular Cancer in HCV Patients Treated With Direct-Acting Antiviral Agents. Gastroenterology. 2017;153:996-1005.e1.
PubMed Abstract»Konjeti VR, John BV. Interaction Between Hepatocellular Carcinoma and Hepatitis C Eradication With Direct-acting Antiviral Therapy. Curr Treat Options Gastroenterol. 2018;16:203-214.
PubMed Abstract»Mahale P, Engels EA, Li R, et al. The effect of sustained virological response on the risk of extrahepatic manifestations of hepatitis C virus infection. Gut. 2018;67:553-561.
PubMed Abstract»Martin NK, Hickman M, Hutchinson SJ, Goldberg DJ, Vickerman P. Combination interventions to prevent HCV transmission among people who inject drugs: modeling the impact of antiviral treatment, needle and syringe programs, and opiate substitution therapy. Clin Infect Dis. 2013;57 Suppl 2:S39-45.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Olafsson S, Tyrfingsson T, Runarsdottir V, et al. Treatment as Prevention for Hepatitis C (TraP Hep C) - a nationwide elimination programme in Iceland using direct-acting antiviral agents. J Intern Med. 2018;283:500-7.
PubMed Abstract»Page K, Hahn JA, Evans J, et al. Acute hepatitis C virus infection in young adult injection drug users: a prospective study of incident infection, resolution, and reinfection. J Infect Dis. 2009;200:1216-26.
PubMed Abstract»Pol S, Carnot F, Nalpas B, et al. Reversibility of hepatitis C virus-related cirrhosis. Hum Pathol. 2004;35:107-12.
PubMed Abstract»Pol S, Parlati L. Treatment of hepatitis C: the use of the new pangenotypic direct-acting antivirals in "special populations". Liver Int. 2018;38 Suppl 1:28-33.
PubMed Abstract»Poynard T, Moussalli J, Munteanu M, et al. Slow regression of liver fibrosis presumed by repeated biomarkers after virological cure in patients with chronic hepatitis C. J Hepatol. 2013;59:675-83.
PubMed Abstract»Shiratori Y, Imazeki F, Moriyama M, et al. Histologic improvement of fibrosis in patients with hepatitis C who have sustained response to interferon therapy. Ann Intern Med. 2000;132:517-24.
PubMed Abstract»Shiratori Y, Ito Y, Yokosuka O, et al. Antiviral therapy for cirrhotic hepatitis C: association with reduced hepatocellular carcinoma development and improved survival. Ann Intern Med. 2005;142:105-14.
PubMed Abstract»Singal AG, Volk ML, Jensen D, Di Bisceglie AM, Schoenfeld PS. A sustained viral response is associated with reduced liver-related morbidity and mortality in patients with hepatitis C virus. Clin Gastroenterol Hepatol. 2010;8:280-8.
PubMed Abstract»Tang L, Marcell L, Kottilil S. Systemic manifestations of hepatitis C infection. Infect Agent Cancer. 2016;11:29.
PubMed Abstract»Veldt BJ, Heathcote EJ, Wedemeyer H, et al. Sustained virologic response and clinical outcomes in patients with chronic hepatitis C and advanced fibrosis. Ann Intern Med. 2007;147:677-84.
PubMed Abstract»Waziry R, Hajarizadeh B, Grebely J, et al. Hepatocellular carcinoma risk following direct-acting antiviral HCV therapy: A systematic review, meta-analyses, and meta-regression. J Hepatol. 2017;67:1204-1212.
PubMed Abstract»Zelenev A, Li J, Mazhnaya A, Basu S, Altice FL. Hepatitis C virus treatment as prevention in an extended network of people who inject drugs in the USA: a modelling study. Lancet Infect Dis. 2018;18:215-24.
PubMed Abstract»Lesson 2. Making a Decision on When to Initiate HCV Therapy
Background
Asselah T, Kowdley KV, Zadeikis N, et al. Efficacy of Glecaprevir/Pibrentasvir for 8 or 12 Weeks in Patients With Hepatitis C Virus Genotype 2, 4, 5, or 6 Infection Without Cirrhosis. Clin Gastroenterol Hepatol. 2018;16:417-26.
PubMed Abstract»Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599-607.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Tada T, Kumada T, Toyoda H, et al. Viral eradication reduces all-cause mortality, including non-liver-related disease, in patients with progressive hepatitis C virus-related fibrosis. J Gastroenterol Hepatol. 2017;32:687-694.
PubMed Abstract»van der Meer AJ, Veldt BJ, Feld JJ, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012 ;308:2584-93.
PubMed Abstract»Veldt BJ, Heathcote EJ, Wedemeyer H, et al. Sustained virologic response and clinical outcomes in patients with chronic hepatitis C and advanced fibrosis. Ann Intern Med. 2007;147:677-84.
PubMed Abstract»Zeuzem S, Foster GR, Wang S, et al. Glecaprevir-Pibrentasvir for 8 or 12 Weeks in HCV Genotype 1 or 3 Infection. N Engl J Med. 2018;378:354-69.
PubMed Abstract»Indications for HCV Treatment
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»European Association for Study of the Liver. EASL Clinical Practice Guidelines: management of hepatitis C virus infection. J Hepatol. 2014;60:392-420.
PubMed Abstract»Hellard ME, Jenkinson R, Higgs P, et al. Modelling antiviral treatment to prevent hepatitis C infection among people who inject drugs in Victoria, Australia. Med J Aust. 2012;196:638-41.
PubMed Abstract»Henderson DK, Dembry L, Fishman NO, et al. SHEA guideline for management of healthcare workers who are infected with hepatitis B virus, hepatitis C virus, and/or human immunodeficiency virus. Infect Control Hosp Epidemiol. 2010;31:203-32.
PubMed Abstract»Marcellin F, Roux P, Protopopescu C, Duracinsky M, Spire B, Carrieri MP. Patient-reported outcomes with direct-acting antivirals for the treatment of chronic hepatitis C: current knowledge and outstanding issues. Expert Rev Gastroenterol Hepatol. 2017;11:259-268.
PubMed Abstract»Martin NK, Hickman M, Hutchinson SJ, Goldberg DJ, Vickerman P. Combination interventions to prevent HCV transmission among people who inject drugs: modeling the impact of antiviral treatment, needle and syringe programs, and opiate substitution therapy. Clin Infect Dis. 2013;57 Suppl 2:S39-45.
PubMed Abstract»Martin NK, Vickerman P, Grebely J, et al. Hepatitis C virus treatment for prevention among people who inject drugs: Modeling treatment scale-up in the age of direct-acting antivirals. Hepatology. 2013;58:1598-609.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Tada T, Kumada T, Toyoda H, et al. Viral eradication reduces all-cause mortality, including non-liver-related disease, in patients with progressive hepatitis C virus-related fibrosis. J Gastroenterol Hepatol. 2017;32:687-694.
PubMed Abstract»Thomas DL, Villano SA, Riester KA, et al. Perinatal transmission of hepatitis C virus from human immunodeficiency virus type 1-infected mothers. Women and Infants Transmission Study. J Infect Dis. 1998;177:1480-8.
PubMed Abstract»van der Meer AJ, Veldt BJ, Feld JJ, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012 ;308:2584-93.
PubMed Abstract»Veldt BJ, Heathcote EJ, Wedemeyer H, et al. Sustained virologic response and clinical outcomes in patients with chronic hepatitis C and advanced fibrosis. Ann Intern Med. 2007;147:677-84.
PubMed Abstract»Contraindications for Treatment
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Beer L, Inglis S, Malaguti A, et al. Randomized clinical trial: Direct-acting antivirals as treatment for hepatitis C in people who inject drugs: Delivered in needle and syringe programs via directly observed therapy versus fortnightly collection. J Viral Hepat. 2022;29:646-53.
PubMed Abstract»Bini EJ, Bräu N, Currie S, et al. Prospective multicenter study of eligibility for antiviral therapy among 4,084 U.S. veterans with chronic hepatitis C virus infection. Am J Gastroenterol. 2005;100:1772-9.
PubMed Abstract»Butt AA, Wagener M, Shakil AO, Ahmad J. Reasons for non-treatment of hepatitis C in veterans in care. J Viral Hepat. 2005;12:81-5.
PubMed Abstract»Cacoub P, Desbois AC, Isnard-Bagnis C, Rocatello D, Ferri C. Hepatitis C virus infection and chronic kidney disease: Time for reappraisal. J Hepatol. 2016;65:S82-S94.
PubMed Abstract»Charlton M, Everson GT, Flamm SL, et al. Ledipasvir and sofosbuvir plus ribavirin for treatment of HCV infection in patients with advanced liver disease. Gastroenterology. 2015;149:649-59.
PubMed Abstract»Dore GJ, Altice F, Litwin AH, et al. Elbasvir-Grazoprevir to Treat Hepatitis C Virus Infection in Persons Receiving Opioid Agonist Therapy: A Randomized Trial. Ann Intern Med. 2016;165:625-634.
PubMed Abstract»Feld JJ, Jacobson IM, Sulkowski MS, Poordad F, Tatsch F, Pawlotsky JM. Ribavirin revisited in the era of direct-acting antiviral therapy for hepatitis C virus infection. Liver Int. 2017;37:5-18.
PubMed Abstract»Ferm VH, Willhite C, Kilham L. Teratogenic effects of ribavirin on hamster and rat embryos. Teratology. 1978;17:93-101.
PubMed Abstract»Gane E, Lawitz E, Pugatch D, et al. Glecaprevir and Pibrentasvir in Patients with HCV and Severe Renal Impairment. N Engl J Med. 2017;377:1448-55.
PubMed Abstract»Grebely J, Dalgard O, Conway B, et al. Sofosbuvir and velpatasvir for hepatitis C virus infection in people with recent injection drug use (SIMPLIFY): an open-label, single-arm, phase 4, multicentre trial. Lancet Gastroenterol Hepatol. 2018;3:153-61.
PubMed Abstract»Grebely J, Dore GJ, Zeuzem S, et al. Efficacy and Safety of Sofosbuvir/Velpatasvir in Patients With Chronic Hepatitis C Virus Infection Receiving Opioid Substitution Therapy: Analysis of Phase 3 ASTRAL Trials. Clin Infect Dis. 2016;63:1479-1481.
PubMed Abstract»Grebely J, Hajarizadeh B, Dore GJ. Direct-acting antiviral agents for HCV infection affecting people who inject drugs. Nat Rev Gastroenterol Hepatol. 2017;14:641-651.
PubMed Abstract»Grebely J, Oser M, Taylor LE, Dore GJ. Breaking down the barriers to hepatitis C virus (HCV) treatment among individuals with HCV/HIV coinfection: action required at the system, provider, and patient levels. J Infect Dis. 2013;207 Suppl 1:S19-25.
PubMed Abstract»Litwin AH, Lum PJ, Taylor LE, et al. Patient-centred models of hepatitis C treatment for people who inject drugs: a multicentre, pragmatic randomised trial. Lancet Gastroenterol Hepatol. 2022;7:1112-27.
PubMed Abstract»Meyer JP, Moghimi Y, Marcus R, Lim JK, Litwin AH, Altice FL. Evidence-based interventions to enhance assessment, treatment, and adherence in the chronic Hepatitis C care continuum. Int J Drug Policy. 2015;26:922-35.
PubMed Abstract»Roberts SS, Miller RK, Jones JK, et al. The Ribavirin Pregnancy Registry: Findings after 5 years of enrollment, 2003-2009. Birth Defects Res A Clin Mol Teratol. 2010;88:551-9.
PubMed Abstract»Talal AH, LaFleur J, Hoop R, et al. Absolute and relative contraindications to pegylated-interferon or ribavirin in the US general patient population with chronic hepatitis C: results from a US database of over 45 000 HCV-infected, evaluated patients. Aliment Pharmacol Ther. 2013;37:473-81.
PubMed Abstract»Ward RP, Kugelmas M. Using pegylated interferon and ribavirin to treat patients with chronic hepatitis C. Am Fam Physician. 2005;72:655-62.
PubMed Abstract»Timing of Initiation of Treatment
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Asselah T, Marcellin P. Interferon free therapy with direct acting antivirals for HCV. Liver Int. 2013;33 Suppl 1:93-104.
PubMed Abstract»Butt AA, Yan P. Natural history of hepatitis C virus infection in a large national seroconversion cohort in the direct-acting antiviral agent era: Results from ERCHIVES. J Viral Hepat. 2021 Mar 24. Online ahead of print.
PubMed Abstract»Hepatitis C. State of Medicaid Access. Center for Health Law and Policy Innovation of Harvard Law School (CHLPI) and the National Viral Hepatitis Roundtable (NVHR).
CHLPI and NVHR»Jacobson IM, Gordon SC, Kowdley KV, et al. Sofosbuvir for hepatitis C genotype 2 or 3 in patients without treatment options. N Engl J Med. 2013;368:1867-77.
PubMed Abstract»Jeźequel C, Bardou-Jacquet E, Desille Y, Renard I, Lainé F, Lelan C, et al. Survival of patients infected by chronic hepatitis C and F0F1 fibrosis at baseline after a 15 years follow-up. J Hepatol. 2015;62:S589.
EASL»Poordad F, Lawitz E, Kowdley KV, et al. Exploratory study of oral combination antiviral therapy for hepatitis C. N Engl J Med. 2013 Jan 3;368:45-53.
PubMed Abstract»Sahakyan Y, Lee-Kim V, Bremner KE, Bielecki JM, Krahn MD. Impact of direct-acting antiviral regimens on mortality and morbidity outcomes in patients with chronic hepatitis c: Systematic review and meta-analysis. J Viral Hepat. 2021 Feb 8. Online ahead of print.
PubMed Abstract»Zahnd C, Salazar-Vizcaya L, Dufour JF, et al. Modelling the impact of deferring HCV treatment on liver-related complications in HIV coinfected men who have sex with men. J Hepatol. 2016;65:26-32.
PubMed Abstract»Monitoring and Follow-Up if Not Treated
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Afdhal NH. Fibroscan (transient elastography) for the measurement of liver fibrosis. Gastroenterol Hepatol (N Y). 2012;8:605-7.
PubMed Abstract»Benhamou Y, Bochet M, Di Martino V, et al. Liver fibrosis progression in human immunodeficiency virus and hepatitis C virus coinfected patients. The Multivirc Group. Hepatology. 1999;30:1054-8.
PubMed Abstract»Butt AA, Wagener M, Shakil AO, Ahmad J. Reasons for non-treatment of hepatitis C in veterans in care. J Viral Hepat. 2005;12:81-5.
PubMed Abstract»Fartoux L, Chazouillères O, Wendum D, Poupon R, Serfaty L. Impact of steatosis on progression of fibrosis in patients with mild hepatitis C. Hepatology. 2005;41:82-7.
PubMed Abstract»Graham CS, Baden LR, Yu E, Mrus JM, Carnie J, Heeren T, Koziel MJ. Influence of human immunodeficiency virus infection on the course of hepatitis C virus infection: a meta-analysis. Clin Infect Dis. 2001;33:562-9.
PubMed Abstract»Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. Am Fam Physician.2006;74:756-62.
PubMed Abstract»Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-80.
PubMed Abstract»Lin ZH, Xin YN, Dong QJ, et al. Performance of the aspartate aminotransferase-to-platelet ratio index for the staging of hepatitis C-related fibrosis: an updated meta-analysis. Hepatology. 2011;53:726-36.
PubMed Abstract»Lingala S, Ghany MG. Natural History of Hepatitis C. Gastroenterol Clin North Am. 2015;44:717-34.
PubMed Abstract»Maasoumy B, Wedemeyer H. Natural history of acute and chronic hepatitis C. Best Pract Res Clin Gastroenterol. 2012;26:401-12.
PubMed Abstract»Missiha SB, Ostrowski M, Heathcote EJ. Disease progression in chronic hepatitis C: modifiable and nonmodifiable factors. Gastroenterology. 2008;134;1699-714.
PubMed Abstract»Poynard T, Morra R, Halfon P, et al. Meta-analyses of FibroTest diagnostic value in chronic liver disease. BMC Gastroenterol. 2007;7:40.
PubMed Abstract»Poynard T, Ratziu V, Charlotte F, Goodman Z, McHutchison J, Albrecht J. Rates and risk factors of liver fibrosis progression in patients with chronic hepatitis C. J Hepatol. 2001;34:730-9.
PubMed Abstract»Singal AG, Llovet JM, Yarchoan M, et al. AASLD Practice Guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology. 2023;78:1922-65.
AASLD»Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012;307:832-42.
PubMed Abstract»Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, Lok AS. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38:518-26.
PubMed Abstract»Wiley TE, McCarthy M, Breidi L, McCarthy M, Layden TJ. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology. 1998;28:805-9.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with decompensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Afdhal N, Everson GT, Calleja JL, et al. Effect of viral suppression on hepatic venous pressure gradient in hepatitis C with cirrhosis and portal hypertension. J Viral Hepat. 2017;24:823-831.
PubMed Abstract»Afdhal N, Reddy KR, Nelson DR, et al. Ledipasvir and sofosbuvir for previously treated HCV genotype 1 infection. N Engl J Med. 2014;370:1483-93.
PubMed Abstract»Afdhal N, Zeuzem S, Kwo P, et al. Ledipasvir and sofosbuvir for untreated HCV genotype 1 infection. N Engl J Med. 2014;370:1889-98.
PubMed Abstract»Afdhal NH. Fibroscan (transient elastography) for the measurement of liver fibrosis. Gastroenterol Hepatol (N Y). 2012;8:605-7.
PubMed Abstract»Asselah T, Kowdley KV, Zadeikis N, et al. Efficacy of Glecaprevir/Pibrentasvir for 8 or 12 Weeks in Patients With Hepatitis C Virus Genotype 2, 4, 5, or 6 Infection Without Cirrhosis. Clin Gastroenterol Hepatol. 2018;16:417-26.
PubMed Abstract»Bourlière M, Bronowicki JP, de Ledinghen V, et al. Ledipasvir-sofosbuvir with or without ribavirin to treat patients with HCV genotype 1 infection and cirrhosis non-responsive to previous protease-inhibitor therapy: a randomised, double-blind, phase 2 trial (SIRIUS). Lancet Infect Dis. 2015;15:397-404.
PubMed Abstract»Bruno S, Shiffman ML, Roberts SK, Gane EJ, Messinger D, Hadziyannis SJ, Marcellin P. Efficacy and safety of peginterferon alfa-2a (40KD) plus ribavirin in hepatitis C patients with advanced fibrosis and cirrhosis. Hepatology. 2010;51:388-97.
PubMed Abstract»Buti M, Agarwal K, Horsmans Y, et al. Telaprevir twice daily is noninferior to telaprevir every 8 hrs for patients with chronic hepatitis C. Gastroenterology. 2014;146:744-53.
PubMed Abstract»Chappell CA, Scarsi KK, Kirby BJ, et al. Ledipasvir plus sofosbuvir in pregnant women with hepatitis C virus infection: a phase 1 pharmacokinetic study. Lancet Microbe. 2020;1:e200-e208.
PubMed Abstract»Charlton M, Everson GT, Flamm SL, et al. Ledipasvir and sofosbuvir plus ribavirin for treatment of HCV infection in patients with advanced liver disease. Gastroenterology. 2015;149:649-59.
PubMed Abstract»Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599-607.
PubMed Abstract»Fried MW, Shiffman ML, Reddy KR, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med. 2002;347:975-82.
PubMed Abstract»Graham CS, Baden LR, Yu E, Mrus JM, Carnie J, Heeren T, Koziel MJ. Influence of human immunodeficiency virus infection on the course of hepatitis C virus infection: a meta-analysis. Clin Infect Dis. 2001;33:562-9.
PubMed Abstract»Hézode C, Fontaine H, Dorival C, et al. Effectiveness of telaprevir or boceprevir in treatment-experienced patients with HCV genotype 1 infection and cirrhosis. Gastroenterology. 2014;147:132-142.e4.
PubMed Abstract»Hézode C, Fontaine H, Dorival C, et al. Triple therapy in treatment-experienced patients with HCV-cirrhosis in a multicentre cohort of the French Early Access Programme (ANRS CO20-CUPIC) - NCT01514890. J Hepatol. 2013;59:434-41.
PubMed Abstract»Hadziyannis SJ, Sette H Jr, Morgan TR, et al. Peginterferon-alfa2a and ribavirin combination therapy in chronic hepatitis C: a randomized study of treatment duration and ribavirin dose. Ann Intern Med. 2004;140:346–55.
PubMed Abstract»Heathcote EJ, Shiffman ML, Cooksley WG, et al. Peginterferon alfa-2a in patients with chronic hepatitis C and cirrhosis. N Engl J Med. 2000;343:1673-80.
PubMed Abstract»Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. Am Fam Physician.2006;74:756-62.
PubMed Abstract»Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-80.
PubMed Abstract»Helbling B, Jochum W, Stamenic I, et al. HCV-related advanced fibrosis/cirrhosis: randomized controlled trial of pegylated interferon alpha-2a and ribavirin. J Viral Hepat. 2006;13:762-9.
PubMed Abstract»Jacobson IM, McHutchison JG, Dusheiko G, et al. Telaprevir for previously untreated chronic hepatitis C virus infection. N Engl J Med. 2011;364:2405-16.
PubMed Abstract»Lawitz E, Poordad F, Brainard DM, et al. Sofosbuvir with peginterferon-ribavirin for 12 weeks in previously treated patients with hepatitis C genotype 2 or 3 and cirrhosis. Hepatology. 2015;61:769-75.
PubMed Abstract»Lawitz E, Sulkowski MS, Ghalib R, et al. Simeprevir plus sofosbuvir, with or without ribavirin, to treat chronic infection with hepatitis C virus genotype 1 in non-responders to pegylated interferon and ribavirin and treatment-naive patients: the COSMOS randomised study. Lancet. 2014;384:1756-65.
PubMed Abstract»Lin ZH, Xin YN, Dong QJ, et al. Performance of the aspartate aminotransferase-to-platelet ratio index for the staging of hepatitis C-related fibrosis: an updated meta-analysis. Hepatology. 2011;53:726-36.
PubMed Abstract»Lingala S, Ghany MG. Natural History of Hepatitis C. Gastroenterol Clin North Am. 2015;44:717-34.
PubMed Abstract»Maasoumy B, Wedemeyer H. Natural history of acute and chronic hepatitis C. Best Pract Res Clin Gastroenterol. 2012;26:401-12.
PubMed Abstract»Manns MP, McHutchison JG, Gordon SC, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet. 2001;358:958-65.
PubMed Abstract»Marcellin F, Roux P, Protopopescu C, Duracinsky M, Spire B, Carrieri MP. Patient-reported outcomes with direct-acting antivirals for the treatment of chronic hepatitis C: current knowledge and outstanding issues. Expert Rev Gastroenterol Hepatol. 2017;11:259-268.
PubMed Abstract»Martin NK, Hickman M, Hutchinson SJ, Goldberg DJ, Vickerman P. Combination interventions to prevent HCV transmission among people who inject drugs: modeling the impact of antiviral treatment, needle and syringe programs, and opiate substitution therapy. Clin Infect Dis. 2013;57 Suppl 2:S39-45.
PubMed Abstract»McHutchison JG, Everson GT, Gordon SC, et al. Telaprevir with peginterferon and ribavirin for chronic HCV genotype 1 infection. N Engl J Med. 2009;360:1827-38.
PubMed Abstract»Missiha SB, Ostrowski M, Heathcote EJ. Disease progression in chronic hepatitis C: modifiable and nonmodifiable factors. Gastroenterology. 2008;134;1699-714.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Muir AJ, Poordad F, Lalezari J, et al. Daclatasvir in combination with asunaprevir and beclabuvir for hepatitis C virus genotype 1 infection with compensated cirrhosis. JAMA. 2015;313:1736-44.
PubMed Abstract»Poordad F, Hezode C, Trinh R, et al. ABT-450/r-ombitasvir and dasabuvir with ribavirin for hepatitis C with cirrhosis. N Engl J Med. 2014;370:1973-82.
PubMed Abstract»Poordad F, McCone J Jr, Bacon BR, et al. Boceprevir for untreated chronic HCV genotype 1 infection. N Engl J Med. 2011;364:1195-206.
PubMed Abstract»Poynard T, Bedossa P, Opolon P. Lancet. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825-32.
PubMed Abstract»Poynard T, Morra R, Halfon P, et al. Meta-analyses of FibroTest diagnostic value in chronic liver disease. BMC Gastroenterol. 2007;7:40.
PubMed Abstract»Poynard T, Ratziu V, Charlotte F, Goodman Z, McHutchison J, Albrecht J. Rates and risk factors of liver fibrosis progression in patients with chronic hepatitis C. J Hepatol. 2001;34:730-9.
PubMed Abstract»Schmid P, Bregenzer A, Huber M, et al. Progression of Liver Fibrosis in HIV/HCV Co-Infection: A Comparison between Non-Invasive Assessment Methods and Liver Biopsy. PLoS One. 2015;10:e0138838.
PubMed Abstract»Singal AG, Llovet JM, Yarchoan M, et al. AASLD Practice Guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology. 2023;78:1922-65.
AASLD»Tada T, Kumada T, Toyoda H, et al. Viral eradication reduces all-cause mortality, including non-liver-related disease, in patients with progressive hepatitis C virus-related fibrosis. J Gastroenterol Hepatol. 2017;32:687-694.
PubMed Abstract»Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012;307:832-42.
PubMed Abstract»van der Meer AJ, Veldt BJ, Feld JJ, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012 ;308:2584-93.
PubMed Abstract»Veldt BJ, Heathcote EJ, Wedemeyer H, et al. Sustained virologic response and clinical outcomes in patients with chronic hepatitis C and advanced fibrosis. Ann Intern Med. 2007;147:677-84.
PubMed Abstract»Vierling JM, Zeuzem S, Poordad F, et al. Safety and efficacy of boceprevir/peginterferon/ribavirin for HCV G1 compensated cirrhotics: Meta-analysis of 5 trials. J Hepatol. 2014;61:200-9.
PubMed Abstract»Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, Lok AS. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38:518-26.
PubMed Abstract»Wiley TE, McCarthy M, Breidi L, McCarthy M, Layden TJ. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology. 1998;28:805-9.
PubMed Abstract»Yattoo GN, Shafi SM, Dar GA, et al. Safety and efficacy of treatment for chronic hepatitis C during pregnancy: A prospective observational study in Srinagar, India. Clin Liver Dis (Hoboken). 2023;22:134-9.
PubMed Abstract»Zeuzem S, Dusheiko GM, Salupere R, et al. Sofosbuvir and ribavirin in HCV genotypes 2 and 3. N Engl J Med. 2014;370:1993-2001.
PubMed Abstract»Lesson 3. Addressing Barriers to HCV Treatment
Background
Braun DL, Hampel B, Ledergerber B, et al. A Treatment-as-Prevention Trial to Eliminate Hepatitis C Among Men Who Have Sex With Men Living With Human Immunodeficiency Virus (HIV) in the Swiss HIV Cohort Study. Clin Infect Dis. 2021;73:e2194-e2202.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). 2019 Viral Hepatitis Surveillance Report—Hepatitis C. Published May 2021.
CDC»Centers for Disease Control and Prevention (CDC). Division of Viral Hepatitis 2025 Strategic Plan, CDC; 2020. 1-22.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2022. Published April 2024.
CDC»Falade-Nwulia O, Suarez-Cuervo C, Nelson DR, Fried MW, Segal JB, Sulkowski MS. Oral Direct-Acting Agent Therapy for Hepatitis C Virus Infection: A Systematic Review. Ann Intern Med. 2017;166:637-48.
PubMed Abstract»Hofmeister MG, Rosenthal EM, Barker LK, et al. Estimating Prevalence of Hepatitis C Virus Infection in the United States, 2013-2016. Hepatology. 2019;69:1020-31.
PubMed Abstract»Iversen J, Dore GJ, Catlett B, Cunningham P, Grebely J, Maher L. Association between rapid utilisation of direct hepatitis C antivirals and decline in the prevalence of viremia among people who inject drugs in Australia. J Hepatol. 2019;70:33-9.
PubMed Abstract»Martin NK, Vickerman P, Grebely J, et al. Hepatitis C virus treatment for prevention among people who inject drugs: Modeling treatment scale-up in the age of direct-acting antivirals. Hepatology. 2013;58:1598-609.
PubMed Abstract»Zibbell JE, Asher AK, Patel RC, et al. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am J Public Health. 2018;108:175-181.
PubMed Abstract»Zibbell JE, Hart-Malloy R, Barry J, Fan L, Flanigan C. Risk factors for HCV infection among young adults in rural New York who inject prescription opioid analgesics. Am J Public Health. 2014;104:2226-32.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»The Path to HCV Cure: HCV Care Continuum
Chhatwal J, Chen Q, Bethea ED, Hur C, Spaulding AC, Kanwal F. The impact of direct-acting anti-virals on the hepatitis C care cascade: identifying progress and gaps towards hepatitis C elimination in the United States. Aliment Pharmacol Ther. 2019;50:66-74.
PubMed Abstract»Hill A, Khoo S, Fortunak J, Simmons B, Ford N. Minimum costs for producing hepatitis C direct-acting antivirals for use in large-scale treatment access programs in developing countries. Clin Infect Dis. 2014;58:928-36.
PubMed Abstract»Iyengar S, Tay-Teo K, Vogler S, et al. Prices, Costs, and Affordability of New Medicines for Hepatitis C in 30 Countries: An Economic Analysis. PLoS Med. 2016;13:e1002032.
PubMed Abstract»Rosenthal ES, Graham CS. Price and affordability of direct-acting antiviral regimens for hepatitis C virus in the United States. Infect Agent Cancer. 2016;11:24.
PubMed Abstract»Saag MS. Editorial commentary: getting smart in how we pay for HCV drugs: KAOS vs CONTROL. Clin Infect Dis. 2015 Mar 16;61:169-70.
PubMed Abstract»Safreed-Harmon K, Blach S, Aleman S, et al. The Consensus Hepatitis C Cascade of Care: Standardized Reporting to Monitor Progress Toward Elimination. Clin Infect Dis. 2019;69:2218-27.
PubMed Abstract»Trooskin SB, Reynolds H, Kostman JR. Access to Costly New Hepatitis C Drugs: Medicine, Money, and Advocacy. Clin Infect Dis. 2015;61:1825-30.
PubMed Abstract»Yehia BR, Schranz AJ, Umscheid CA, Lo Re V 3rd. The treatment cascade for chronic hepatitis C virus infection in the United States: a systematic review and meta-analysis. PLoS One. 2014;9:e101554.
PubMed Abstract»Zhou K, Fitzpatrick T, Walsh N, et al. Interventions to optimise the care continuum for chronic viral hepatitis: a systematic review and meta-analyses. Lancet Infect Dis. 2016;16:1409-22.
PubMed Abstract»Zou B, Yeo YH, Le MH, et al. Prevalence of Viremic Hepatitis C Virus Infection by Age, Race/Ethnicity, and Birthplace and Disease Awareness Among Viremic Persons in the United States, 1999-2016. J Infect Dis. 2020;221:408-18.
PubMed Abstract»HCV Testing: Access, Efficiency, and Reimbursement
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Burrell CN, Sharon MJ, Davis S, et al. Using the electronic medical record to increase testing for HIV and hepatitis C virus in an Appalachian emergency department. BMC Health Serv Res. 2021;21:524.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Division of Viral Hepatitis 2025 Strategic Plan, CDC; 2020. 1-22.
CDC»Chou R, Dana T, Fu R, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2020;323:1318.
PubMed Abstract»Coyle C, Kwakwa H, Viner K. Integrating Routine HCV Testing in Primary Care: Lessons Learned from Five Federally Qualified Health Centers in Philadelphia, Pennsylvania, 2012-2014. Public Health Rep. 2016;131 Suppl 2:65-73.
PubMed Abstract»Coyle C, Kwakwa H. Dual-Routine HCV/HIV Testing: Seroprevalence and Linkage to Care in Four Community Health Centers in Philadelphia, Pennsylvania. Public Health Rep. 2016;131 Suppl 1:41-52.
PubMed Abstract»Denkinger CM, Kessel M. Diagnostics for hepatitis C: an urgent need for action. Lancet Glob Health. 2015;3:e195.
PubMed Abstract»Falade-Nwulia O, Mehta S, Sulkowski M, Lasola J, Ghanem K, Chaulk P, Thomas D. Impact of Rapid hepatitis C testing on receipt of hepatitis C results in a public STD clinic. Program and abstracts of the 21st Conference on Retroviruses and Opportunistic Infections; March 3-6, 2014; Boston, Massachusetts. Abstract Number 631.
CROI»Fleurence RL, Collins FS. A National Hepatitis C Elimination Program in the United States: A Historic Opportunity. JAMA. 2023;329:1251-2.
PubMed Abstract»Frimpong JA, Shiu-Yee K, Tross S, et al. Bundling Rapid Human Immunodeficiency Virus and Hepatitis C Virus Testing to Increase Receipt of Test Results: A Randomized Trial. Med Care. 2020;58:445-52.
PubMed Abstract»Geboy AG, Nichols WL, Fernandez SJ, Desale S, Basch P, Fishbein DA. Leveraging the electronic health record to eliminate hepatitis C: Screening in a large integrated healthcare system. PLoS One. 2019;14:e0216459.
PubMed Abstract»Hack B, Sanghavi K, Gundapaneni S, et al. HCV universal EHR prompt successfully increases screening, highlights potential disparities. PLoS One. 2023;18:e0279972.
PubMed Abstract»Mehta SJ, Torgersen J, Small DS, et al. Effect of a Default Order vs an Alert in the Electronic Health Record on Hepatitis C Virus Screening Among Hospitalized Patients: A Stepped-Wedge Randomized Clinical Trial. JAMA Netw Open. 2022;5:e222427.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Improving Services for Linkage-to-Care
Falade-Nwulia O, Gicquelais RE, Astemborski J, et al. Hepatitis C treatment uptake among people who inject drugs in the oral direct-acting antiviral era. Liver Int. 2020;40:2407-16.
PubMed Abstract»Falade-Nwulia O, Mehta SH, Lasola J, et al. Public health clinic-based hepatitis C testing and linkage to care in Baltimore. J Viral Hepat. 2016;23:366-74.
PubMed Abstract»Henderson C, Madden A, Kelsall J. 'Beyond the willing & the waiting' - The role of peer-based approaches in hepatitis C diagnosis & treatment. Int J Drug Policy. 2017;50:111-5.
PubMed Abstract»Hofmeister MG, Rosenthal EM, Barker LK, et al. Estimating Prevalence of Hepatitis C Virus Infection in the United States, 2013-2016. Hepatology. 2019;69:1020-31.
PubMed Abstract»Hunt BR, Ahmed C, Ramirez-Mercado K, Patron C, Glick NR. Routine Screening and Linkage to Care for Hepatitis C Virus in an Urban Safety-Net Health System, 2017-2019. Public Health Rep. 2021;136:219-27.
PubMed Abstract»Jordan AE, Cleland CM, Schackman BR, Wyka K, Perlman DC, Nash D. Hepatitis C Virus (HCV) Care Continuum Outcomes and HCV Community Viral Loads Among Patients in an Opioid Treatment Program. J Infect Dis. 2020;222:S335-S345.
PubMed Abstract»Jordan AE, Perlman DC, Reed J, Smith DJ, Hagan H. Patterns and Gaps Identified in a Systematic Review of the Hepatitis C Virus Care Continuum in Studies among People Who Use Drugs. Front Public Health. 2017;5:348.
PubMed Abstract»Litwin AH, Drolet M, Nwankwo C, et al. Perceived barriers related to testing, management and treatment of HCV infection among physicians prescribing opioid agonist therapy: The C-SCOPE Study. J Viral Hepat. 2019;26:1094-1104.
PubMed Abstract»Litwin AH, Lum PJ, Taylor LE, et al. Patient-centred models of hepatitis C treatment for people who inject drugs: a multicentre, pragmatic randomised trial. Lancet Gastroenterol Hepatol. 2022;7:1112-27.
PubMed Abstract»Norton BL, Bachhuber MA, Singh R, et al. Evaluation of contingency management as a strategy to improve HCV linkage to care and treatment in persons attending needle and syringe programs: A pilot study. Int J Drug Policy. 2019;69:1-7.
PubMed Abstract»Sherbuk JE, McManus KA, Kemp Knick T, Canan CE, Flickinger T, Dillingham R. Disparities in Hepatitis C Linkage to Care in the Direct Acting Antiviral Era: Findings From a Referral Clinic With an Embedded Nurse Navigator Model. Front Public Health. 2019;7:362.
PubMed Abstract»Stagg HR, Surey J, Francis M, et al. Improving engagement with healthcare in hepatitis C: a randomised controlled trial of a peer support intervention. BMC Med. 2019;17:71.
PubMed Abstract»Strebe J, Rich NE, Wang L, et al. Patient Navigation Increases Linkage to Care and Receipt of Direct-acting Antiviral Therapy in Patients with Hepatitis C. Clin Gastroenterol Hepatol. 2023;21:988-94.e2.
PubMed Abstract»Zhou K, Fitzpatrick T, Walsh N, et al. Interventions to optimise the care continuum for chronic viral hepatitis: a systematic review and meta-analyses. Lancet Infect Dis. 2016;16:1409-22.
PubMed Abstract»Expanding Medical Provider Capacity
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Overview of cost, reimbursement, and cost-effectiveness considerations for hepatitis C treatment regimens.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364:2199-207.
PubMed Abstract»Beste LA, Glorioso TJ, Ho PM, et al. Telemedicine Specialty Support Promotes Hepatitis C Treatment by Primary Care Providers in the Department of Veterans Affairs. Am J Med. 2017;130:432-438.e3.
PubMed Abstract»Facente SN, Burk K, Eagen K, Mara ES, Smith AA, Lynch CS. New Treatments Have Changed the Game: Hepatitis C Treatment in Primary Care. Infect Dis Clin North Am. 2018;32:313-22.
PubMed Abstract»Irvin R, Ntiri-Reid B, Kleinman M, et al. Sharing the cure: Building primary care and public health infrastructure to improve the hepatitis C care continuum in Maryland. J Viral Hepat. 2020;27:1388-95.
PubMed Abstract»Kattakuzhy S, Gross C, Emmanuel B, et al. Expansion of Treatment for Hepatitis C Virus Infection by Task Shifting to Community-Based Nonspecialist Providers: A Nonrandomized Clinical Trial. Ann Intern Med. 2017;167:311-318.
PubMed Abstract»Overton K, Clegg J, Pekin F, et al. Outcomes of a nurse-led model of care for hepatitis C assessment and treatment with direct-acting antivirals in the custodial setting. Int J Drug Policy. 2019;72:123-8.
PubMed Abstract»Radley A, de Bruin M, Inglis SK, et al. Clinical effectiveness of pharmacist-led versus conventionally delivered antiviral treatment for hepatitis C virus in patients receiving opioid substitution therapy: a pragmatic, cluster-randomised trial. Lancet Gastroenterol Hepatol. 2020;5:809-18.
PubMed Abstract»Scott JD, Unruh KT, Catlin MC, et al. Project ECHO: a model for complex, chronic care in the Pacific Northwest region of the United States. J Telemed Telecare. 2012;18:481-4.
PubMed Abstract»Expanding Settings for HCV Clinical Care and Treatment
Taylor JL, Johnson S, Cruz R, Gray JR, Schiff D, Bagley SM. Integrating Harm Reduction into Outpatient Opioid Use Disorder Treatment Settings : Harm Reduction in Outpatient Addiction Treatment. J Gen Intern Med. 2021;36:3810-19.
PubMed Abstract»Insurance and Medicaid Restrictions to HCV Treatment Access
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Canary LA, Klevens RM, Holmberg SD. Limited Access to New Hepatitis C Virus Treatment Under State Medicaid Programs. Ann Intern Med. 2015;163:226-8.
PubMed Abstract»Dore GJ, Altice F, Litwin AH, et al. Elbasvir-Grazoprevir to Treat Hepatitis C Virus Infection in Persons Receiving Opioid Agonist Therapy: A Randomized Trial. Ann Intern Med. 2016;165:625-634.
PubMed Abstract»Gowda C, Lott S, Grigorian M, et al. Absolute Insurer Denial of Direct-Acting Antiviral Therapy for Hepatitis C: A National Specialty Pharmacy Cohort Study. Open Forum Infect Dis. 2018;5:ofy076.
PubMed Abstract»Grebely J, Dalgard O, Conway B, et al. Sofosbuvir and velpatasvir for hepatitis C virus infection in people with recent injection drug use (SIMPLIFY): an open-label, single-arm, phase 4, multicentre trial. Lancet Gastroenterol Hepatol. 2018;3:153-61.
PubMed Abstract»Iversen J, Dore GJ, Catlett B, Cunningham P, Grebely J, Maher L. Association between rapid utilisation of direct hepatitis C antivirals and decline in the prevalence of viremia among people who inject drugs in Australia. J Hepatol. 2019;70:33-9.
PubMed Abstract»Javanbakht M, Archer R, Klausner J. Will prior health insurance authorization for medications continue to hinder hepatitis C treatment delivery in the United States? Perspectives from hepatitis C treatment providers in a large urban healthcare system. PLoS One. 2020;15:e0241615.
PubMed Abstract»Lo Re V 3rd, Gowda C, Urick PN, et al. Disparities in Absolute Denial of Modern Hepatitis C Therapy by Type of Insurance. Clin Gastroenterol Hepatol. 2016;14:1035-43.
PubMed Abstract»Martin NK, Vickerman P, Dore GJ, Hickman M. The hepatitis C virus epidemics in key populations (including people who inject drugs, prisoners and MSM): the use of direct-acting antivirals as treatment for prevention. Curr Opin HIV AIDS. 2015;10:374-80.
PubMed Abstract»Martin NK, Vickerman P, Grebely J, et al. Hepatitis C virus treatment for prevention among people who inject drugs: Modeling treatment scale-up in the age of direct-acting antivirals. Hepatology. 2013;58:1598-609.
PubMed Abstract»Rosecrans AM, Cheedalla A, Rives ST, et al. Public Health Clinic-Based Hepatitis C Treatment. Am J Prev Med. 2020;59:420-7.
PubMed Abstract»Saeed S, Strumpf E, Moodie EEM, et al. Eliminating Structural Barriers: The Impact of Unrestricted Access on Hepatitis C Treatment Uptake Among People Living With Human Immunodeficiency Virus. Clin Infect Dis. 2020;71:363-71.
PubMed Abstract»Sood N, Ung D, Shankar A, Strom BL. A Novel Strategy for Increasing Access to Treatment for Hepatitis C Virus Infection for Medicaid Beneficiaries. Ann Intern Med. 2018;169:118-9.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with decompensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Afdhal N, Everson GT, Calleja JL, et al. Effect of viral suppression on hepatic venous pressure gradient in hepatitis C with cirrhosis and portal hypertension. J Viral Hepat. 2017;24:823-831.
PubMed Abstract»Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364:2199-207.
PubMed Abstract»Barua S, Greenwald R, Grebely J, Dore GJ, Swan T, Taylor LE. Restrictions for medicaid reimbursement of sofosbuvir for the treatment of hepatitis C virus infection in the United States. Ann Intern Med. 2015;163:215-23.
PubMed Abstract»Buti M, Domínguez-Hernández R, Oyagüez I, Casado MA, Esteban R. Cost-effectiveness analysis of ledipasvir/sofosbuvir in patients with chronic hepatitis C: Treatment of patients with absence or mild fibrosis compared to patients with advanced fibrosis. J Viral Hepat. 2017;24:750-758.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). 2019 Viral Hepatitis Surveillance Report—Hepatitis C. Published May 2021.
CDC»Chahal HS, Marseille EA, Tice JA, et al. Cost-effectiveness of Early Treatment of Hepatitis C Virus Genotype 1 by Stage of Liver Fibrosis in a US Treatment-Naive Population. JAMA Intern Med. 2016;176:65-73.
PubMed Abstract»Charlton M, Everson GT, Flamm SL, et al. Ledipasvir and sofosbuvir plus ribavirin for treatment of HCV infection in patients with advanced liver disease. Gastroenterology. 2015;149:649-59.
PubMed Abstract»Chhatwal J, He T, Hur C, Lopez-Olivo MA. Direct-Acting Antiviral Agents for Patients With Hepatitis C Virus Genotype 1 Infection Are Cost-Saving. Clin Gastroenterol Hepatol. 2017;15:827-837.e8.
PubMed Abstract»Chhatwal J, He T, Lopez-Olivo MA. Systematic Review of Modelling Approaches for the Cost Effectiveness of Hepatitis C Treatment with Direct-Acting Antivirals. Pharmacoeconomics. 2016;34:551-67.
PubMed Abstract»Chhatwal J, Kanwal F, Roberts MS, Dunn MA. Cost-effectiveness and budget impact of hepatitis C virus treatment with sofosbuvir and ledipasvir in the United States. Ann Intern Med. 2015;162:397-406.
PubMed Abstract»Chidi AP, Rogal S, Bryce CL, et al. Cost-effectiveness of new antiviral regimens for treatment-naïve U.S. veterans with hepatitis C. Hepatology. 2016;63:428-36.
PubMed Abstract»Chou R, Dana T, Fu R, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2020;323:1318.
PubMed Abstract»Crippin JS, McCashland T, Terrault N, Sheiner P, Charlton MR. A pilot study of the tolerability and efficacy of antiviral therapy in hepatitis C virus-infected patients awaiting liver transplantation. Liver Transpl. 2002;8:350-5.
PubMed Abstract»Curry MP, Forns X, Chung RT, et al. Sofosbuvir and ribavirin prevent recurrence of HCV infection after liver transplantation: an open-label study. Gastroenterology. 2015;148:100-107.
PubMed Abstract»Dore GJ, Altice F, Litwin AH, et al. Elbasvir-Grazoprevir to Treat Hepatitis C Virus Infection in Persons Receiving Opioid Agonist Therapy: A Randomized Trial. Ann Intern Med. 2016;165:625-634.
PubMed Abstract»Everson GT, Trotter J, Forman L, et al. Treatment of advanced hepatitis C with a low accelerating dosage regimen of antiviral therapy. Hepatology. 2005;42:255-62.
PubMed Abstract»Falade-Nwulia O, Momoh O, Felsher M, et al. Validation of a tool to assess effectiveness of peer-recruitment for hepatitis C testing and linkage to care among people who inject drugs. Drug Alcohol Depend. 2021;230:109177.
PubMed Abstract»Falade-Nwulia O, Suarez-Cuervo C, Nelson DR, Fried MW, Segal JB, Sulkowski MS. Oral Direct-Acting Agent Therapy for Hepatitis C Virus Infection: A Systematic Review. Ann Intern Med. 2017;166:637-48.
PubMed Abstract»Forns X, García-Retortillo M, Serrano T, et al. Antiviral therapy of patients with decompensated cirrhosis to prevent recurrence of hepatitis C after liver transplantation. J Hepatol. 2003;39:389-96.
PubMed Abstract»Grebely J, Dalgard O, Conway B, et al. Sofosbuvir and velpatasvir for hepatitis C virus infection in people with recent injection drug use (SIMPLIFY): an open-label, single-arm, phase 4, multicentre trial. Lancet Gastroenterol Hepatol. 2018;3:153-61.
PubMed Abstract»Hagan LM, Sulkowski MS, Schinazi RF. Cost analysis of sofosbuvir/ribavirin versus sofosbuvir/simeprevir for genotype 1 hepatitis C virus in interferon-ineligible/intolerant individuals. Hepatology. 2014;60:37-45.
PubMed Abstract»He T, Lopez-Olivo MA, Hur C, Chhatwal J. Systematic review: cost-effectiveness of direct-acting antivirals for treatment of hepatitis C genotypes 2-6. Aliment Pharmacol Ther. 2017;46:711-721.
PubMed Abstract»Hofmeister MG, Rosenthal EM, Barker LK, et al. Estimating Prevalence of Hepatitis C Virus Infection in the United States, 2013-2016. Hepatology. 2019;69:1020-31.
PubMed Abstract»Holmberg SD, Spradling PR, Moorman AC, Denniston MM. Hepatitis C in the United States. N Engl J Med. 2013;368:1859-61.
PubMed Abstract»Iacobellis A, Ippolito A, Andriulli A. Antiviral therapy in hepatitis C virus cirrhotic patients in compensated and decompensated condition. World J Gastroenterol. 2008;14:6467-72.
PubMed Abstract»Iacobellis A, Siciliano M, Perri F, et al. Peginterferon alfa-2b and ribavirin in patients with hepatitis C virus and decompensated cirrhosis: a controlled study. J Hepatol. 2007;46:206-12.
PubMed Abstract»Kattakuzhy S, Gross C, Emmanuel B, et al. Expansion of Treatment for Hepatitis C Virus Infection by Task Shifting to Community-Based Nonspecialist Providers: A Nonrandomized Clinical Trial. Ann Intern Med. 2017;167:311-318.
PubMed Abstract»Leidner AJ, Chesson HW, Xu F, Ward JW, Spradling PR, Holmberg SD. Cost-effectiveness of hepatitis C treatment for patients in early stages of liver disease. Hepatology. 2015;61:1860-9.
PubMed Abstract»Linas BP, Morgan JR, Pho MT, et al. Cost Effectiveness and Cost Containment in the Era of Interferon-Free Therapies to Treat Hepatitis C Virus Genotype 1. Open Forum Infect Dis. 2017;4:ofw266.
PubMed Abstract»Litwin AH, Lum PJ, Taylor LE, et al. Patient-centred models of hepatitis C treatment for people who inject drugs: a multicentre, pragmatic randomised trial. Lancet Gastroenterol Hepatol. 2022;7:1112-27.
PubMed Abstract»Maier MM, Ross DB, Chartier M, Belperio PS, Backus LI. Cascade of Care for Hepatitis C Virus Infection Within the US Veterans Health Administration. Am J Public Health. 2016;106:353-8.
PubMed Abstract»Martin NK, Vickerman P, Dore GJ, et al. Prioritization of HCV treatment in the direct-acting antiviral era: An economic evaluation. J Hepatol. 2016;65:17-25.
PubMed Abstract»Martin NK, Vickerman P, Grebely J, et al. Hepatitis C virus treatment for prevention among people who inject drugs: Modeling treatment scale-up in the age of direct-acting antivirals. Hepatology. 2013;58:1598-609.
PubMed Abstract»Mattingly TJ 2nd, Slejko JF, Mullins CD. Hepatitis C Treatment Regimens Are Cost-Effective: But Compared With What? Ann Pharmacother. 2017;51:961-9.
PubMed Abstract»Muir AJ, Poordad F, Lalezari J, et al. Daclatasvir in combination with asunaprevir and beclabuvir for hepatitis C virus genotype 1 infection with compensated cirrhosis. JAMA. 2015;313:1736-44.
PubMed Abstract»Najafzadeh M, Andersson K, Shrank WH, et al. Cost-effectiveness of novel regimens for the treatment of hepatitis C virus. Ann Intern Med. 2015;162:407-19.
PubMed Abstract»National Viral Hepatitis Roundtable (NVHR) and the Center for Health Law and Policy Innovation of Harvard Law School (CHLPI). Hepatitis C: The State of Medicaid Access. Preliminary Findings: National Summary Report. November 14, 2016.
NVHR & CHPI»Rein DB, Wittenborn JS, Smith BD, Liffmann DK, Ward JW. The cost-effectiveness, health benefits, and financial costs of new antiviral treatments for hepatitis C virus. Clin Infect Dis. 2015;61:157-68.
PubMed Abstract»Saab S, Gordon SC, Park H, Sulkowski M, Ahmed A, Younossi Z. Cost-effectiveness analysis of sofosbuvir plus peginterferon/ribavirin in the treatment of chronic hepatitis C virus genotype 1 infection. Aliment Pharmacol Ther. 2014;40:657-75.
PubMed Abstract»Saint-Laurent Thibault C, Moorjaney D, Ganz ML, et al. Cost-effectiveness of combination daclatasvir-sofosbuvir for treatment of genotype 3 chronic hepatitis C infection in the United States. J Med Econ. 2017;20:692-702.
PubMed Abstract»Saxena V, Nyberg L, Pauly M, et al. Safety and Efficacy of Simeprevir/Sofosbuvir in Hepatitis C-Infected Patients With Compensated and Decompensated Cirrhosis. Hepatology. 2015;62:715-25.
PubMed Abstract»Saxena V, Terrault N. Current Management of hepatitis C virus: regimens for peri-liver transplant patients. Clin Liver Dis. 2015;19:669-88.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Scott J, Fagalde M, Baer A, et al. A Population-Based Intervention to Improve Care Cascades of Patients With Hepatitis C Virus Infection. Hepatol Commun. 2021;5:387-9.
PubMed Abstract»Sethi N, Tapper EB, Vong A, Sethi S, Rourke M, Afdhal NH. Direct costs of first-generation protease inhibitors for the treatment of genotype 1 chronic hepatitis C viral infection. J Viral Hepat. 2015;22:974-6.
PubMed Abstract»Thomas RM, Brems JJ, Guzman-Hartman G, Yong S, Cavaliere P, Van Thiel DH. Infection with chronic hepatitis C virus and liver transplantation: a role for interferon therapy before transplantation. Liver Transpl. 2003;9:905-15.
PubMed Abstract»Tice JA, Chahal HS, Ollendorf DA. Comparative Clinical Effectiveness and Value of Novel Interferon-Free Combination Therapy for Hepatitis C Genotype 1: Summary of California Technology Assessment Forum Report. JAMA Intern Med. 2015;175:1559-60.
PubMed Abstract»Trooskin SB, Poceta J, Towey CM, et al. Results from a Geographically Focused, Community-Based HCV Screening, Linkage-to-Care and Patient Navigation Program. J Gen Intern Med. 2015;30:950-7.
PubMed Abstract»US Preventive Services Task Force, Owens DK, Davidson KW, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;323:970-5.
PubMed Abstract»Viner K, Kuncio D, Newbern EC, Johnson CC. The continuum of hepatitis C testing and care. Hepatology. 2015;61:783-9.
PubMed Abstract»World Health Organization. Global health sector strategy on viral hepatitis 2016-2021. Towards ending viral hepatitis. World Health Organization. June 2016:1-53.
WHO»Zibbell JE, Asher AK, Patel RC, et al. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am J Public Health. 2018;108:175-181.
PubMed Abstract»Zibbell JE, Hart-Malloy R, Barry J, Fan L, Flanigan C. Risk factors for HCV infection among young adults in rural New York who inject prescription opioid analgesics. Am J Public Health. 2014;104:2226-32.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»Module 5. Treatment of Hepatitis C Infection
Lesson 1. Simplified HCV Treatment for All HCV Genotypes
Introduction
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»National Academy of Medicine of the National Academies of Sciences, Engineering and Medicine. A National Strategy for the Elimination of Hepatitis B and C: Phase Two Report (2017)
National Academies»World Health Organization. Global Health Sector Strategy on Viral Hepatitis: 2016–2021. Towards ending viral hepatitis. June 2016.
World Health Organization»World Health Organization. Guidelines for the Care and treatment of persons diagnosed with chronic hepatitis C virus infection. July 2018.
World Health Organization»Eligibility for Simplified HCV Treatment: Initial Assessment
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of Adults with HCV infection.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with decompensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Beste LA, Green PK, Berry K, Kogut MJ, Allison SK, Ioannou GN. Effectiveness of hepatitis C antiviral treatment in a USA cohort of veteran patients with hepatocellular carcinoma. J Hepatol. 2017;67:32-9.
PubMed Abstract»Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»Jacobson IM, Lawitz E, Gane EJ, et al. Efficacy of 8 Weeks of Sofosbuvir, Velpatasvir, and Voxilaprevir in Patients With Chronic HCV Infection: 2 Phase 3 Randomized Trials. Gastroenterology. 2017;153:113-22.
PubMed Abstract»Jacobson IM, Poordad F, Firpi-Morell R, et al. Elbasvir/Grazoprevir in People With Hepatitis C Genotype 1 Infection and Child-Pugh Class B Cirrhosis: The C-SALT Study. Clin Transl Gastroenterol. 2019;10:e00007.
PubMed Abstract»Kaplan DE, Dai F, Aytaman A, et al. Development and Performance of an Algorithm to Estimate the Child-Turcotte-Pugh Score From a National Electronic Healthcare Database. Clin Gastroenterol Hepatol. 2015;13:2333-41.e1-6.
PubMed Abstract»Lawitz E, Poordad F, Gutierrez JA, et al. Simeprevir, daclatasvir and sofosbuvir for hepatitis C virus-infected patients with decompensated liver disease. J Viral Hepat. 2017;24:287-94.
PubMed Abstract»Mücke MM, Backus LI, Mücke VT, et al. Hepatitis B virus reactivation during direct-acting antiviral therapy for hepatitis C: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2018;3:172-80.
PubMed Abstract»Manns M, Samuel D, Gane EJ, et al. Ledipasvir and sofosbuvir plus ribavirin in patients with genotype 1 or 4 hepatitis C virus infection and advanced liver disease: a multicentre, open-label, randomised, phase 2 trial. Lancet Infect Dis. 2016;16:685-97.
PubMed Abstract»Sparkes T, Lemonovich TL. Interactions between anti-infective agents and immunosuppressants-Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33:e13510.
PubMed Abstract»Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43:1317-25.
PubMed Abstract»Welzel TM, Petersen J, Herzer K, et al. Daclatasvir plus sofosbuvir, with or without ribavirin, achieved high sustained virological response rates in patients with HCV infection and advanced liver disease in a real-world cohort. Gut. 2016;65:1861-1870.
PubMed Abstract»Simplified Treatment: Pretreatment Assessment for Patients without Cirrhosis
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of Adults with HCV infection.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»Centers for Disease Control and Prevention and Association of Public Health Laboratories. 2018 Quick reference guide: Recommended laboratory HIV testing algorithm for serum or plasma specimens. Published January 27, 2018.
CDC»Centers for Disease Control and Prevention and Association of Public Health Laboratories. Laboratory Testing for the Diagnosis of HIV Infection: Updated Recommendations. Published June 27, 2014.
CDC»Conners EE, Panagiotakopoulos L, Hofmeister MG, et al. Screening and Testing for Hepatitis B Virus Infection: CDC Recommendations - United States, 2023. MMWR Recomm Rep. 2023;72:1-25.
PubMed Abstract»Recommended Simplified Treatment Regimens for Patients without Cirrhosis
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»Asselah T, Kowdley KV, Zadeikis N, et al. Efficacy of Glecaprevir/Pibrentasvir for 8 or 12 Weeks in Patients With Hepatitis C Virus Genotype 2, 4, 5, or 6 Infection Without Cirrhosis. Clin Gastroenterol Hepatol. 2018;16:417-26.
PubMed Abstract»Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599-607.
PubMed Abstract»Foster GR, Afdhal N, Roberts SK, et al. Sofosbuvir and velpatasvir for HCV genotype 2 and 3 infection. N Engl J Med. 2015;373:2608-17.
PubMed Abstract»Solomon SS, Wagner-Cardoso S, Smeaton L, et al. A minimal monitoring approach for the treatment of hepatitis C virus infection (ACTG A5360 [MINMON]): a phase 4, open-label, single-arm trial. Lancet Gastroenterol Hepatol. 2022;7:307-17.
PubMed Abstract»Zeuzem S, Foster GR, Wang S, et al. Glecaprevir-Pibrentasvir for 8 or 12 Weeks in HCV Genotype 1 or 3 Infection. N Engl J Med. 2018;378:354-69.
PubMed Abstract»Monitoring on and after HCV Treatment in Patients without Cirrhosis
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»Abdel Alem S, Elsharkawy A, Fouad R, et al. Improvement of glycemic state among responders to Sofosbuvir-based treatment regimens: Single center experience. J Med Virol. 2017;89:2181-7.
PubMed Abstract»Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»DeCarolis DD, Westanmo AD, Chen YC, Boese AL, Walquist MA, Rector TS. Evaluation of a Potential Interaction Between New Regimens to Treat Hepatitis C and Warfarin. Ann Pharmacother. 2016;50:909-17.
PubMed Abstract»Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-80.
PubMed Abstract»Simplified Treatment: Pretreatment Assessment for Patients with Compensated Cirrhosis
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of Adults with HCV infection.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with decompensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»Esteban R, Pineda JA, Calleja JL, et al. Efficacy of Sofosbuvir and Velpatasvir, With and Without Ribavirin, in Patients With Hepatitis C Virus Genotype 3 Infection and Cirrhosis. Gastroenterology. 2018;155:1120-7.e4.
PubMed Abstract»Foster GR, Afdhal N, Roberts SK, et al. Sofosbuvir and velpatasvir for HCV genotype 2 and 3 infection. N Engl J Med. 2015;373:2608-17.
PubMed Abstract»Jacobson IM, Poordad F, Firpi-Morell R, et al. Elbasvir/Grazoprevir in People With Hepatitis C Genotype 1 Infection and Child-Pugh Class B Cirrhosis: The C-SALT Study. Clin Transl Gastroenterol. 2019;10:e00007.
PubMed Abstract»Kaplan DE, Dai F, Aytaman A, et al. Development and Performance of an Algorithm to Estimate the Child-Turcotte-Pugh Score From a National Electronic Healthcare Database. Clin Gastroenterol Hepatol. 2015;13:2333-41.e1-6.
PubMed Abstract»Lawitz E, Poordad F, Gutierrez JA, et al. Simeprevir, daclatasvir and sofosbuvir for hepatitis C virus-infected patients with decompensated liver disease. J Viral Hepat. 2017;24:287-94.
PubMed Abstract»Manns M, Samuel D, Gane EJ, et al. Ledipasvir and sofosbuvir plus ribavirin in patients with genotype 1 or 4 hepatitis C virus infection and advanced liver disease: a multicentre, open-label, randomised, phase 2 trial. Lancet Infect Dis. 2016;16:685-97.
PubMed Abstract»Wei L, Lim SG, Xie Q, et al. Sofosbuvir-velpatasvir for treatment of chronic hepatitis C virus infection in Asia: a single-arm, open-label, phase 3 trial. Lancet Gastroenterol Hepatol. 2019;4:127-34.
PubMed Abstract»Welzel TM, Petersen J, Herzer K, et al. Daclatasvir plus sofosbuvir, with or without ribavirin, achieved high sustained virological response rates in patients with HCV infection and advanced liver disease in a real-world cohort. Gut. 2016;65:1861-1870.
PubMed Abstract»Recommended Simplified Treatment Regimens for Patients with Compensated Cirrhosis
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»Monitoring On and After Treatment for Patients with Compensated Cirrhosis
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»Treatment Interruptions
Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»Cunningham EB, Amin J, Feld JJ, et al. Adherence to sofosbuvir and velpatasvir among people with chronic HCV infection and recent injection drug use: The SIMPLIFY study. Int J Drug Policy. 2018;62:14-23.
PubMed Abstract»Cunningham EB, Hajarizadeh B, Amin J, et al. Adherence to Once-daily and Twice-daily Direct-acting Antiviral Therapy for Hepatitis C Infection Among People With Recent Injection Drug Use or Current Opioid Agonist Therapy. Clin Infect Dis. 2020;71:e115-e124.
PubMed Abstract»Fabbiani M, Lombardi A, Colaneri M, et al. High rates of sustained virological response despite premature discontinuation of directly acting antivirals in HCV-infected patients treated in a real-life setting. J Viral Hepat. 2021;28:558-68.
PubMed Abstract»Serper M, Evon DM, Stewart PW, et al. Medication Non-adherence in a Prospective, Multi-center Cohort Treated with Hepatitis C Direct-Acting Antivirals. J Gen Intern Med. 2020;35:1011-20.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with decompensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Asselah T, Kowdley KV, Zadeikis N, et al. Efficacy of Glecaprevir/Pibrentasvir for 8 or 12 Weeks in Patients With Hepatitis C Virus Genotype 2, 4, 5, or 6 Infection Without Cirrhosis. Clin Gastroenterol Hepatol. 2018;16:417-26.
PubMed Abstract»Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»Brown RS Jr, Buti M, Rodrigues L, et al. Glecaprevir/pibrentasvir for 8 weeks in treatment-naïve patients with chronic HCV genotypes 1-6 and compensated cirrhosis: The EXPEDITION-8 trial. J Hepatol. 2020;72:441-9.
PubMed Abstract»Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599-607.
PubMed Abstract»Foster GR, Afdhal N, Roberts SK, et al. Sofosbuvir and velpatasvir for HCV genotype 2 and 3 infection. N Engl J Med. 2015;373:2608-17.
PubMed Abstract»Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-80.
PubMed Abstract»Hsieh YC, Jeng WJ, Huang CH, et al. Hepatic decompensation during paritaprevir/ritonavir/ombitasvir/dasabuvir treatment for genotype 1b chronic hepatitis C patients with advanced fibrosis and compensated cirrhosis. PLoS One. 2018;13:e0202777.
PubMed Abstract»Jacobson IM, Lawitz E, Gane EJ, et al. Efficacy of 8 Weeks of Sofosbuvir, Velpatasvir, and Voxilaprevir in Patients With Chronic HCV Infection: 2 Phase 3 Randomized Trials. Gastroenterology. 2017;153:113-22.
PubMed Abstract»Manns M, Samuel D, Gane EJ, et al. Ledipasvir and sofosbuvir plus ribavirin in patients with genotype 1 or 4 hepatitis C virus infection and advanced liver disease: a multicentre, open-label, randomised, phase 2 trial. Lancet Infect Dis. 2016;16:685-97.
PubMed Abstract»Office of HIV/AIDS and Infectious Disease Policy (OHAIDP). National Viral Hepatitis Action Plan. 2017-2020. January 2017.
HHS»Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43:1317-25.
PubMed Abstract»U.S. Department of Health and Human Services. 2020. Viral Hepatitis National Strategic Plan for the United States: A Roadmap to Elimination (2021–2025). Washington, DC.
HHS»Zeuzem S, Foster GR, Wang S, et al. Glecaprevir-Pibrentasvir for 8 or 12 Weeks in HCV Genotype 1 or 3 Infection. N Engl J Med. 2018;378:354-69.
PubMed Abstract»Lesson 2. Retreatment of Patients with Prior HCV Treatment Experience
Introduction
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV resistance primer.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed: Glecaprevir/Pibrentasvir Treatment Failures.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed: Multiple DAA Treatment Failures (All Genotypes), Including Sofosbuvir/Velpatasvir/Voxilaprevir or Sofosbuvir Plus Glecaprevir/Pibrentasvir.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed: Sofosbuvir-Based and Elbasvir/Grazoprevir Treatment Failures.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed.
AASLD-IDSA Hepatitis C Guidance»Special Considerations with Retreatment
Chang CH, Chen KY, Lai MY, Chan KA. Meta-analysis: ribavirin-induced haemolytic anaemia in patients with chronic hepatitis C. Aliment Pharmacol Ther. 2002;16:1623-32.
PubMed Abstract»Ward RP, Kugelmas M. Using pegylated interferon and ribavirin to treat patients with chronic hepatitis C. Am Fam Physician. 2005;72:655-62.
PubMed Abstract»Treatment Failure with Sofosbuvir-Containing DAA or Elbasvir-Grazoprevir
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed: Sofosbuvir-Based and Elbasvir/Grazoprevir Treatment Failures.
AASLD-IDSA Hepatitis C Guidance»Lok AS, Sulkowski MS, Kort JJ, et al. Efficacy of Glecaprevir and Pibrentasvir in Patients With Genotype 1 Hepatitis C Virus Infection With Treatment Failure After NS5A Inhibitor Plus Sofosbuvir Therapy. Gastroenterology. 2019;157:1506-17.
PubMed Abstract»Treatment Failure with Glecaprevir-Pibrentasvir
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed: Glecaprevir/Pibrentasvir Treatment Failures.
AASLD-IDSA Hepatitis C Guidance»Pearlman B, Perrys M, Hinds A. Sofosbuvir/Velpatasvir/Voxilaprevir for Previous Treatment Failures With Glecaprevir/Pibrentasvir in Chronic Hepatitis C Infection. Am J Gastroenterol. 2019;114:1550-2.
PubMed Abstract»Wyles D, Weiland O, Yao B, et al. Retreatment of patients who failed glecaprevir/pibrentasvir treatment for hepatitis C virus infection. J Hepatol. 2019;70:1019-23.
PubMed Abstract»Treatment Failure with Multiple DAA Regimens
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed: Multiple DAA Treatment Failures (All Genotypes), Including Sofosbuvir/Velpatasvir/Voxilaprevir or Sofosbuvir Plus Glecaprevir/Pibrentasvir.
AASLD-IDSA Hepatitis C Guidance»Bernhard B, Stickel F. Successful fourth line treatment of a relapse patient with chronic hepatitis C virus infection genotype 3a using sofosbuvir, glecaprevir/pibrentasvir, and ribavirin: a case report. Z Gastroenterol. 2020;58:451-5.
PubMed Abstract»Dietz J, Di Maio VC, de Salazar A, et al. Failure on voxilaprevir, velpatasvir, sofosbuvir and efficacy of rescue therapy. J Hepatol. 2021;74:801-10.
PubMed Abstract»Gane EJ, Shiffman ML, Etzkorn K, et al. Sofosbuvir-velpatasvir with ribavirin for 24 weeks in hepatitis C virus patients previously treated with a direct-acting antiviral regimen. Hepatology. 2017;66:1083-9.
PubMed Abstract»Ng TI, Krishnan P, Pilot-Matias T, et al. In Vitro Antiviral Activity and Resistance Profile of the Next-Generation Hepatitis C Virus NS5A Inhibitor Pibrentasvir. Antimicrob Agents Chemother. 2017;61:e02558-16.
PubMed Abstract»Ng TI, Tripathi R, Reisch T, et al. In Vitro Antiviral Activity and Resistance Profile of the Next-Generation Hepatitis C Virus NS3/4A Protease Inhibitor Glecaprevir. Antimicrob Agents Chemother. 2017;62:e01620-17.
PubMed Abstract»Wyles D, Weiland O, Yao B, et al. Retreatment of patients who failed glecaprevir/pibrentasvir treatment for hepatitis C virus infection. J Hepatol. 2019;70:1019-23.
PubMed Abstract»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Bourlière M, Gordon SC, Flamm SL, et al. Sofosbuvir, Velpatasvir, and Voxilaprevir for Previously Treated HCV Infection. N Engl J Med. 2017;376:2134-46.
PubMed Abstract»Bruggmann P, Dampz M, Gerlach T, Kravecz L, Falcato L. Treatment outcome in relation to alcohol consumption during hepatitis C therapy: an analysis of the Swiss Hepatitis C Cohort Study. Drug Alcohol Depend. 2010;110:167-71.
PubMed Abstract»Garbutt JC. The state of pharmacotherapy for the treatment of alcohol dependence. Journal of substance abuse treatment. 2009;36:S15-23; quiz S24-15.
PubMed Abstract»Innes HA, Hutchinson SJ, Barclay S, et al. Quantifying the fraction of cirrhosis attributable to alcohol among chronic HCV patients: Implications for treatment cost-effectiveness. Hepatology. 2012;57:451-60.
PubMed Abstract»Le Lan C, Guillygomarc'h A, Danielou H, et al. A multi-disciplinary approach to treating hepatitis C with interferon and ribavirin in alcohol-dependent patients with ongoing abuse. J Hepatol. 2012;56:334-40.
PubMed Abstract»Lok AS, Sulkowski MS, Kort JJ, et al. Efficacy of Glecaprevir and Pibrentasvir in Patients With Genotype 1 Hepatitis C Virus Infection With Treatment Failure After NS5A Inhibitor Plus Sofosbuvir Therapy. Gastroenterology. 2019;157:1506-17.
PubMed Abstract»McMahon BJ, Bruden D, Bruce MG, et al. Adverse outcomes in Alaska Natives who recovered from or have chronic hepatitis C infection. Gastroenterology. 2010;138:922-31.
PubMed Abstract»Pearlman B, Perrys M, Hinds A. Sofosbuvir/Velpatasvir/Voxilaprevir for Previous Treatment Failures With Glecaprevir/Pibrentasvir in Chronic Hepatitis C Infection. Am J Gastroenterol. 2019;114:1550-2.
PubMed Abstract»Perzynski AT, McCormick R, Webster NJ, et al. Psychosocial correlates of alcohol use and reduction for individuals with hepatitis C. Journal of studies on alcohol and drugs. 2011;72:787-98.
PubMed Abstract»Poordad F, Felizarta F, Asatryan A, et al. Glecaprevir and pibrentasvir for 12 weeks for hepatitis C virus genotype 1 infection and prior direct-acting antiviral treatment. Hepatology. 2017;66:389-97.
PubMed Abstract»Poordad F, Pol S, Asatryan A, et al. Glecaprevir/Pibrentasvir in patients with hepatitis C virus genotype 1 or 4 and past direct-acting antiviral treatment failure. Hepatology. 2018;67:1253-60.
PubMed Abstract»Poynard T, Bedossa P, Opolon P. Lancet. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825-32.
PubMed Abstract»Ward RP, Kugelmas M. Using pegylated interferon and ribavirin to treat patients with chronic hepatitis C. Am Fam Physician. 2005;72:655-62.
PubMed Abstract»Wiley TE, McCarthy M, Breidi L, McCarthy M, Layden TJ. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology. 1998;28:805-9.
PubMed Abstract»Wilson E, Covert E, Hoffmann J, et al. A pilot study of safety and efficacy of HCV retreatment with sofosbuvir/velpatasvir/voxilaprevir in patients with or without HIV (RESOLVE STUDY). J Hepatol. 2019;71:498-504.
PubMed Abstract»Wyles D, Poordad F, Wang S, et al. Glecaprevir/pibrentasvir for hepatitis C virus genotype 3 patients with cirrhosis and/or prior treatment experience: A partially randomized phase 3 clinical trial. Hepatology. 2018;67:514-23.
PubMed Abstract»Wyles D, Weiland O, Yao B, et al. Retreatment of patients who failed glecaprevir/pibrentasvir treatment for hepatitis C virus infection. J Hepatol. 2019;70:1019-23.
PubMed Abstract»Lesson 3. Monitoring During and After HCV Treatment
Background
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»Monitoring for Treatment Efficacy
Backus LI, Belperio PS, Shahoumian TA, Loomis TP, Mole LA. Real-world effectiveness of ledipasvir/sofosbuvir in 4,365 treatment-naive, genotype 1 hepatitis C-infected patients. Hepatology. 2016;64:405-14.
PubMed Abstract»Chevaliez S, Bouvier-Alias M, Brillet R, Pawlotsky JM. Overestimation and underestimation of hepatitis C virus RNA levels in a widely used real-time polymerase chain reaction-based method. Hepatology. 2007;46:22-31.
PubMed Abstract»Childs-Kean LM, Hong J. Detectable Viremia at the End of Treatment With Direct-Acting Antivirals Can Be Associated With Subsequent Clinical Cure in Patients With Chronic Hepatitis C: A Case Series. Gastroenterology. 2017;153:1165-1166.
PubMed Abstract»Cloherty G, Cohen D, Sarrazin C, et al. HCV RNA assay sensitivity impacts the management of patients treated with direct-acting antivirals. Antivir Ther. 2014;20:177-83.
PubMed Abstract»Cobb B, Pockros PJ, Vilchez RA, Vierling JM. HCV RNA viral load assessments in the era of direct-acting antivirals. Am J Gastroenterol. 2013;108:471-5.
PubMed Abstract»European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C: Final update of the series☆. J Hepatol. 2020:S0168-8278(20)30548-1.
EASL»Harrington PR, Deming DJ, Komatsu TE, Naeger LK. Hepatitis C virus RNA levels during interferon-free combination direct-acting antiviral treatment in registrational trials. Clin Infect Dis. 2015;61:666-7.
PubMed Abstract»Manns MP, Pockros PJ, Norkrans G, et al. Long-term clearance of hepatitis C virus following interferon α-2b or peginterferon α-2b, alone or in combination with ribavirin. J Viral Hepat. 2013;20:524-9.
PubMed Abstract»Morisco F, Granata R, Stroffolini T, et al. Sustained virological response: a milestone in the treatment of chronic hepatitis C. World J Gastroenterol. 2013;19:2793-8.
PubMed Abstract»Pearlman BL, Traub N. Sustained virologic response to antiviral therapy for chronic hepatitis C virus infection: a cure and so much more. Clin Infect Dis. 2011;52:889-900.
PubMed Abstract»Sidharthan S, Kohli A, Sims Z, et al. Utility of hepatitis C viral load monitoring on direct-acting antiviral therapy. Clin Infect Dis. 2015;60:1743-51.
PubMed Abstract»Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of Late Relapse or Reinfection With Hepatitis C Virus After Achieving a Sustained Virological Response: A Systematic Review and Meta-analysis. Clin Infect Dis. 2016;62:683-94.
PubMed Abstract»Steinebrunner N, Sprinzl MF, Zimmermann T, et al. Early virological response may predict treatment response in sofosbuvir-based combination therapy of chronic hepatitis c in a multi-center "real-life" cohort. BMC Gastroenterol. 2015;15:97.
PubMed Abstract»Strassl R, Rutter K, Stättermayer AF, et al. Real-Time PCR Assays for the Quantification of HCV RNA: Concordance, Discrepancies and Implications for Response Guided Therapy. PLoS One. 2015;10:e0135963.
PubMed Abstract»Vermehren J, Kau A, Görtner BC, Göbel R, Zeuzem S, Sarrazin C. Differences between two real-time PCR-based hepatitis C virus (HCV) assays (RealTime HCV and Cobas AmpliPrep/Cobas TaqMan) and one signal amplification assay (Versant HCV RNA 3.0) for RNA detection and quantification. J Clin Microbiol. 2008;46:3880-91.
PubMed Abstract»Yoshida EM, Sulkowski MS, Gane EJ, et al. Concordance of sustained virological response 4, 12, and 24 weeks post-treatment with sofosbuvir-containing regimens for hepatitis C virus. Hepatology. 2015;61:41-5.
PubMed Abstract»Monitoring for Safety at Baseline and During Treatment
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C: Final update of the series☆. J Hepatol. 2020:S0168-8278(20)30548-1.
EASL»U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA warns of serious liver injury risk with hepatitis C treatments Viekira Pak and Technivie
U.S. Food and Drug Administration»Hepatitis B Reactivation Associated with HCV DAA Therapy
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»Belperio PS, Shahoumian TA, Mole LA, Backus LI. Evaluation of hepatitis B reactivation among 62,920 veterans treated with oral hepatitis C antivirals. Hepatology. 2017;66:27-36.
PubMed Abstract»Bersoff-Matcha SJ, Cao K, Jason M, et al. Hepatitis B Virus Reactivation Associated With Direct-Acting Antiviral Therapy for Chronic Hepatitis C Virus: A Review of Cases Reported to the U.S. Food and Drug Administration Adverse Event Reporting System. Ann Intern Med. 2017;166:792-8.
PubMed Abstract»Collins JM, Raphael KL, Terry C, et al. Hepatitis B Virus Reactivation During Successful Treatment of Hepatitis C Virus With Sofosbuvir and Simeprevir. Clin Infect Dis. 2015;61:1304-6.
PubMed Abstract»De Monte A, Courjon J, Anty R, et al. Direct-acting antiviral treatment in adults infected with hepatitis C virus: Reactivation of hepatitis B virus coinfection as a further challenge. J Clin Virol. 2016;78:27-30.
PubMed Abstract»Ende AR, Kim NH, Yeh MM, Harper J, Landis CS. Fulminant hepatitis B reactivation leading to liver transplantation in a patient with chronic hepatitis C treated with simeprevir and sofosbuvir: a case report. J Med Case Rep. 2015;9:164.
PubMed Abstract»Hayashi K, Ishigami M, Ishizu Y, et al. A case of acute hepatitis B in a chronic hepatitis C patient after daclatasvir and asunaprevir combination therapy: hepatitis B virus reactivation or acute self-limited hepatitis? Clin J Gastroenterol. 2016;9:252-6.
PubMed Abstract»Ou P, Fang Z, Chen J. Hepatitis B reactivation in a chronic hepatitis C patient treated with ledipasvir and sofosbuvir: A case report. Clin Res Hepatol Gastroenterol. 2017;41:e17-e18.
PubMed Abstract»Pisaturo M, Macera M, Alessio L, Calò F, Coppola N. Hepatitis B Virus (HBV) Reactivation Following Pharmacological Eradication of Hepatitis C Virus (HCV). Viruses. 2019;11:850.
PubMed Abstract»Serper M, Forde KA, Kaplan DE. Rare clinically significant hepatic events and hepatitis B reactivation occur more frequently following rather than during direct-acting antiviral therapy for chronic hepatitis C: Data from a national US cohort. J Viral Hepat. 2018;25:187-197.
PubMed Abstract»Sulkowski MS, Chuang WL, Kao JH, et al. No Evidence of Reactivation of Hepatitis B Virus Among Patients Treated With Ledipasvir-Sofosbuvir for Hepatitis C Virus Infection. Clin Infect Dis. 2016;63:1202-1204.
PubMed Abstract»Takayama H, Sato T, Ikeda F, Fujiki S. Reactivation of hepatitis B virus during interferon-free therapy with daclatasvir and asunaprevir in patient with hepatitis B virus/hepatitis C virus co-infection. Hepatol Res. 2016;46:489-91.
PubMed Abstract»Terrault NA, Bzowej NH, Chang KM, Hwang JP, Jonas MM, Murad MH. AASLD guidelines for treatment of chronic hepatitis B. Hepatology. 2016;63:261-83.
PubMed Abstract»U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA warns about the risk of hepatitis B reactivating in some patients treated with direct-acting antivirals for hepatitis C.
U.S. Food and Drug Administration»Wang C, Ji D, Chen J, et al. Hepatitis due to Reactivation of Hepatitis B Virus in Endemic Areas Among Patients With Hepatitis C Treated With Direct-acting Antiviral Agents. Clin Gastroenterol Hepatol. 2017;15:132-6.
PubMed Abstract»Zhang K, Lai X, Song J, et al. A novel cell culture model reveals the viral interference during hepatitis B and C virus coinfection. Antiviral Res. 2021;189:105061.
PubMed Abstract»Monitoring After Receiving HCV Therapy
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335.
PubMed Abstract»Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922-38.
AASLD Practice Guidelines»Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-80.
PubMed Abstract»Ingiliz P, Martin TC, Rodger A, et al. HCV reinfection incidence and spontaneous clearance rates in HIV-positive men who have sex with men in Western Europe. J Hepatol. 2017;66:282-287.
PubMed Abstract»Manns MP, Pockros PJ, Norkrans G, et al. Long-term clearance of hepatitis C virus following interferon α-2b or peginterferon α-2b, alone or in combination with ribavirin. J Viral Hepat. 2013;20:524-9.
PubMed Abstract»Martin TC, Martin NK, Hickman M, et al. Hepatitis C virus reinfection incidence and treatment outcome among HIV-positive MSM. AIDS. 2013;27:2551-7.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Morisco F, Granata R, Stroffolini T, et al. Sustained virological response: a milestone in the treatment of chronic hepatitis C. World J Gastroenterol. 2013;19:2793-8.
PubMed Abstract»Pearlman BL, Traub N. Sustained virologic response to antiviral therapy for chronic hepatitis C virus infection: a cure and so much more. Clin Infect Dis. 2011;52:889-900.
PubMed Abstract»Sarrazin C, Isakov V, Svarovskaia ES, et al. Late Relapse Versus Hepatitis C Virus Reinfection in Patients With Sustained Virologic Response After Sofosbuvir-Based Therapies. Clin Infect Dis. 2017;64:44-52.
PubMed Abstract»Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of Late Relapse or Reinfection With Hepatitis C Virus After Achieving a Sustained Virological Response: A Systematic Review and Meta-analysis. Clin Infect Dis. 2016;62:683-94.
PubMed Abstract»Singal AG, Volk ML, Jensen D, Di Bisceglie AM, Schoenfeld PS. A sustained viral response is associated with reduced liver-related morbidity and mortality in patients with hepatitis C virus. Clin Gastroenterol Hepatol. 2010;8:280-8.
PubMed Abstract»Welker MW, Zeuzem S. Occult hepatitis C: how convincing are the current data? Hepatology. 2009;49:665-75.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Monitoring patients who are starting HCV treatment, are on treatment, or have completed therapy.
AASLD-IDSA HCV Guidance»Bajaj BS. Review article: the modern management of hepatic encephalopathy. Aliment Pharmacol Ther. 2010;31:537-47.
PubMed Abstract»Braun DL, Hampel B, Kouyos R, et al. High Cure Rates With Grazoprevir-Elbasvir With or Without Ribavirin Guided by Genotypic Resistance Testing Among Human Immunodeficiency Virus/Hepatitis C Virus-coinfected Men Who Have Sex With Men. Clin Infect Dis. 2019;68:569-76.
PubMed Abstract»Bustamante J, Rimola A, Ventura PJ, Navasa M, Cirera I, Reggiardo V, Rodés J. Prognostic significance of hepatic encephalopathy in patients with cirrhosis. J Hepatol. 1999;30:890-5.
PubMed Abstract»European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C: Final update of the series☆. J Hepatol. 2020:S0168-8278(20)30548-1.
EASL»Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335.
PubMed Abstract»Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-80.
PubMed Abstract»Ingiliz P, Martin TC, Rodger A, et al. HCV reinfection incidence and spontaneous clearance rates in HIV-positive men who have sex with men in Western Europe. J Hepatol. 2017;66:282-287.
PubMed Abstract»Martin TC, Martin NK, Hickman M, et al. Hepatitis C virus reinfection incidence and treatment outcome among HIV-positive MSM. AIDS. 2013;27:2551-7.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Morisco F, Granata R, Stroffolini T, et al. Sustained virological response: a milestone in the treatment of chronic hepatitis C. World J Gastroenterol. 2013;19:2793-8.
PubMed Abstract»Pearlman BL, Traub N. Sustained virologic response to antiviral therapy for chronic hepatitis C virus infection: a cure and so much more. Clin Infect Dis. 2011;52:889-900.
PubMed Abstract»Prakash R, Mullen KD. Mechanisms, diagnosis and management of hepatic encephalopathy. Nat Rev Gastroenterol Hepatol. 2010;7:515-25.
PubMed Abstract»Sarrazin C, Isakov V, Svarovskaia ES, et al. Late Relapse Versus Hepatitis C Virus Reinfection in Patients With Sustained Virologic Response After Sofosbuvir-Based Therapies. Clin Infect Dis. 2017;64:44-52.
PubMed Abstract»Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of Late Relapse or Reinfection With Hepatitis C Virus After Achieving a Sustained Virological Response: A Systematic Review and Meta-analysis. Clin Infect Dis. 2016;62:683-94.
PubMed Abstract»Singal AG, Volk ML, Jensen D, Di Bisceglie AM, Schoenfeld PS. A sustained viral response is associated with reduced liver-related morbidity and mortality in patients with hepatitis C virus. Clin Gastroenterol Hepatol. 2010;8:280-8.
PubMed Abstract»Yoshida EM, Sulkowski MS, Gane EJ, et al. Concordance of sustained virological response 4, 12, and 24 weeks post-treatment with sofosbuvir-containing regimens for hepatitis C virus. Hepatology. 2015;61:41-5.
PubMed Abstract»Lesson 4. Treatment of HCV in Persons with Cirrhosis
Background
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with decompensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»Akhtar E, Manne V, Saab S. Cirrhosis regression in hepatitis C patients with sustained virological response after antiviral therapy: a meta-analysis. Liver Int. 2014;35:30-6.
PubMed Abstract»Benvegnù L, Chemello L, Noventa F, Fattovich G, Pontisso P, Alberti A. Retrospective analysis of the effect of interferon therapy on the clinical outcome of patients with viral cirrhosis. Cancer. 1998;83:901-9.
PubMed Abstract»Cardoso AC, Moucari R, Figueiredo-Mendes C, et al. Impact of peginterferon and ribavirin therapy on hepatocellular carcinoma: incidence and survival in hepatitis C patients with advanced fibrosis. J Hepatol. 2010;52:652-7.
PubMed Abstract»Chan J, Gogela N, Zheng H, et al. Direct-Acting Antiviral Therapy for Chronic HCV Infection Results in Liver Stiffness Regression Over 12 Months Post-treatment. Dig Dis Sci. 2018;63:486-492.
PubMed Abstract»D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-31.
PubMed Abstract»D'Amico G, Morabito A, Pagliaro L, Marubini E. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig Dis Sci. 1986;31:468-75.
PubMed Abstract»Dohmen K, Kawano A, Takahashi K, et al. The incidence and risk factors for the development of hepatocellular carcinoma after peginterferon plus ribavirin therapy for chronic hepatitis C. Hepatogastroenterology. 2013;60:2034-8.
PubMed Abstract»Dufour JF, DeLellis R, Kaplan MM. Regression of hepatic fibrosis in hepatitis C with long-term interferon treatment. Dig Dis Sci. 1998;43:2573-6.
PubMed Abstract»Garcia-Tsao G, Friedman S, Iredale J, Pinzani M. Now there are many (stages) where before there was one: In search of a pathophysiological classification of cirrhosis. Hepatology. 2010;51:1445-9.
PubMed Abstract»Ge PS, Runyon BA. Treatment of Patients with Cirrhosis. N Engl J Med. 2016;375:767-77.
PubMed Abstract»Kobayashi N, Iijima H, Tada T, et al. Changes in liver stiffness and steatosis among patients with hepatitis C virus infection who received direct-acting antiviral therapy and achieved sustained virological response. Eur J Gastroenterol Hepatol. 2018;30:546-551.
PubMed Abstract»Marcellin F, Roux P, Protopopescu C, Duracinsky M, Spire B, Carrieri MP. Patient-reported outcomes with direct-acting antivirals for the treatment of chronic hepatitis C: current knowledge and outstanding issues. Expert Rev Gastroenterol Hepatol. 2017;11:259-268.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Pockros PJ, Hamzeh FM, Martin P, et al. Histologic outcomes in hepatitis C-infected patients with varying degrees of virologic response to interferon-based treatments. Hepatology. 2010;52:1193-200.
PubMed Abstract»Pol S, Carnot F, Nalpas B, et al. Reversibility of hepatitis C virus-related cirrhosis. Hum Pathol. 2004;35:107-12.
PubMed Abstract»Poynard T, McHutchison J, Manns M, et al. Impact of pegylated interferon alfa-2b and ribavirin on liver fibrosis in patients with chronic hepatitis C. Gastroenterology. 2002;122:1303-13.
PubMed Abstract»Poynard T, Moussalli J, Munteanu M, et al. Slow regression of liver fibrosis presumed by repeated biomarkers after virological cure in patients with chronic hepatitis C. J Hepatol. 2013;59:675-83.
PubMed Abstract»Shiratori Y, Imazeki F, Moriyama M, et al. Histologic improvement of fibrosis in patients with hepatitis C who have sustained response to interferon therapy. Ann Intern Med. 2000;132:517-24.
PubMed Abstract»Shiratori Y, Ito Y, Yokosuka O, et al. Antiviral therapy for cirrhotic hepatitis C: association with reduced hepatocellular carcinoma development and improved survival. Ann Intern Med. 2005;142:105-14.
PubMed Abstract»Singal AG, Volk ML, Jensen D, Di Bisceglie AM, Schoenfeld PS. A sustained viral response is associated with reduced liver-related morbidity and mortality in patients with hepatitis C virus. Clin Gastroenterol Hepatol. 2010;8:280-8.
PubMed Abstract»Singh S, Facciorusso A, Loomba R, Falck-Ytter YT. Magnitude and Kinetics of Decrease in Liver Stiffness After Antiviral Therapy in Patients With Chronic Hepatitis C: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2018;16:27-38.e4.
PubMed Abstract»Tada T, Kumada T, Toyoda H, et al. Improvement of liver stiffness in patients with hepatitis C virus infection who received direct-acting antiviral therapy and achieved sustained virological response. J Gastroenterol Hepatol. 2017;32:1982-8.
PubMed Abstract»Tada T, Kumada T, Toyoda H, et al. Viral eradication reduces all-cause mortality, including non-liver-related disease, in patients with progressive hepatitis C virus-related fibrosis. J Gastroenterol Hepatol. 2017;32:687-694.
PubMed Abstract»van der Meer AJ, Veldt BJ, Feld JJ, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012;308:2584-93.
PubMed Abstract»Impact of Treating HCV in Persons with Cirrhosis
Akhtar E, Manne V, Saab S. Cirrhosis regression in hepatitis C patients with sustained virological response after antiviral therapy: a meta-analysis. Liver Int. 2014;35:30-6.
PubMed Abstract»Chan J, Gogela N, Zheng H, et al. Direct-Acting Antiviral Therapy for Chronic HCV Infection Results in Liver Stiffness Regression Over 12 Months Post-treatment. Dig Dis Sci. 2018;63:486-492.
PubMed Abstract»Conti F, Buonfiglioli F, Scuteri A, et al. Early occurrence and recurrence of hepatocellular carcinoma in HCV-related cirrhosis treated with direct-acting antivirals. J Hepatol. 2016;65:727-733.
PubMed Abstract»Innes H, Barclay ST, Hayes PC, et al. The risk of hepatocellular carcinoma in cirrhotic patients with hepatitis C and sustained viral response: Role of the treatment regimen. J Hepatol. 2018;68:646-54.
PubMed Abstract»Kobayashi N, Iijima H, Tada T, et al. Changes in liver stiffness and steatosis among patients with hepatitis C virus infection who received direct-acting antiviral therapy and achieved sustained virological response. Eur J Gastroenterol Hepatol. 2018;30:546-551.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Ogawa E, Kawano A, Ooho A, et al. Long-term hepatic function of patients with compensated cirrhosis following successful direct-acting antiviral treatment for hepatitis C virus infection. J Gastroenterol Hepatol. 2022;37:371-7.
PubMed Abstract»Reig M, Mariño Z, Perelló C, et al. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J Hepatol. 2016;65:719-726.
PubMed Abstract»Rockey DC, Friedman SL. Fibrosis Regression After Eradication of Hepatitis C Virus: From Bench to Bedside. Gastroenterology. 2021;160:1502-20.e1.
PubMed Abstract»Simmons B, Saleem J, Heath K, Cooke GS, Hill A. Long-Term Treatment Outcomes of Patients Infected With Hepatitis C Virus: A Systematic Review and Meta-analysis of the Survival Benefit of Achieving a Sustained Virological Response. Clin Infect Dis. 2015;61:730-40.
PubMed Abstract»Singh S, Facciorusso A, Loomba R, Falck-Ytter YT. Magnitude and Kinetics of Decrease in Liver Stiffness After Antiviral Therapy in Patients With Chronic Hepatitis C: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2018;16:27-38.e4.
PubMed Abstract»Tada T, Kumada T, Toyoda H, et al. Improvement of liver stiffness in patients with hepatitis C virus infection who received direct-acting antiviral therapy and achieved sustained virological response. J Gastroenterol Hepatol. 2017;32:1982-8.
PubMed Abstract»Tada T, Kumada T, Toyoda H, et al. Viral eradication reduces all-cause mortality, including non-liver-related disease, in patients with progressive hepatitis C virus-related fibrosis. J Gastroenterol Hepatol. 2017;32:687-694.
PubMed Abstract»van der Meer AJ, Veldt BJ, Feld JJ, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012;308:2584-93.
PubMed Abstract»Verna EC, Morelli G, Terrault NA, et al. DAA therapy and long-term hepatic function in advanced/decompensated cirrhosis: Real-world experience from HCV-TARGET cohort. J Hepatol. 2020;73:540-548.
PubMed Abstract»Waziry R, Hajarizadeh B, Grebely J, et al. Hepatocellular carcinoma risk following direct-acting antiviral HCV therapy: A systematic review, meta-analyses, and meta-regression. J Hepatol. 2017;67:1204-1212.
PubMed Abstract»Treating HCV in Persons with Compensated Cirrhosis
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with decompensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»Afdhal N, Everson GT, Calleja JL, et al. Effect of viral suppression on hepatic venous pressure gradient in hepatitis C with cirrhosis and portal hypertension. J Viral Hepat. 2017;24:823-831.
PubMed Abstract»Afdhal N, Reddy KR, Nelson DR, et al. Ledipasvir and sofosbuvir for previously treated HCV genotype 1 infection. N Engl J Med. 2014;370:1483-93.
PubMed Abstract»Afdhal N, Zeuzem S, Kwo P, et al. Ledipasvir and sofosbuvir for untreated HCV genotype 1 infection. N Engl J Med. 2014;370:1889-98.
PubMed Abstract»Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»Bourlière M, Bronowicki JP, de Ledinghen V, et al. Ledipasvir-sofosbuvir with or without ribavirin to treat patients with HCV genotype 1 infection and cirrhosis non-responsive to previous protease-inhibitor therapy: a randomised, double-blind, phase 2 trial (SIRIUS). Lancet Infect Dis. 2015;15:397-404.
PubMed Abstract»Brown RS Jr, Buti M, Rodrigues L, et al. Glecaprevir/pibrentasvir for 8 weeks in treatment-naïve patients with chronic HCV genotypes 1-6 and compensated cirrhosis: The EXPEDITION-8 trial. J Hepatol. 2020;72:441-9.
PubMed Abstract»Bruno S, Shiffman ML, Roberts SK, Gane EJ, Messinger D, Hadziyannis SJ, Marcellin P. Efficacy and safety of peginterferon alfa-2a (40KD) plus ribavirin in hepatitis C patients with advanced fibrosis and cirrhosis. Hepatology. 2010;51:388-97.
PubMed Abstract»Buti M, Agarwal K, Horsmans Y, et al. Telaprevir twice daily is noninferior to telaprevir every 8 hrs for patients with chronic hepatitis C. Gastroenterology. 2014;146:744-53.
PubMed Abstract»Charlton M, Everson GT, Flamm SL, et al. Ledipasvir and sofosbuvir plus ribavirin for treatment of HCV infection in patients with advanced liver disease. Gastroenterology. 2015;149:649-59.
PubMed Abstract»Esteban R, Pineda JA, Calleja JL, et al. Efficacy of Sofosbuvir and Velpatasvir, With and Without Ribavirin, in Patients With Hepatitis C Virus Genotype 3 Infection and Cirrhosis. Gastroenterology. 2018;155:1120-7.e4.
PubMed Abstract»European Association for Study of the Liver. EASL Clinical Practice Guidelines: management of hepatitis C virus infection. J Hepatol. 2014;60:392-420.
PubMed Abstract»Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599-607.
PubMed Abstract»Foster GR, Afdhal N, Roberts SK, et al. Sofosbuvir and velpatasvir for HCV genotype 2 and 3 infection. N Engl J Med. 2015;373:2608-17.
PubMed Abstract»Foster GR, Irving WL, Cheung MC, et al. Impact of direct acting antiviral therapy in patients with chronic hepatitis C and decompensated cirrhosis. J Hepatol. 2016;64:1224-31.
PubMed Abstract»Fried MW, Shiffman ML, Reddy KR, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med. 2002;347:975-82.
PubMed Abstract»Gane E, Poordad F, Zadeikis N, et al. Safety and Pharmacokinetics of Glecaprevir/Pibrentasvir in Adults With Chronic Genotype 1-6 Hepatitis C Virus Infections and Compensated Liver Disease. Clin Infect Dis. 2019;69:1657-64.
PubMed Abstract»Hézode C, Fontaine H, Dorival C, et al. Effectiveness of telaprevir or boceprevir in treatment-experienced patients with HCV genotype 1 infection and cirrhosis. Gastroenterology. 2014;147:132-142.e4.
PubMed Abstract»Hézode C, Fontaine H, Dorival C, et al. Triple therapy in treatment-experienced patients with HCV-cirrhosis in a multicentre cohort of the French Early Access Programme (ANRS CO20-CUPIC) - NCT01514890. J Hepatol. 2013;59:434-41.
PubMed Abstract»Hadziyannis SJ, Sette H Jr, Morgan TR, et al. Peginterferon-alfa2a and ribavirin combination therapy in chronic hepatitis C: a randomized study of treatment duration and ribavirin dose. Ann Intern Med. 2004;140:346–55.
PubMed Abstract»Heathcote EJ, Shiffman ML, Cooksley WG, et al. Peginterferon alfa-2a in patients with chronic hepatitis C and cirrhosis. N Engl J Med. 2000;343:1673-80.
PubMed Abstract»Helbling B, Jochum W, Stamenic I, et al. HCV-related advanced fibrosis/cirrhosis: randomized controlled trial of pegylated interferon alpha-2a and ribavirin. J Viral Hepat. 2006;13:762-9.
PubMed Abstract»Jacobson IM, Lawitz E, Gane EJ, et al. Efficacy of 8 Weeks of Sofosbuvir, Velpatasvir, and Voxilaprevir in Patients With Chronic HCV Infection: 2 Phase 3 Randomized Trials. Gastroenterology. 2017;153:113-22.
PubMed Abstract»Jacobson IM, Lawitz E, Kwo PY, et al. Safety and Efficacy of Elbasvir/Grazoprevir in Patients With Hepatitis C Virus Infection and Compensated Cirrhosis: An Integrated Analysis. Gastroenterology. 2017;152:1372-1382.e2.
PubMed Abstract»Jacobson IM, McHutchison JG, Dusheiko G, et al. Telaprevir for previously untreated chronic hepatitis C virus infection. N Engl J Med. 2011;364:2405-16.
PubMed Abstract»Lawitz E, Poordad F, Brainard DM, et al. Sofosbuvir with peginterferon-ribavirin for 12 weeks in previously treated patients with hepatitis C genotype 2 or 3 and cirrhosis. Hepatology. 2015;61:769-75.
PubMed Abstract»Lawitz E, Sulkowski MS, Ghalib R, et al. Simeprevir plus sofosbuvir, with or without ribavirin, to treat chronic infection with hepatitis C virus genotype 1 in non-responders to pegylated interferon and ribavirin and treatment-naive patients: the COSMOS randomised study. Lancet. 2014;384:1756-65.
PubMed Abstract»Manns MP, McHutchison JG, Gordon SC, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet. 2001;358:958-65.
PubMed Abstract»McHutchison JG, Everson GT, Gordon SC, et al. Telaprevir with peginterferon and ribavirin for chronic HCV genotype 1 infection. N Engl J Med. 2009;360:1827-38.
PubMed Abstract»Muir AJ, Poordad F, Lalezari J, et al. Daclatasvir in combination with asunaprevir and beclabuvir for hepatitis C virus genotype 1 infection with compensated cirrhosis. JAMA. 2015;313:1736-44.
PubMed Abstract»Poordad F, Hezode C, Trinh R, et al. ABT-450/r-ombitasvir and dasabuvir with ribavirin for hepatitis C with cirrhosis. N Engl J Med. 2014;370:1973-82.
PubMed Abstract»Poordad F, McCone J Jr, Bacon BR, et al. Boceprevir for untreated chronic HCV genotype 1 infection. N Engl J Med. 2011;364:1195-206.
PubMed Abstract»Reddy KR, Bourlière M, Sulkowski M, et al. Ledipasvir and sofosbuvir in patients with genotype 1 hepatitis C virus infection and compensated cirrhosis: An integrated safety and efficacy analysis. Hepatology. 2015;62:79-86.
PubMed Abstract»Vierling JM, Zeuzem S, Poordad F, et al. Safety and efficacy of boceprevir/peginterferon/ribavirin for HCV G1 compensated cirrhotics: Meta-analysis of 5 trials. J Hepatol. 2014;61:200-9.
PubMed Abstract»Zeuzem S, Dusheiko GM, Salupere R, et al. Sofosbuvir and ribavirin in HCV genotypes 2 and 3. N Engl J Med. 2014;370:1993-2001.
PubMed Abstract»Treating HCV in Persons with Decompensated Cirrhosis
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with decompensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»Afdhal N, Everson GT, Calleja JL, et al. Effect of viral suppression on hepatic venous pressure gradient in hepatitis C with cirrhosis and portal hypertension. J Viral Hepat. 2017;24:823-831.
PubMed Abstract»Ahmed A, Gonzalez SA, Cholankeril G, et al. Treatment of patients waitlisted for liver transplant with all-oral direct-acting antivirals is a cost-effective treatment strategy in the United States. Hepatology. 2017;66:46-56.
PubMed Abstract»Belli LS, Berenguer M, Cortesi PA, et al. Delisting of liver transplant candidates with chronic hepatitis C after viral eradication: A European study. J Hepatol. 2016;65:524-31.
PubMed Abstract»Charlton M, Everson GT, Flamm SL, et al. Ledipasvir and sofosbuvir plus ribavirin for treatment of HCV infection in patients with advanced liver disease. Gastroenterology. 2015;149:649-59.
PubMed Abstract»Crippin JS, McCashland T, Terrault N, Sheiner P, Charlton MR. A pilot study of the tolerability and efficacy of antiviral therapy in hepatitis C virus-infected patients awaiting liver transplantation. Liver Transpl. 2002;8:350-5.
PubMed Abstract»Curry MP, Forns X, Chung RT, et al. Sofosbuvir and ribavirin prevent recurrence of HCV infection after liver transplantation: an open-label study. Gastroenterology. 2015;148:100-107.
PubMed Abstract»Curry MP, O'Leary JG, Bzowej N, et al. Sofosbuvir and Velpatasvir for HCV in Patients with Decompensated Cirrhosis. N Engl J Med. 2015;373:2618-28.
PubMed Abstract»D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-31.
PubMed Abstract»Everson GT, Trotter J, Forman L, et al. Treatment of advanced hepatitis C with a low accelerating dosage regimen of antiviral therapy. Hepatology. 2005;42:255-62.
PubMed Abstract»Flemming JA, Kim WR, Brosgart CL, Terrault NA. Reduction in liver transplant wait-listing in the era of direct-acting antiviral therapy. Hepatology. 2017;65:804-12.
PubMed Abstract»Forns X, García-Retortillo M, Serrano T, et al. Antiviral therapy of patients with decompensated cirrhosis to prevent recurrence of hepatitis C after liver transplantation. J Hepatol. 2003;39:389-96.
PubMed Abstract»Garcia-Tsao G, Friedman S, Iredale J, Pinzani M. Now there are many (stages) where before there was one: In search of a pathophysiological classification of cirrhosis. Hepatology. 2010;51:1445-9.
PubMed Abstract»Ge PS, Runyon BA. Treatment of Patients with Cirrhosis. N Engl J Med. 2016;375:767-77.
PubMed Abstract»Iacobellis A, Ippolito A, Andriulli A. Antiviral therapy in hepatitis C virus cirrhotic patients in compensated and decompensated condition. World J Gastroenterol. 2008;14:6467-72.
PubMed Abstract»Iacobellis A, Siciliano M, Perri F, et al. Peginterferon alfa-2b and ribavirin in patients with hepatitis C virus and decompensated cirrhosis: a controlled study. J Hepatol. 2007;46:206-12.
PubMed Abstract»Krassenburg LAP, Maan R, Ramji A, et al. Clinical outcomes following DAA therapy in patients with HCV-related cirrhosis depend on disease severity. J Hepatol. 2021;74:1053-63.
PubMed Abstract»Li J, Wu V, Pan CQ. Direct antiviral therapy for hepatitis C cirrhotic patients in liver transplantation settings: a systematic review. Hepatol Int. 2022;16:1020-31.
PubMed Abstract»Manns M, Samuel D, Gane EJ, et al. Ledipasvir and sofosbuvir plus ribavirin in patients with genotype 1 or 4 hepatitis C virus infection and advanced liver disease: a multicentre, open-label, randomised, phase 2 trial. Lancet Infect Dis. 2016;16:685-97.
PubMed Abstract»Muir AJ, Poordad F, Lalezari J, et al. Daclatasvir in combination with asunaprevir and beclabuvir for hepatitis C virus genotype 1 infection with compensated cirrhosis. JAMA. 2015;313:1736-44.
PubMed Abstract»Poordad F, Schiff ER, Vierling JM, et al. Daclatasvir with sofosbuvir and ribavirin for hepatitis C virus infection with advanced cirrhosis or post-liver transplantation recurrence. Hepatology. 2016;63:1493-505.
PubMed Abstract»Saxena V, Nyberg L, Pauly M, et al. Safety and Efficacy of Simeprevir/Sofosbuvir in Hepatitis C-Infected Patients With Compensated and Decompensated Cirrhosis. Hepatology. 2015;62:715-25.
PubMed Abstract»Saxena V, Terrault N. Current Management of hepatitis C virus: regimens for peri-liver transplant patients. Clin Liver Dis. 2015;19:669-88.
PubMed Abstract»Snyder HS, Wiegel JJ, Khalil K, et al. A systematic review of direct acting antiviral therapies in hepatitis C virus-negative liver transplant recipients of hepatitis C-viremic donors. Pharmacotherapy. 2022;42:905-20.
PubMed Abstract»Takehara T, Sakamoto N, Nishiguchi S, et al. Efficacy and safety of sofosbuvir-velpatasvir with or without ribavirin in HCV-infected Japanese patients with decompensated cirrhosis: an open-label phase 3 trial. J Gastroenterol. 2019;54:87-95.
PubMed Abstract»Thomas RM, Brems JJ, Guzman-Hartman G, Yong S, Cavaliere P, Van Thiel DH. Infection with chronic hepatitis C virus and liver transplantation: a role for interferon therapy before transplantation. Liver Transpl. 2003;9:905-15.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy failed.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with decompensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»Afdhal N, Everson GT, Calleja JL, et al. Effect of viral suppression on hepatic venous pressure gradient in hepatitis C with cirrhosis and portal hypertension. J Viral Hepat. 2017;24:823-831.
PubMed Abstract»Afdhal N, Reddy KR, Nelson DR, et al. Ledipasvir and sofosbuvir for previously treated HCV genotype 1 infection. N Engl J Med. 2014;370:1483-93.
PubMed Abstract»Afdhal N, Zeuzem S, Kwo P, et al. Ledipasvir and sofosbuvir for untreated HCV genotype 1 infection. N Engl J Med. 2014;370:1889-98.
PubMed Abstract»Akhtar E, Manne V, Saab S. Cirrhosis regression in hepatitis C patients with sustained virological response after antiviral therapy: a meta-analysis. Liver Int. 2014;35:30-6.
PubMed Abstract»Akhtar E, Manne V, Saab S. Cirrhosis regression in hepatitis C patients with sustained virological response after antiviral therapy: a meta-analysis. Liver Int. 2015;35:30-6.
PubMed Abstract»Benvegnù L, Chemello L, Noventa F, Fattovich G, Pontisso P, Alberti A. Retrospective analysis of the effect of interferon therapy on the clinical outcome of patients with viral cirrhosis. Cancer. 1998;83:901-9.
PubMed Abstract»Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»Bourlière M, Bronowicki JP, de Ledinghen V, et al. Ledipasvir-sofosbuvir with or without ribavirin to treat patients with HCV genotype 1 infection and cirrhosis non-responsive to previous protease-inhibitor therapy: a randomised, double-blind, phase 2 trial (SIRIUS). Lancet Infect Dis. 2015;15:397-404.
PubMed Abstract»Brown RS Jr, Buti M, Rodrigues L, et al. Glecaprevir/pibrentasvir for 8 weeks in treatment-naïve patients with chronic HCV genotypes 1-6 and compensated cirrhosis: The EXPEDITION-8 trial. J Hepatol. 2020;72:441-9.
PubMed Abstract»Bruno S, Shiffman ML, Roberts SK, Gane EJ, Messinger D, Hadziyannis SJ, Marcellin P. Efficacy and safety of peginterferon alfa-2a (40KD) plus ribavirin in hepatitis C patients with advanced fibrosis and cirrhosis. Hepatology. 2010;51:388-97.
PubMed Abstract»Burton JR Jr, O'Leary JG, Verna EC, et al. A US multicenter study of hepatitis C treatment of liver transplant recipients with protease-inhibitor triple therapy. J Hepatol. 2014;61:508-14.
PubMed Abstract»Buti M, Agarwal K, Horsmans Y, et al. Telaprevir twice daily is noninferior to telaprevir every 8 hrs for patients with chronic hepatitis C. Gastroenterology. 2014;146:744-53.
PubMed Abstract»Cardoso AC, Moucari R, Figueiredo-Mendes C, et al. Impact of peginterferon and ribavirin therapy on hepatocellular carcinoma: incidence and survival in hepatitis C patients with advanced fibrosis. J Hepatol. 2010;52:652-7.
PubMed Abstract»Chan J, Gogela N, Zheng H, et al. Direct-Acting Antiviral Therapy for Chronic HCV Infection Results in Liver Stiffness Regression Over 12 Months Post-treatment. Dig Dis Sci. 2018;63:486-492.
PubMed Abstract»Charlton M, Everson GT, Flamm SL, et al. Ledipasvir and sofosbuvir plus ribavirin for treatment of HCV infection in patients with advanced liver disease. Gastroenterology. 2015;149:649-59.
PubMed Abstract»Colombo M, Strasser S, Moreno C, et al. Sustained virological response with telaprevir in 1,078 patients with advanced hepatitis C: the international telaprevir access program. J Hepatol. 2014;61:976-83.
PubMed Abstract»Crippin JS, McCashland T, Terrault N, Sheiner P, Charlton MR. A pilot study of the tolerability and efficacy of antiviral therapy in hepatitis C virus-infected patients awaiting liver transplantation. Liver Transpl. 2002;8:350-5.
PubMed Abstract»Curry MP, Forns X, Chung RT, et al. Sofosbuvir and ribavirin prevent recurrence of HCV infection after liver transplantation: an open-label study. Gastroenterology. 2015;148:100-107.
PubMed Abstract»Curry MP, O'Leary JG, Bzowej N, et al. Sofosbuvir and Velpatasvir for HCV in Patients with Decompensated Cirrhosis. N Engl J Med. 2015;373:2618-28.
PubMed Abstract»D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-31.
PubMed Abstract»D'Amico G, Morabito A, Pagliaro L, Marubini E. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig Dis Sci. 1986;31:468-75.
PubMed Abstract»Daniel KE, Said A. Considerations When Treating Hepatitis C in a Cirrhotic Transplant Candidate. Curr Gastroenterol Rep. 2018;20:20.
PubMed Abstract»Dohmen K, Kawano A, Takahashi K, et al. The incidence and risk factors for the development of hepatocellular carcinoma after peginterferon plus ribavirin therapy for chronic hepatitis C. Hepatogastroenterology. 2013;60:2034-8.
PubMed Abstract»Dufour JF, DeLellis R, Kaplan MM. Regression of hepatic fibrosis in hepatitis C with long-term interferon treatment. Dig Dis Sci. 1998;43:2573-6.
PubMed Abstract»El-Sherif O, Jiang ZG, Tapper EB, et al. Baseline Factors Associated With Improvements in Decompensated Cirrhosis After Direct-Acting Antiviral Therapy for Hepatitis C Virus Infection. Gastroenterology. 2018;154:2111-2121.e8.
PubMed Abstract»Esteban R, Pineda JA, Calleja JL, et al. Efficacy of Sofosbuvir and Velpatasvir, With and Without Ribavirin, in Patients With Hepatitis C Virus Genotype 3 Infection and Cirrhosis. Gastroenterology. 2018;155:1120-7.e4.
PubMed Abstract»European Association for Study of the Liver. EASL Clinical Practice Guidelines: management of hepatitis C virus infection. J Hepatol. 2014;60:392-420.
PubMed Abstract»Everson GT, Terrault NA, Lok AS, et al. A randomized controlled trial of pretransplant antiviral therapy to prevent recurrence of hepatitis C after liver transplantation. Hepatology. 2013;57:1752-62.
PubMed Abstract»Everson GT, Trotter J, Forman L, et al. Treatment of advanced hepatitis C with a low accelerating dosage regimen of antiviral therapy. Hepatology. 2005;42:255-62.
PubMed Abstract»Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599-607.
PubMed Abstract»Flemming JA, Kim WR, Brosgart CL, Terrault NA. Reduction in liver transplant wait-listing in the era of direct-acting antiviral therapy. Hepatology. 2017;65:804-12.
PubMed Abstract»Forestier N, Zeuzem S. Triple therapy with telaprevir: results in hepatitis C virus-genotype 1 infected relapsers and non-responders. Liver Int. 2012;32 Suppl 1:44-50.
PubMed Abstract»Forman LM, Lewis JD, Berlin JA, Feldman HI, Lucey MR. The association between hepatitis C infection and survival after orthotopic liver transplantation. Gastroenterology. 2002;122:889-96.
PubMed Abstract»Forman LM. To transplant or not to transplant recurrent hepatitis C and liver failure. Clin Liver Dis. 2003;7:615-29.
PubMed Abstract»Forns X, García-Retortillo M, Serrano T, et al. Antiviral therapy of patients with decompensated cirrhosis to prevent recurrence of hepatitis C after liver transplantation. J Hepatol. 2003;39:389-96.
PubMed Abstract»Foster GR, Afdhal N, Roberts SK, et al. Sofosbuvir and velpatasvir for HCV genotype 2 and 3 infection. N Engl J Med. 2015;373:2608-17.
PubMed Abstract»Foster GR, Irving WL, Cheung MC, et al. Impact of direct acting antiviral therapy in patients with chronic hepatitis C and decompensated cirrhosis. J Hepatol. 2016;64:1224-31.
PubMed Abstract»Fried MW, Shiffman ML, Reddy KR, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med. 2002;347:975-82.
PubMed Abstract»Gane EJ, Portmann BC, Naoumov NV, et al. Long-term outcome of hepatitis C infection after liver transplantation. N Engl J Med. 1996;334:815-20.
PubMed Abstract»García-Álvarez M, Pineda-Tenor D, Jiménez-Sousa MA, Fernández-Rodríguez A, Guzmán-Fulgencio M, Resino S. Relationship of vitamin D status with advanced liver fibrosis and response to hepatitis C virus therapy: A meta-analysis. Hepatology. 2014;60:1541-50.
PubMed Abstract»Garcia-Retortillo M, Forns X, Feliu A, et al. Hepatitis C virus kinetics during and immediately after liver transplantation. Hepatology. 2002;35:680-7.
PubMed Abstract»Garcia-Tsao G, Friedman S, Iredale J, Pinzani M. Now there are many (stages) where before there was one: In search of a pathophysiological classification of cirrhosis. Hepatology. 2010;51:1445-9.
PubMed Abstract»Ge PS, Runyon BA. Treatment of Patients with Cirrhosis. N Engl J Med. 2016;375:767-77.
PubMed Abstract»Hézode C, Fontaine H, Dorival C, et al. Effectiveness of telaprevir or boceprevir in treatment-experienced patients with HCV genotype 1 infection and cirrhosis. Gastroenterology. 2014;147:132-142.e4.
PubMed Abstract»Hézode C, Fontaine H, Dorival C, et al. Triple therapy in treatment-experienced patients with HCV-cirrhosis in a multicentre cohort of the French Early Access Programme (ANRS CO20-CUPIC) - NCT01514890. J Hepatol. 2013;59:434-41.
PubMed Abstract»Hadziyannis SJ, Sette H Jr, Morgan TR, et al. Peginterferon-alfa2a and ribavirin combination therapy in chronic hepatitis C: a randomized study of treatment duration and ribavirin dose. Ann Intern Med. 2004;140:346–55.
PubMed Abstract»Heathcote EJ, Shiffman ML, Cooksley WG, et al. Peginterferon alfa-2a in patients with chronic hepatitis C and cirrhosis. N Engl J Med. 2000;343:1673-80.
PubMed Abstract»Helbling B, Jochum W, Stamenic I, et al. HCV-related advanced fibrosis/cirrhosis: randomized controlled trial of pegylated interferon alpha-2a and ribavirin. J Viral Hepat. 2006;13:762-9.
PubMed Abstract»Iacobellis A, Ippolito A, Andriulli A. Antiviral therapy in hepatitis C virus cirrhotic patients in compensated and decompensated condition. World J Gastroenterol. 2008;14:6467-72.
PubMed Abstract»Iacobellis A, Siciliano M, Perri F, et al. Peginterferon alfa-2b and ribavirin in patients with hepatitis C virus and decompensated cirrhosis: a controlled study. J Hepatol. 2007;46:206-12.
PubMed Abstract»Jacobson IM, Lawitz E, Gane EJ, et al. Efficacy of 8 Weeks of Sofosbuvir, Velpatasvir, and Voxilaprevir in Patients With Chronic HCV Infection: 2 Phase 3 Randomized Trials. Gastroenterology. 2017;153:113-22.
PubMed Abstract»Jacobson IM, McHutchison JG, Dusheiko G, et al. Telaprevir for previously untreated chronic hepatitis C virus infection. N Engl J Med. 2011;364:2405-16.
PubMed Abstract»Joshi D, Pinzani M, Carey I, Agarwal K. Recurrent HCV after liver transplantation-mechanisms, assessment and therapy. Nat Rev Gastroenterol Hepatol. 2014;11:710-21.
PubMed Abstract»Lawitz E, Poordad F, Brainard DM, et al. Sofosbuvir with peginterferon-ribavirin for 12 weeks in previously treated patients with hepatitis C genotype 2 or 3 and cirrhosis. Hepatology. 2015;61:769-75.
PubMed Abstract»Lawitz E, Sulkowski MS, Ghalib R, et al. Simeprevir plus sofosbuvir, with or without ribavirin, to treat chronic infection with hepatitis C virus genotype 1 in non-responders to pegylated interferon and ribavirin and treatment-naive patients: the COSMOS randomised study. Lancet. 2014;384:1756-65.
PubMed Abstract»Lens S, Gambato M, Londoño MC, Forns X. Interferon-free regimens in the liver-transplant setting. Semin Liver Dis. 2014;34:58-71.
PubMed Abstract»Leroy V, Angus P, Bronowicki JP, et al. Daclatasvir, sofosbuvir, and ribavirin for hepatitis C virus genotype 3 and advanced liver disease: A randomized phase III study (ALLY-3+). Hepatology. 2016;63:1430-41.
PubMed Abstract»Leroy V, Dumortier J, Coilly A, et al. Efficacy of Sofosbuvir and Daclatasvir in Patients With Fibrosing Cholestatic Hepatitis C After Liver Transplantation. Clin Gastroenterol Hepatol. 2015;13:1993-2001.e1-2.
PubMed Abstract»Manns M, Samuel D, Gane EJ, et al. Ledipasvir and sofosbuvir plus ribavirin in patients with genotype 1 or 4 hepatitis C virus infection and advanced liver disease: a multicentre, open-label, randomised, phase 2 trial. Lancet Infect Dis. 2016;16:685-97.
PubMed Abstract»Manns MP, McHutchison JG, Gordon SC, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet. 2001;358:958-65.
PubMed Abstract»Marcellin F, Roux P, Protopopescu C, Duracinsky M, Spire B, Carrieri MP. Patient-reported outcomes with direct-acting antivirals for the treatment of chronic hepatitis C: current knowledge and outstanding issues. Expert Rev Gastroenterol Hepatol. 2017;11:259-268.
PubMed Abstract»McHutchison JG, Lawitz EJ, Shiffman ML, et al. Peginterferon alfa-2b or alfa-2a with ribavirin for treatment of hepatitis C infection. N Engl J Med. 2009;361:580-93.
PubMed Abstract»Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-37.
PubMed Abstract»Muir AJ, Poordad F, Lalezari J, et al. Daclatasvir in combination with asunaprevir and beclabuvir for hepatitis C virus genotype 1 infection with compensated cirrhosis. JAMA. 2015;313:1736-44.
PubMed Abstract»Pockros PJ, Hamzeh FM, Martin P, et al. Histologic outcomes in hepatitis C-infected patients with varying degrees of virologic response to interferon-based treatments. Hepatology. 2010;52:1193-200.
PubMed Abstract»Pol S, Carnot F, Nalpas B, et al. Reversibility of hepatitis C virus-related cirrhosis. Hum Pathol. 2004;35:107-12.
PubMed Abstract»Poordad F, Hezode C, Trinh R, et al. ABT-450/r-ombitasvir and dasabuvir with ribavirin for hepatitis C with cirrhosis. N Engl J Med. 2014;370:1973-82.
PubMed Abstract»Poordad F, McCone J Jr, Bacon BR, et al. Boceprevir for untreated chronic HCV genotype 1 infection. N Engl J Med. 2011;364:1195-206.
PubMed Abstract»Poynard T, McHutchison J, Manns M, et al. Impact of pegylated interferon alfa-2b and ribavirin on liver fibrosis in patients with chronic hepatitis C. Gastroenterology. 2002;122:1303-13.
PubMed Abstract»Poynard T, Moussalli J, Munteanu M, et al. Slow regression of liver fibrosis presumed by repeated biomarkers after virological cure in patients with chronic hepatitis C. J Hepatol. 2013;59:675-83.
PubMed Abstract»Reig M, Mariño Z, Perelló C, et al. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J Hepatol. 2016;65:719-726.
PubMed Abstract»Saxena V, Nyberg L, Pauly M, et al. Safety and Efficacy of Simeprevir/Sofosbuvir in Hepatitis C-Infected Patients With Compensated and Decompensated Cirrhosis. Hepatology. 2015;62:715-25.
PubMed Abstract»Saxena V, Terrault N. Current Management of hepatitis C virus: regimens for peri-liver transplant patients. Clin Liver Dis. 2015;19:669-88.
PubMed Abstract»Shiratori Y, Imazeki F, Moriyama M, et al. Histologic improvement of fibrosis in patients with hepatitis C who have sustained response to interferon therapy. Ann Intern Med. 2000;132:517-24.
PubMed Abstract»Shiratori Y, Ito Y, Yokosuka O, et al. Antiviral therapy for cirrhotic hepatitis C: association with reduced hepatocellular carcinoma development and improved survival. Ann Intern Med. 2005;142:105-14.
PubMed Abstract»Simmons B, Saleem J, Heath K, Cooke GS, Hill A. Long-Term Treatment Outcomes of Patients Infected With Hepatitis C Virus: A Systematic Review and Meta-analysis of the Survival Benefit of Achieving a Sustained Virological Response. Clin Infect Dis. 2015;61:730-40.
PubMed Abstract»Singal AG, Volk ML, Jensen D, Di Bisceglie AM, Schoenfeld PS. A sustained viral response is associated with reduced liver-related morbidity and mortality in patients with hepatitis C virus. Clin Gastroenterol Hepatol. 2010;8:280-8.
PubMed Abstract»Singh S, Facciorusso A, Loomba R, Falck-Ytter YT. Magnitude and Kinetics of Decrease in Liver Stiffness After Antiviral Therapy in Patients With Chronic Hepatitis C: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2018;16:27-38.e4.
PubMed Abstract»Solomon SS, Wagner-Cardoso S, Smeaton L, et al. A minimal monitoring approach for the treatment of hepatitis C virus infection (ACTG A5360 [MINMON]): a phase 4, open-label, single-arm trial. Lancet Gastroenterol Hepatol. 2022;7:307-17.
PubMed Abstract»Tada T, Kumada T, Toyoda H, et al. Viral eradication reduces all-cause mortality, including non-liver-related disease, in patients with progressive hepatitis C virus-related fibrosis. J Gastroenterol Hepatol. 2017;32:687-694.
PubMed Abstract»Terrault NA, Zeuzem S, Di Bisceglie AM, et al. Effectiveness of Ledipasvir-Sofosbuvir Combination in Patients With Hepatitis C Virus Infection and Factors Associated With Sustained Virologic Response. Gastroenterology. 2016;151:1131-1140.e5.
PubMed Abstract»Thomas RM, Brems JJ, Guzman-Hartman G, Yong S, Cavaliere P, Van Thiel DH. Infection with chronic hepatitis C virus and liver transplantation: a role for interferon therapy before transplantation. Liver Transpl. 2003;9:905-15.
PubMed Abstract»van der Meer AJ, Veldt BJ, Feld JJ, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012;308:2584-93.
PubMed Abstract»Vierling JM, Zeuzem S, Poordad F, et al. Safety and efficacy of boceprevir/peginterferon/ribavirin for HCV G1 compensated cirrhotics: Meta-analysis of 5 trials. J Hepatol. 2014;61:200-9.
PubMed Abstract»Waziry R, Hajarizadeh B, Grebely J, et al. Hepatocellular carcinoma risk following direct-acting antiviral HCV therapy: A systematic review, meta-analyses, and meta-regression. J Hepatol. 2017;67:1204-1212.
PubMed Abstract»Welzel TM, Petersen J, Herzer K, et al. Daclatasvir plus sofosbuvir, with or without ribavirin, achieved high sustained virological response rates in patients with HCV infection and advanced liver disease in a real-world cohort. Gut. 2016;65:1861-1870.
PubMed Abstract»Wiesner R, Edwards E, Freeman R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91-6.
PubMed Abstract»Yoshida H, Arakawa Y, Sata M, et al. Interferon therapy prolonged life expectancy among chronic hepatitis C patients. Gastroenterology. 2002;123:483-91.
PubMed Abstract»Zeuzem S, Dusheiko GM, Salupere R, et al. Sofosbuvir and ribavirin in HCV genotypes 2 and 3. N Engl J Med. 2014;370:1993-2001.
PubMed Abstract»Zeuzem S, Ghalib R, Reddy KR, et al. Grazoprevir-Elbasvir Combination Therapy for Treatment-Naive Cirrhotic and Noncirrhotic Patients With Chronic Hepatitis C Virus Genotype 1, 4, or 6 Infection: A Randomized Trial. Ann Intern Med. 2015;163:1-13.
PubMed Abstract»Lesson 5. Treatment of Acute HCV Infection
Background
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: management of acute HCV infection.
AASLD-IDSA Hepatitis C Guidance»Centers for Disease Control and Prevention (CDC). 2019 Viral Hepatitis Surveillance Report—Hepatitis C. Published May 2021.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Centers for Disease Control and Prevention (CDC). Sexual transmission of hepatitis C virus among HIV-infected men who have sex with men--New York City, 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60:945-50.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Viral Hepatitis Statistics and Surveillance—United States, 2016.
CDC Viral Hepatitis Surveillance»Grady BP, Schinkel J, Thomas XV, Dalgard O. Hepatitis C virus reinfection following treatment among people who use drugs. Clin Infect Dis. 2013;57 Suppl 2:S105-10.
PubMed Abstract»Grebely J, Matthews GV, Dore GJ. Treatment of acute HCV infection. Nat Rev Gastroenterol Hepatol. 2011;8:265-74.
PubMed Abstract»Hajarizadeh B, Grebely J, Dore GJ. Case definitions for acute hepatitis C virus infection: A systematic review. J Hepatol. 2012;57:1349-60.
PubMed Abstract»Ragonnet R, Deuffic-Burban S, Boesecke C, et al. Estimating the Time to Diagnosis and the Chance of Spontaneous Clearance During Acute Hepatitis C in Human Immunodeficiency Virus-Infected Individuals. Open Forum Infect Dis. 2017 Winter;4:ofw235.
PubMed Abstract»Ryerson AB, Schillie S, Barker LK, Kupronis BA, Wester C. Vital Signs: Newly Reported Acute and Chronic Hepatitis C Cases - United States, 2009-2018. MMWR Morb Mortal Wkly Rep. 2020;69:399-404.
PubMed Abstract»Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of Late Relapse or Reinfection With Hepatitis C Virus After Achieving a Sustained Virological Response: A Systematic Review and Meta-analysis. Clin Infect Dis. 2016;62:683-694.
PubMed Abstract»Williams IT, Bell BP, Kuhnert W, Alter MJ. Incidence and transmission patterns of acute hepatitis C in the United States, 1982-2006. Arch Intern Med. 2011;171:242-8.
PubMed Abstract»Witt MD, Seaberg EC, Darilay A, et al. Incident hepatitis C virus infection in men who have sex with men: a prospective cohort analysis, 1984-2011. Clin Infect Dis. 2013;57:77-84.
PubMed Abstract»Young J, Rossi C, Gill J, et al. Risk Factors for Hepatitis C Virus Reinfection After Sustained Virologic Response in Patients Coinfected With HIV. Clin Infect Dis. 2017;64:1154-1162.
PubMed Abstract»Zibbell JE, Hart-Malloy R, Barry J, Fan L, Flanigan C. Risk factors for HCV infection among young adults in rural New York who inject prescription opioid analgesics. Am J Public Health. 2014;104:2226-32.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»Spontaneous Clearance of HCV Following Acute Infection
Aisyah DN, Shallcross L, Hully AJ, O'Brien A, Hayward A. Assessing hepatitis C spontaneous clearance and understanding associated factors-A systematic review and meta-analysis. J Viral Hepat. 2018;25:680-698.
PubMed Abstract»Gerlach JT, Diepolder HM, Zachoval R, et al. Acute hepatitis C: high rate of both spontaneous and treatment-induced viral clearance. Gastroenterology. 2003;125:80-8.
PubMed Abstract»Grebely J, Page K, Sacks-Davis R, et al. The effects of female sex, viral genotype, and IL28B genotype on spontaneous clearance of acute hepatitis C virus infection. Hepatology. 2014;59:109-20.
PubMed Abstract»Grebely J, Petoumenos K, Hellard M, et al. Potential role for interleukin-28B genotype in treatment decision-making in recent hepatitis C virus infection. Hepatology. 2010;52:1216-24.
PubMed Abstract»Grebely J, Prins M, Hellard M, et al. Hepatitis C virus clearance, reinfection, and persistence, with insights from studies of injecting drug users: towards a vaccine. Lancet Infect Dis. 2012;12:408-14.
PubMed Abstract»Hofer H, Watkins-Riedel T, Janata O, et al. Spontaneous viral clearance in patients with acute hepatitis C can be predicted by repeated measurements of serum viral load. Hepatology. 2003;37:60-4.
PubMed Abstract»Kamal SM. Acute hepatitis C: a systematic review. Am J Gastroenterol. 2008;103:1283-97.
PubMed Abstract»Maheshwari A, Ray S, Thuluvath PJ. Acute hepatitis C. Lancet. 2008;372(9635):321-32.
PubMed Abstract»Micallef JM, Kaldor JM, Dore GJ. Spontaneous viral clearance following acute hepatitis C infection: a systematic review of longitudinal studies. J Viral Hepat. 2006;13:34-41.
PubMed Abstract»Park JS, Wong J, Cohen H. Hepatitis C virus screening of high-risk patients in a community hospital emergency department: Retrospective review of patient characteristics and future implications. PLoS One. 2021;16:e0252976.
PubMed Abstract»Ragonnet R, Deuffic-Burban S, Boesecke C, et al. Estimating the Time to Diagnosis and the Chance of Spontaneous Clearance During Acute Hepatitis C in Human Immunodeficiency Virus-Infected Individuals. Open Forum Infect Dis. 2017 Winter;4:ofw235.
PubMed Abstract»Seaberg EC, Witt MD, Jacobson LP, et al. Differences in hepatitis C virus prevalence and clearance by mode of acquisition among men who have sex with men. J Viral Hepat. 2013;21:696-705.
PubMed Abstract»Seo S, Silverberg MJ, Hurley LB, et al. Prevalence of Spontaneous Clearance of Hepatitis C Virus Infection Doubled From 1998 to 2017. Clin Gastroenterol Hepatol. 2020;18:511-3.
PubMed Abstract»Thomson EC, Fleming VM, Main J, et al. Predicting spontaneous clearance of acute hepatitis C virus in a large cohort of HIV-1-infected men. Gut. 2010;60:837-45.
PubMed Abstract»Acute HCV Treatment Data
Boerekamps A, De Weggheleire A, van den Berk GE, et al. Treatment of acute hepatitis C genotypes 1 and 4 with 8 weeks of grazoprevir plus elbasvir (DAHHS2): an open-label, multicentre, single-arm, phase 3b trial. Lancet Gastroenterol Hepatol. 2019;4:269-277.
PubMed Abstract»Corey KE, Mendez-Navarro J, Gorospe EC, Zheng H, Chung RT. Early treatment improves outcomes in acute hepatitis C virus infection: a meta-analysis. J Viral Hepat. 2009;17:201-7.
PubMed Abstract»Corey KE, Ross AS, Wurcel A, et al. Outcomes and treatment of acute hepatitis C virus infection in a United States population. Clin Gastroenterol Hepatol. 2006;4:1278-82.
PubMed Abstract»De Rosa FG, Bargiacchi O, Audagnotto S, et al. Twelve-week treatment of acute hepatitis C virus with pegylated interferon- alpha -2b in injection drug users. Clin Infect Dis. 2007;45:583-8.
PubMed Abstract»Delwaide J, Bourgeois N, Gerard C, et al. Treatment of acute hepatitis C with interferon alpha-2b: early initiation of treatment is the most effective predictive factor of sustained viral response. Aliment Pharmacol Ther. 2004;20:15-22.
PubMed Abstract»Deterding K, Grüner N, Buggisch P, et al. Delayed versus immediate treatment for patients with acute hepatitis C: a randomised controlled non-inferiority trial. Lancet Infect Dis. 2013;13:497-506.
PubMed Abstract»Deterding K, Spinner CD, Schott E, et al. Ledipasvir plus sofosbuvir fixed-dose combination for 6 weeks in patients with acute hepatitis C virus genotype 1 monoinfection (HepNet Acute HCV IV): an open-label, single-arm, phase 2 study. Lancet Infect Dis. 2017;17:215-22.
PubMed Abstract»Dore GJ, Hellard M, Matthews GV, et al. Effective treatment of injecting drug users with recently acquired hepatitis C virus infection. Gastroenterology. 2009;138:123-35.e1-2.
PubMed Abstract»European AIDS Treatment Network (NEAT) Acute Hepatitis C Infection Consensus Panel. Acute hepatitis C in HIV-infected individuals: recommendations from the European AIDS Treatment Network (NEAT) consensus conference. AIDS. 2011;25:399-409.
EASL»Fabrizi F, Dixit V, Messa P, Martin P. Interferon therapy of acute hepatitis C in dialysis patients: meta-analysis. J Viral Hepat. 2012;19:784-91.
PubMed Abstract»Fierer DS, Dieterich DT, Mullen MP, et al. Telaprevir in the treatment of acute hepatitis C virus infection in HIV-infected men. Clin Infect Dis. 2014;58:873-9.
PubMed Abstract»Gerlach JT, Diepolder HM, Zachoval R, et al. Acute hepatitis C: high rate of both spontaneous and treatment-induced viral clearance. Gastroenterology. 2003;125:80-8.
PubMed Abstract»Hullegie SJ, Claassen MA, van den Berk GE, et al. Boceprevir, peginterferon and ribavirin for acute hepatitis C in HIV infected patients. J Hepatol. 2016;64:807-12.
PubMed Abstract»Hwang SJ, Lee SD, Chan CY, Lu RH, Lo KJ. A randomized controlled trial of recombinant interferon alpha-2b in the treatment of Chinese patients with acute post-transfusion hepatitis C. J Hepatol. 1994;21:831-6.
PubMed Abstract»Jaeckel E, Cornberg M, Wedemeyer H, et al. Treatment of acute hepatitis C with interferon alfa-2b. N Engl J Med. 2001;345:1452-7.
PubMed Abstract»Kamal SM, Fouly AE, Kamel RR, et al. Peginterferon alfa-2b therapy in acute hepatitis C: impact of onset of therapy on sustained virologic response. Gastroenterology. 2006;130:632-8.
PubMed Abstract»Kamal SM, Ismail A, Graham CS, et al. Pegylated interferon alpha therapy in acute hepatitis C: relation to hepatitis C virus-specific T cell response kinetics. Hepatology. 2004;39:1721-31.
PubMed Abstract»Kamal SM, Moustafa KN, Chen J, et al. Duration of peginterferon therapy in acute hepatitis C: a randomized trial. Hepatology. 2006;43:923-31.
PubMed Abstract»Lampertico P, Rumi M, Romeo R, et al. A multicenter randomized controlled trial of recombinant interferon-alpha 2b in patients with acute transfusion-associated hepatitis C. Hepatology. 1994;19:19-22.
PubMed Abstract»Licata A, Di Bona D, Schepis F, Shahied L, Craxi A, Camma C. When and how to treat acute hepatitis C? J Hepatol. 2003;39:1056-62.
PubMed Abstract»Maasoumy B, Ingiliz P, Spinner CD, et al. Sofosbuvir plus velpatasvir for 8 weeks in patients with acute hepatitis C: The HepNet acute HCV-V study. JHEP Rep. 2023;5:100650.
PubMed Abstract»Martinello M, Bhagani S, Gane E, et al. Shortened therapy of eight weeks with paritaprevir/ritonavir/ombitasvir and dasabuvir is highly effective in people with recent HCV genotype 1 infection. J Viral Hepat. 2018;25:1180-8.
PubMed Abstract»Martinello M, Bhagani S, Shaw D, et al. TARGET3D: Glecaprevir-pibrentasvir for 4 weeks in people with recent HCV infection. In: Program and abstracts of the 30th Conference on Retroviruses and Opportunistic Infections; February 19-22, 2023; Seattle, WA. Abstract Number 194.
CROI»Martinello M, Gane E, Hellard M, et al. Sofosbuvir and ribavirin for 6 weeks is not effective among people with recent hepatitis C virus infection: The DARE-C II study. Hepatology. 2016;64:1911-1921.
PubMed Abstract»Martinello M, Orkin C, Cooke G, et al. Short-Duration Pan-Genotypic Therapy With Glecaprevir/Pibrentasvir for 6 Weeks Among People With Recent Hepatitis C Viral Infection. Hepatology. 2020;72:7-18.
PubMed Abstract»Matthews GV, Bhagani S, Van der Valk M, et al. Sofosbuvir/velpatasvir for 12 vs. 6 weeks for the treatment of recently acquired hepatitis C infection. J Hepatol. 2021;75:829-839.
PubMed Abstract»Micallef JM, Kaldor JM, Dore GJ. Spontaneous viral clearance following acute hepatitis C infection: a systematic review of longitudinal studies. J Viral Hepat. 2006;13:34-41.
PubMed Abstract»Naggie S, Fierer DS, Hughes MD, et al. Ledipasvir/Sofosbuvir for 8 Weeks to Treat Acute Hepatitis C Virus Infections in Men With Human Immunodeficiency Virus Infections: Sofosbuvir-Containing Regimens Without Interferon for Treatment of Acute HCV in HIV-1 Infected Individuals. Clin Infect Dis. 2019;69:514-522.
PubMed Abstract»Naggie S, Marks KM, Hughes M, et al. Sofosbuvir Plus Ribavirin Without Interferon for Treatment of Acute Hepatitis C Virus Infection in HIV-1-Infected Individuals: SWIFT-C. Clin Infect Dis. 2017;64:1035-1042.
PubMed Abstract»Nomura H, Sou S, Tanimoto H, et al. Short-term interferon-alfa therapy for acute hepatitis C: a randomized controlled trial. Hepatology. 2004;39:1213-9.
PubMed Abstract»Palaniswami PM, El Sayed A, Asriel B, Carollo JR, Fierer DS. Ledipasvir and Sofosbuvir in the Treatment of Early Hepatitis C Virus Infection in HIV-Infected Men. Open Forum Infect Dis. 2018;5:ofy238.
PubMed Abstract»Rocca P, Bailly F, Chevallier M, Chevallier P, Zoulim F, Trépo C. [Early treatment of acute hepatitis C with interferon alpha-2b or interferon alpha-2b plus ribavirin: study of sixteen patients]. Gastroenterol Clin Biol. 2003;27:294-9.
PubMed Abstract»Rockstroh JK, Bhagani S, Hyland RH, et al. Ledipasvir-sofosbuvir for 6 weeks to treat acute hepatitis C virus genotype 1 or 4 infection in patients with HIV coinfection: an open-label, single-arm trial. Lancet Gastroenterol Hepatol. 2017;2:347-353.
PubMed Abstract»Santantonio T, Fasano M, Sinisi E, Guastadisegni A, Casalino C, Mazzola M, Francavilla R, Pastore G. Efficacy of a 24-week course of PEG-interferon alpha-2b monotherapy in patients with acute hepatitis C after failure of spontaneous clearance. J Hepatol. 2005;42:329-33.
PubMed Abstract»Vogel W, Graziadei I, Umlauft F, et al. High-dose interferon-alpha2b treatment prevents chronicity in acute hepatitis C: a pilot study. Dig Dis Sci. 1996;41:81S-85S.
PubMed Abstract»Wiegand J, Buggisch P, Boecher W, et al. Early monotherapy with pegylated interferon alpha-2b for acute hepatitis C infection: the HEP-NET acute-HCV-II study. Hepatology. 2006;43:250-6.
PubMed Abstract»AASLD-IDSA Guidance for Management of Acute HCV
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: management of acute HCV infection.
AASLD-IDSA Hepatitis C Guidance»Asselah T, Marcellin P, Schinazi RF. Treatment of hepatitis C virus infection with direct-acting antiviral agents: 100% cure? Liver Int. 2018;38 Suppl 1:7-13.
PubMed Abstract»Fabrizi F, Dixit V, Messa P, Martin P. Interferon therapy of acute hepatitis C in dialysis patients: meta-analysis. J Viral Hepat. 2012;19:784-91.
PubMed Abstract»Jaeckel E, Cornberg M, Wedemeyer H, et al. Treatment of acute hepatitis C with interferon alfa-2b. N Engl J Med. 2001;345:1452-7.
PubMed Abstract»Kamal SM, Fouly AE, Kamel RR, et al. Peginterferon alfa-2b therapy in acute hepatitis C: impact of onset of therapy on sustained virologic response. Gastroenterology. 2006;130:632-8.
PubMed Abstract»Marcellin F, Roux P, Protopopescu C, Duracinsky M, Spire B, Carrieri MP. Patient-reported outcomes with direct-acting antivirals for the treatment of chronic hepatitis C: current knowledge and outstanding issues. Expert Rev Gastroenterol Hepatol. 2017;11:259-268.
PubMed Abstract»Aisyah DN, Shallcross L, Hully AJ, O'Brien A, Hayward A. Assessing hepatitis C spontaneous clearance and understanding associated factors-A systematic review and meta-analysis. J Viral Hepat. 2018;25:680-698.
PubMed Abstract»Asher A, Lum PJ, Page K. Assessing candidacy for acute hepatitis C treatment among active young injection drug users: a case-series report. J Assoc Nurses AIDS Care. 2011;23:16-29.
PubMed Abstract»Asselah T, Marcellin P, Schinazi RF. Treatment of hepatitis C virus infection with direct-acting antiviral agents: 100% cure? Liver Int. 2018;38 Suppl 1:7-13.
PubMed Abstract»Bethea ED, Chen Q, Hur C, Chung RT, Chhatwal J. Should we treat acute hepatitis C? A decision and cost-effectiveness analysis. Hepatology. 2018;67:837-846.
PubMed Abstract»Broers B, Helbling B, Francois A, et al. Barriers to interferon-alpha therapy are higher in intravenous drug users than in other patients with acute hepatitis C. J Hepatol. 2005;42:323-8.
PubMed Abstract»Brunet L, Moodie EE, Rollet K, et al. Marijuana smoking does not accelerate progression of liver disease in HIV-hepatitis C coinfection: A longitudinal cohort analysis. Clin Infect Dis. 2013;57:663-70.
PubMed Abstract»Calleri G, Colombatto P, Gozzelino M, et al. Natural beta interferon in acute type-C hepatitis patients: a randomized controlled trial. Ital J Gastroenterol Hepatol. 1998;30:181-4.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). 2019 Viral Hepatitis Surveillance Report—Hepatitis C. Published May 2021.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Centers for Disease Control and Prevention (CDC). Sexual transmission of hepatitis C virus among HIV-infected men who have sex with men--New York City, 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60:945-50.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Viral Hepatitis Statistics and Surveillance—United States, 2016.
CDC Viral Hepatitis Surveillance»El Sayed A, Barbati ZR, Turner SS, et al. Sofosbuvir in the treatment of early HCV infection in HIV-infected men. HIV Clin Trials. 2017;18:60-66.
PubMed Abstract»El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142:1264-1273.e1.
PubMed Abstract»Fabrizi F, Dixit V, Messa P, Martin P. Interferon therapy of acute hepatitis C in dialysis patients: meta-analysis. J Viral Hepat. 2012;19:784-91.
PubMed Abstract»Gerlach JT, Diepolder HM, Zachoval R, et al. Acute hepatitis C: high rate of both spontaneous and treatment-induced viral clearance. Gastroenterology. 2003;125:80-8.
PubMed Abstract»Grady BP, Schinkel J, Thomas XV, Dalgard O. Hepatitis C virus reinfection following treatment among people who use drugs. Clin Infect Dis. 2013;57 Suppl 2:S105-10.
PubMed Abstract»Grebely J, Matthews GV, Dore GJ. Treatment of acute HCV infection. Nat Rev Gastroenterol Hepatol. 2011;8:265-74.
PubMed Abstract»Grebely J, Page K, Sacks-Davis R, et al. The effects of female sex, viral genotype, and IL28B genotype on spontaneous clearance of acute hepatitis C virus infection. Hepatology. 2014;59:109-20.
PubMed Abstract»Grebely J, Petoumenos K, Hellard M, et al. Potential role for interleukin-28B genotype in treatment decision-making in recent hepatitis C virus infection. Hepatology. 2010;52:1216-24.
PubMed Abstract»Hézode C, Lonjon I, Roudot-Thoraval F, Mavier JP, Pawlotsky JM, Zafrani ES, Dhumeaux D. Impact of smoking on histological liver lesions in chronic hepatitis C. Gut. 2003;52:126-9.
PubMed Abstract»Hajarizadeh B, Grebely J, Dore GJ. Case definitions for acute hepatitis C virus infection: A systematic review. J Hepatol. 2012;57:1349-60.
PubMed Abstract»Hofer H, Watkins-Riedel T, Janata O, et al. Spontaneous viral clearance in patients with acute hepatitis C can be predicted by repeated measurements of serum viral load. Hepatology. 2003;37:60-4.
PubMed Abstract»Ishida JH, Peters MG, Jin C, Louie K, Tan V, Bacchetti P, Terrault NA. Influence of cannabis use on severity of hepatitis C disease. Clin Gastroenterol Hepatol. 2008;6:69-75.
PubMed Abstract»Jacobson IM, Lawitz E, Kwo PY, et al. Safety and Efficacy of Elbasvir/Grazoprevir in Patients With Hepatitis C Virus Infection and Compensated Cirrhosis: An Integrated Analysis. Gastroenterology. 2017;152:1372-1382.e2.
PubMed Abstract»Jin F, Matthews GV, Grulich AE. Sexual transmission of hepatitis C virus among gay and bisexual men: a systematic review. Sex Health. 2017;14:28-41.
PubMed Abstract»Kamal SM. Acute hepatitis C: a systematic review. Am J Gastroenterol. 2008;103:1283-97.
PubMed Abstract»Maheshwari A, Ray S, Thuluvath PJ. Acute hepatitis C. Lancet. 2008;372(9635):321-32.
PubMed Abstract»Maheshwari A, Thuluvath PJ. Management of acute hepatitis C. Clin Liver Dis. 2010;14:169-76.
PubMed Abstract»Marcellin F, Roux P, Protopopescu C, Duracinsky M, Spire B, Carrieri MP. Patient-reported outcomes with direct-acting antivirals for the treatment of chronic hepatitis C: current knowledge and outstanding issues. Expert Rev Gastroenterol Hepatol. 2017;11:259-268.
PubMed Abstract»Micallef JM, Kaldor JM, Dore GJ. Spontaneous viral clearance following acute hepatitis C infection: a systematic review of longitudinal studies. J Viral Hepat. 2006;13:34-41.
PubMed Abstract»Nunnari G, Montineri A, Portelli V, Savalli F, Fatuzzo F, Cacopardo B. The use of peginterferon in monotherapy or in combination with ribavirin for the treatment of acute hepatitis C. Eur Rev Med Pharmacol Sci. 2012;16:1013-6.
PubMed Abstract»Pol S, Parlati L. Treatment of hepatitis C: the use of the new pangenotypic direct-acting antivirals in "special populations". Liver Int. 2018;38 Suppl 1:28-33.
PubMed Abstract»Purohit V, Rapaka R, Shurtleff D. Role of cannabinoids in the development of fatty liver (steatosis). The AAPS journal. 2010;12:233-7.
PubMed Abstract»Ryerson AB, Schillie S, Barker LK, Kupronis BA, Wester C. Vital Signs: Newly Reported Acute and Chronic Hepatitis C Cases - United States, 2009-2018. MMWR Morb Mortal Wkly Rep. 2020;69:399-404.
PubMed Abstract»Seo S, Silverberg MJ, Hurley LB, et al. Prevalence of Spontaneous Clearance of Hepatitis C Virus Infection Doubled From 1998 to 2017. Clin Gastroenterol Hepatol. 2020;18:511-3.
PubMed Abstract»Sharma SA, Feld JJ. Acute hepatitis C: management in the rapidly evolving world of HCV. Curr Gastroenterol Rep. 2014;16:371.
PubMed Abstract»Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of Late Relapse or Reinfection With Hepatitis C Virus After Achieving a Sustained Virological Response: A Systematic Review and Meta-analysis. Clin Infect Dis. 2016;62:683-694.
PubMed Abstract»Sulkowski MS. Management of acute and chronic HCV infection in persons with HIV coinfection. J Hepatol. 2014;61:S108-S119.
PubMed Abstract»Sylvestre DL, Clements BJ, Malibu Y. Cannabis use improves retention and virological outcomes in patients treated for hepatitis C. Eur J Gastroenterol Hepatol. 2006;18:1057-63.
PubMed Abstract»Wiegand J, Jackel E, Cornberg M, et al. Long-term follow-up after successful interferon therapy of acute hepatitis C. Hepatology 2004;40:98-107.
PubMed Abstract»Williams IT, Bell BP, Kuhnert W, Alter MJ. Incidence and transmission patterns of acute hepatitis C in the United States, 1982-2006. Arch Intern Med. 2011;171:242-8.
PubMed Abstract»Young J, Rossi C, Gill J, et al. Risk Factors for Hepatitis C Virus Reinfection After Sustained Virologic Response in Patients Coinfected With HIV. Clin Infect Dis. 2017;64:1154-1162.
PubMed Abstract»Zibbell JE, Hart-Malloy R, Barry J, Fan L, Flanigan C. Risk factors for HCV infection among young adults in rural New York who inject prescription opioid analgesics. Am J Public Health. 2014;104:2226-32.
PubMed Abstract»Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64:453-8.
PubMed Abstract»Zimmermann T, Hueppe D, Mauss S, et al. Effects of Smoking on Pegylated Interferon alpha 2a and First Generation Protease Inhibitor-based Antiviral Therapy in Naïve Patients Infected with Hepatitis C Virus Genotype 1. J Gastrointestin Liver Dis. 2016;25:15-24.
PubMed Abstract»Module 6. Treatment of Key Populations and Unique Situations
Lesson 1. Treatment of HCV in Persons with HIV Coinfection
Background of HIV-HCV Coinfection
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with HIV/HCV coinfection.
AASLD-IDSA Hepatitis C Guidance»Berenguer J, González-García J, López-Aldeguer J, et al. Pegylated interferon {alpha}2a plus ribavirin versus pegylated interferon {alpha}2b plus ribavirin for the treatment of chronic hepatitis C in HIV-infected patients. J Antimicrob Chemother. 2009;63:1256-63.
PubMed Abstract»Bosh KA, Coyle JR, Hansen V, et al. HIV and viral hepatitis coinfection analysis using surveillance data from 15 US states and two cities. Epidemiol Infect. 2018;146:920-930.
PubMed Abstract»Cachay ER, Hill L, Wyles D, et al. The hepatitis C cascade of care among HIV infected patients: a call to address ongoing barriers to care. PLoS One. 2014;9:e102883.
PubMed Abstract»Carrat F, Bani-Sadr F, Pol S, et al. Pegylated interferon alfa-2b vs standard interferon alfa-2b, plus ribavirin, for chronic hepatitis C in HIV-infected patients: a randomized controlled trial. JAMA. 2004;292:2839-48.
PubMed Abstract»Chung RT, Andersen J, Volberding P, et al. Peginterferon Alfa-2a plus ribavirin versus interferon alfa-2a plus ribavirin for chronic hepatitis C in HIV-coinfected persons. N Engl J Med. 2004;351:451-9.
PubMed Abstract»Crowell TA, Berry SA, Fleishman JA, et al. Impact of hepatitis coinfection on healthcare utilization among persons living with HIV. J Acquir Immune Defic Syndr. 2015;68:425-31.
PubMed Abstract»Di Martino V, Rufat P, Boyer N, et al. The influence of human immunodeficiency virus coinfection on chronic hepatitis C in injection drug users: a long-term retrospective cohort study. Hepatology. 2001;34:1193-9.
PubMed Abstract»Dieterich D, Rockstroh JK, Orkin C, et al. Simeprevir (TMC435) with pegylated interferon/ribavirin in patients coinfected with HCV genotype 1 and HIV-1: a phase 3 study. Clin Infect Dis. 2014;59:1579-87.
PubMed Abstract»European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C: Final update of the series☆. J Hepatol. 2020:S0168-8278(20)30548-1.
EASL»Graham CS, Baden LR, Yu E, Mrus JM, Carnie J, Heeren T, Koziel MJ. Influence of human immunodeficiency virus infection on the course of hepatitis C virus infection: a meta-analysis. Clin Infect Dis. 2001;33:562-9.
PubMed Abstract»Joshi D, O'Grady J, Dieterich D, Gazzard B, Agarwal K. Increasing burden of liver disease in patients with HIV infection. Lancet. 2011;377:1198-209.
PubMed Abstract»Kim AY, Onofrey S, Church DR. An epidemiologic update on hepatitis C infection in persons living with or at risk of HIV infection. J Infect Dis. 2013;207 Suppl 1:S1-6.
PubMed Abstract»Kirk GD, Mehta SH, Astemborski J, et al. HIV, age, and the severity of hepatitis C virus-related liver disease: a cohort study. Ann Intern Med. 2013;158:658-66.
PubMed Abstract»Laguno M, Cifuentes C, Murillas J, et al. Randomized trial comparing pegylated interferon alpha-2b versus pegylated interferon alpha-2a, both plus ribavirin, to treat chronic hepatitis C in human immunodeficiency virus patients. Hepatology. 2009;49:22-31.
PubMed Abstract»Laguno M, Murillas J, Blanco JL, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for treatment of HIV/HCV co-infected patients. AIDS. 2004;18:F27-36.
PubMed Abstract»Lo Re V 3rd, Kallan MJ, Tate JP, et al. Hepatic decompensation in antiretroviral-treated patients co-infected with HIV and hepatitis C virus compared with hepatitis C virus-monoinfected patients: a cohort study. Ann Intern Med. 2014;160:369-79.
PubMed Abstract»Martel-Laferrière V, Brinkley S, Bichoupan K, et al. Virological response rates for telaprevir-based hepatitis C triple therapy in patients with and without HIV coinfection. HIV Med. 2013;15:108-15.
PubMed Abstract»Núñez M, Miralles C, Berdún MA, et al. Role of weight-based ribavirin dosing and extended duration of therapy in chronic hepatitis C in HIV-infected patients: the PRESCO trial. AIDS Res Hum Retroviruses. 2007;23:972-82.
PubMed Abstract»Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Hepatitis C virus. Last Updated: January 18, 2023.
HIV.gov»Platt L, Easterbrook P, Gower E, et al. Prevalence and burden of HCV co-infection in people living with HIV: a global systematic review and meta-analysis. Lancet Infect Dis. 2016;16:797-808.
PubMed Abstract»Rockstroh JK, Spengler U. HIV and hepatitis C virus co-infection. Lancet Infect Dis. 2004;4:437-44.
PubMed Abstract»Rosenthal E, Roussillon C, Salmon-Céron D, et al. Liver-related deaths in HIV-infected patients between 1995 and 2010 in France: the Mortavic 2010 study in collaboration with the Agence Nationale de Recherche sur le SIDA (ANRS) EN 20 Mortalité 2010 survey. HIV Med. 2015;16:230-9.
PubMed Abstract»Sherman KE, Rouster SD, Chung RT, Rajicic N. Hepatitis C Virus prevalence among patients infected with Human Immunodeficiency Virus: a cross-sectional analysis of the US adult AIDS Clinical Trials Group. Clin Infect Dis. 2002;34:831-7.
PubMed Abstract»Sulkowski M, Pol S, Mallolas J, et al. Boceprevir versus placebo with pegylated interferon alfa-2b and ribavirin for treatment of hepatitis C virus genotype 1 in patients with HIV: a randomised, double-blind, controlled phase 2 trial. Lancet Infect Dis. 2013;13:597-605.
PubMed Abstract»Sulkowski MS, Poordad F, Manns MP, et al. Anemia during treatment with peginterferon Alfa-2b/ribavirin and boceprevir: Analysis from the serine protease inhibitor therapy 2 (SPRINT-2) trial. Hepatology. 2013;57:974-84.
PubMed Abstract»Sulkowski MS, Sherman KE, Dieterich DT, et al. Combination therapy with telaprevir for chronic hepatitis C virus genotype 1 infection in patients with HIV: a randomized trial. Ann Intern Med. 2013;159:86-96.
PubMed Abstract»Thomas DL. The challenge of hepatitis C in the HIV-infected person. Annu Rev Med. 2008;59:473-85.
PubMed Abstract»Torriani FJ, Rodriguez-Torres M, Rockstroh JK, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection in HIV-infected patients. N Engl J Med. 2004;351:438-50.
PubMed Abstract»HCV Treatment Data in Persons with HIV Coinfection
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with HIV/HCV coinfection.
AASLD-IDSA Hepatitis C Guidance»Berenguer J, González-García J, López-Aldeguer J, et al. Pegylated interferon {alpha}2a plus ribavirin versus pegylated interferon {alpha}2b plus ribavirin for the treatment of chronic hepatitis C in HIV-infected patients. J Antimicrob Chemother. 2009;63:1256-63.
PubMed Abstract»Bhattacharya D, Belperio PS, Shahoumian TA, et al. Effectiveness of All-Oral Antiviral Regimens in 996 Human Immunodeficiency Virus/Hepatitis C Virus Genotype 1-Coinfected Patients Treated in Routine Practice. Clin Infect Dis. 2017;64:1711-1720.
PubMed Abstract»Carrat F, Bani-Sadr F, Pol S, et al. Pegylated interferon alfa-2b vs standard interferon alfa-2b, plus ribavirin, for chronic hepatitis C in HIV-infected patients: a randomized controlled trial. JAMA. 2004;292:2839-48.
PubMed Abstract»Chung RT, Andersen J, Volberding P, et al. Peginterferon Alfa-2a plus ribavirin versus interferon alfa-2a plus ribavirin for chronic hepatitis C in HIV-coinfected persons. N Engl J Med. 2004;351:451-9.
PubMed Abstract»Dieterich D, Nelson M, Soriano V, et al. Faldaprevir and pegylated interferon α-2a/ribavirin in individuals co-infected with hepatitis C virus genotype-1 and HIV. AIDS. 2015;29:571-81.
PubMed Abstract»Dieterich D, Rockstroh JK, Orkin C, et al. Simeprevir (TMC435) with pegylated interferon/ribavirin in patients coinfected with HCV genotype 1 and HIV-1: a phase 3 study. Clin Infect Dis. 2014;59:1579-87.
PubMed Abstract»Kim HN, Nance RM, Williams-Nguyen JS, et al. Effectiveness of Direct-Acting Antiviral Therapy in Patients With Human Immunodeficiency Virus-Hepatitis C Virus Coinfection in Routine Clinical Care: A Multicenter Study. Open Forum Infect Dis. 2019;6:ofz100.
PubMed Abstract»Laguno M, Murillas J, Blanco JL, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for treatment of HIV/HCV co-infected patients. AIDS. 2004;18:F27-36.
PubMed Abstract»Molina JM, Orkin C, Iser DM, et al. Sofosbuvir plus ribavirin for treatment of hepatitis C virus in patients co-infected with HIV (PHOTON-2): a multicentre, open-label, non-randomised, phase 3 study. Lancet. 2015;385:1098-106.
PubMed Abstract»Naggie S, Cooper C, Saag M, et al. Ledipasvir and sofosbuvir for HCV in patients coinfected with HIV-1. N Engl J Med. 2015;373:705-13.
PubMed Abstract»Osinusi A, Meissner EG, Lee YJ, et al. Sofosbuvir and ribavirin for hepatitis C genotype 1 in patients with unfavorable treatment characteristics: a randomized clinical trial. JAMA. 2013;310:804-11.
PubMed Abstract»Osinusi A, Townsend K, Kohli A, et al. Virologic response following combined ledipasvir and sofosbuvir administration in patients with HCV genotype 1 and HIV co-infection. JAMA. 2015;313:1232-9.
PubMed Abstract»Patel M, Rab S, Kalapila AG, Kyle A, Okosun IS, Miller L. Highly Successful Hepatitis C Virus (HCV) Treatment Outcomes in Human Immunodeficiency Virus/HCV-Coinfected Patients at a Large, Urban, Ryan White Clinic. Open Forum Infect Dis. 2017;4:ofx062.
PubMed Abstract»Piroth L, Paniez H, Taburet AM, et al. High Cure Rate With 24 Weeks of Daclatasvir-Based Quadruple Therapy in Treatment-Experienced, Null-Responder Patients With HIV/Hepatitis C Virus Genotype 1/4 Coinfection: The ANRS HC30 QUADRIH Study. Clin Infect Dis. 2015;61:817-25.
PubMed Abstract»Rockstroh JK, Lacombe K, Viani RM, et al. Efficacy and Safety of Glecaprevir/Pibrentasvir in Patients Coinfected With Hepatitis C Virus and Human Immunodeficiency Virus Type 1: The EXPEDITION-2 Study. Clin Infect Dis. 2018;67:1010-17.
PubMed Abstract»Rockstroh JK, Nelson M, Katlama C, et al. Efficacy and safety of grazoprevir (MK-5172) and elbasvir (MK-8742) in patients with hepatitis C virus and HIV co-infection (C-EDGE CO-INFECTION): a non-randomised, open-label trial. Lancet HIV. 2015;2:e319-27.
PubMed Abstract»Rodriguez-Torres M, Gaggar A, Shen G, et al. Sofosbuvir for chronic hepatitis C virus infection genotype 1-4 in patients coinfected with HIV. J Acquir Immune Defic Syndr. 2015;68:543-9.
PubMed Abstract»Sogni P, Gilbert C, Lacombe K, et al. All-oral Direct-acting Antiviral Regimens in HIV/Hepatitis C Virus-coinfected Patients With Cirrhosis Are Efficient and Safe: Real-life Results From the Prospective ANRS CO13-HEPAVIH Cohort. Clin Infect Dis. 2016;63:763-770.
PubMed Abstract»Sulkowski M, Pol S, Mallolas J, et al. Boceprevir versus placebo with pegylated interferon alfa-2b and ribavirin for treatment of hepatitis C virus genotype 1 in patients with HIV: a randomised, double-blind, controlled phase 2 trial. Lancet Infect Dis. 2013;13:597-605.
PubMed Abstract»Sulkowski MS, Eron JJ, Wyles D, et al. Ombitasvir, paritaprevir co-dosed with ritonavir, dasabuvir, and ribavirin for hepatitis C in patients co-infected with HIV-1: a randomized trial. JAMA. 2015;313:1223-31.
PubMed Abstract»Sulkowski MS, Naggie S, Lalezari J, et al. Sofosbuvir and ribavirin for hepatitis C in patients with HIV coinfection. JAMA. 2014;312:353-61.
PubMed Abstract»Sulkowski MS, Sherman KE, Dieterich DT, et al. Combination therapy with telaprevir for chronic hepatitis C virus genotype 1 infection in patients with HIV: a randomized trial. Ann Intern Med. 2013;159:86-96.
PubMed Abstract»Torriani FJ, Rodriguez-Torres M, Rockstroh JK, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection in HIV-infected patients. N Engl J Med. 2004;351:438-50.
PubMed Abstract»Wilson E, Covert E, Hoffmann J, et al. A pilot study of safety and efficacy of HCV retreatment with sofosbuvir/velpatasvir/voxilaprevir in patients with or without HIV (RESOLVE STUDY). J Hepatol. 2019;71:498-504.
PubMed Abstract»Wyles D, Bräu N, Kottilil S, et al. Sofosbuvir and Velpatasvir for the Treatment of Hepatitis C Virus in Patients Coinfected With Human Immunodeficiency Virus Type 1: An Open-Label, Phase 3 Study. Clin Infect Dis. 2017;65:6-12.
PubMed Abstract»Wyles DL, Ruane PJ, Sulkowski MS, et al. Daclatasvir plus sofosbuvir for HCV in patients coinfected with HIV-1. N Engl J Med. 2015;373:714-25.
PubMed Abstract»Treatment of HCV in Persons with HIV Coinfection
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection: treatment-naive genotype 2 with compensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection: treatment-naive genotype 1a with compensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection: treatment-naive genotype 1a without cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection: treatment-naive genotype 1b with compensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection: treatment-naive genotype 1b without cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection: treatment-naive genotype 3 with compensated cirrhosis
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection: treatment-naive genotype 4 with compensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection: treatment-naive genotype 5 or 6.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with HIV/HCV coinfection.
AASLD-IDSA Hepatitis C Guidance»Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»Bhattacharya D, Belperio PS, Shahoumian TA, et al. Effectiveness of All-Oral Antiviral Regimens in 996 Human Immunodeficiency Virus/Hepatitis C Virus Genotype 1-Coinfected Patients Treated in Routine Practice. Clin Infect Dis. 2017;64:1711-1720.
PubMed Abstract»Brown RS Jr, Buti M, Rodrigues L, et al. Glecaprevir/pibrentasvir for 8 weeks in treatment-naïve patients with chronic HCV genotypes 1-6 and compensated cirrhosis: The EXPEDITION-8 trial. J Hepatol. 2020;72:441-9.
PubMed Abstract»Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Considerations for antiretroviral use in patients with coinfections: hepatitis C (HCV)/HIV coinfection. September 21, 2022.
HIV.gov»Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Hepatitis C virus. Last Updated: January 18, 2023.
HIV.gov»Treatment of HIV in Persons with HCV Coinfection
Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Considerations for antiretroviral use in patients with coinfections: hepatitis C (HCV)/HIV coinfection. September 21, 2022.
HIV.gov»Drug Interactions with HIV-HCV Coinfection Treatment
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with HIV/HCV coinfection.
AASLD-IDSA Hepatitis C Guidance»Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»Kosloski MP, Oberoi R, Wang S, et al. Drug-Drug Interactions of Glecaprevir and Pibrentasvir Coadministered With Human Immunodeficiency Virus Antiretrovirals. J Infect Dis. 2020;221:223-31.
PubMed Abstract»Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Considerations for antiretroviral use in patients with coinfections: hepatitis C (HCV)/HIV coinfection. September 21, 2022.
HIV.gov»Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Drug-drug interactions: drug interactions between integrase inhibitors and other drugs. December 18, 2019.
HIV.gov»Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Drug-drug interactions: drug interactions between non-nucleoside reverse transcriptase inhibitors and other drugs. December 18, 2019
HIV.gov»Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Drug-drug interactions: drug interactions between nucleoside reverse transcriptase inhibitors and other drugs (including antiretroviral agents). December 18, 2019.
HIV.gov»Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Drug-drug interactions: drug interactions between protease inhibitors and other drugs. December 18, 2019.
HIV.gov»Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Hepatitis C virus. Last Updated: January 18, 2023.
HIV.gov»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection: treatment-naive genotype 4 with compensated cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy has failed: peginterferon plus ribavirin-experienced, genotype 4 patients without cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Retreatment of persons in whom prior therapy has failed: peginterferon plus ribavirin-experienced, genotype 5 or 6 patients with or without compensated cirrhosis
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults With Compensated Cirrhosis.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Simplified HCV Treatment for Treatment-Naive Adults Without Cirrhosis.
[AASLD-IDSA Hepatitis C Guidance»Asselah T, Kowdley KV, Zadeikis N, et al. Efficacy of Glecaprevir/Pibrentasvir for 8 or 12 Weeks in Patients With Hepatitis C Virus Genotype 2, 4, 5, or 6 Infection Without Cirrhosis. Clin Gastroenterol Hepatol. 2018;16:417-26.
PubMed Abstract»Asselah T, Reesink HW, Gerstoft J, et al. High Efficacy of Elbasvir and Grazoprevir with or Without Ribavirin in 103 Treatment-Naive and Experienced Patients with HCV Genotype 4 infection: A Pooled Analysis. Presented at the 66th Annual Meeting of the American Association for the Study of Liver Diseases. San Francisco, CA. November 13-17, 2015. Abstract 251.
NATAP»Bhattacharya D, Aronsohn A, Price J, Lo Re V. Hepatitis C Guidance 2023 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2023 May 25;ciad319.
PubMed Abstract»Bichoupan K, Dieterich DT, Martel-Laferrière V. HIV-hepatitis C virus co-infection in the era of direct-acting antivirals. Curr HIV/AIDS Rep. 2014;11:241-9.
PubMed Abstract»Brown RS Jr, Buti M, Rodrigues L, et al. Glecaprevir/pibrentasvir for 8 weeks in treatment-naïve patients with chronic HCV genotypes 1-6 and compensated cirrhosis: The EXPEDITION-8 trial. J Hepatol. 2020;72:441-9.
PubMed Abstract»Di Martino V, Rufat P, Boyer N, et al. The influence of human immunodeficiency virus coinfection on chronic hepatitis C in injection drug users: a long-term retrospective cohort study. Hepatology. 2001;34:1193-9.
PubMed Abstract»European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C: Final update of the series☆. J Hepatol. 2020:S0168-8278(20)30548-1.
EASL»Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599-607.
PubMed Abstract»Forns X, Lee SS, Valdes J, et al. Glecaprevir plus pibrentasvir for chronic hepatitis C virus genotype 1, 2, 4, 5, or 6 infection in adults with compensated cirrhosis (EXPEDITION-1): a single-arm, open-label, multicentre phase 3 trial. Lancet Infect Dis. 2017;17:1062-1068.
PubMed Abstract»Graham CS, Baden LR, Yu E, Mrus JM, Carnie J, Heeren T, Koziel MJ. Influence of human immunodeficiency virus infection on the course of hepatitis C virus infection: a meta-analysis. Clin Infect Dis. 2001;33:562-9.
PubMed Abstract»Hézode C, Asselah T, Reddy KR, et al. Ombitasvir plus paritaprevir plus ritonavir with or without ribavirin in treatment-naive and treatment-experienced patients with genotype 4 chronic hepatitis C virus infection (PEARL-I): a randomised, open-label trial. Lancet. 2015;385:2502-9.
PubMed Abstract»Hagan LM, Sulkowski MS, Schinazi RF. Cost analysis of sofosbuvir/ribavirin versus sofosbuvir/simeprevir for genotype 1 hepatitis C virus in interferon-ineligible/intolerant individuals. Hepatology. 2014;60:37-45.
PubMed Abstract»Hasan F, Al-Khaldi J, Asker H, et al. Peginterferon alpha-2b plus ribavirin with or without amantadine [correction of amantidine] for the treatment of non-responders to standard interferon and ribavirin. Antivir Ther. 2004;9:499-503.
PubMed Abstract»Kim AY, Onofrey S, Church DR. An epidemiologic update on hepatitis C infection in persons living with or at risk of HIV infection. J Infect Dis. 2013;207 Suppl 1:S1-6.
PubMed Abstract»Kohli A, Kapoor R, Sims Z, et al. Ledipasvir and sofosbuvir for hepatitis C genotype 4: a proof-of-concept, single-centre, open-label phase 2a cohort study. Lancet Infect Dis. 2015;15:1049-54.
PubMed Abstract»Kwo PY, Poordad F, Asatryan A, et al. Glecaprevir and pibrentasvir yield high response rates in patients with HCV genotype 1-6 without cirrhosis. J Hepatol. 2017;67:263-271.
PubMed Abstract»Moreno C, Hezode C, Marcellin P, et al. Efficacy and safety of simeprevir with PegIFN/ribavirin in naïve or experienced patients infected with chronic HCV genotype 4. J Hepatol. 2015;62:1047-55.
PubMed Abstract»Ruane PJ, Ain D, Stryker R, et al. Sofosbuvir plus ribavirin for the treatment of chronic genotype 4 hepatitis C virus infection in patients of Egyptian ancestry. J Hepatol. 2015;62:1040-6.
PubMed Abstract»Sulkowski M, Hezode C, Gerstoft J, et al. Efficacy and safety of 8 weeks versus 12 weeks of treatment with grazoprevir (MK-5172) and elbasvir (MK-8742) with or without ribavirin in patients with hepatitis C virus genotype 1 mono-infection and HIV/hepatitis C virus co-infection (C-WORTHY): a randomised, open-label phase 2 trial. Lancet. 2015;385:1087-97.
PubMed Abstract»Wilson E, Covert E, Hoffmann J, et al. A pilot study of safety and efficacy of HCV retreatment with sofosbuvir/velpatasvir/voxilaprevir in patients with or without HIV (RESOLVE STUDY). J Hepatol. 2019;71:498-504.
PubMed Abstract»Lesson 2. Treatment of HCV in Persons with Renal Impairment
Background
Awan AAY, Berenguer MC, Bruchfeld A, et al. Prevention, Diagnosis, Evaluation, and Treatment of Hepatitis C in Chronic Kidney Disease: Synopsis of the Kidney Disease: Improving Global Outcomes 2022 Clinical Practice Guideline. Ann Intern Med. 2023;176:1648-55.
PubMed Abstract»Botev R, Mallié JP, Couchoud C, et al. Estimating glomerular filtration rate: Cockcroft-Gault and Modification of Diet in Renal Disease formulas compared to renal inulin clearance. Clin J Am Soc Nephrol. 2009;4:899-906.
PubMed Abstract»Carbone M, Cockwell P, Neuberger J. Hepatitis C and kidney transplantation. Int J Nephrol. 2011;2011:593291.
PubMed Abstract»Carbone M, Mutimer D, Neuberger J. Hepatitis C virus and nonliver solid organ transplantation. Transplantation. 2013;95:779-86.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Recommendations for preventing transmission of infections among chronic hemodialysis patients. MMWR Recomm Rep. 2001;50:1-43.
PubMed Abstract»Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31-41.
PubMed Abstract»Covic A, Abramowicz D, Bruchfeld A, et al. Endorsement of the Kidney Disease Improving Global Outcomes (KDIGO) hepatitis C guidelines: a European Renal Best Practice (ERBP) position statement. Nephrol Dial Transplant. 2009;24:719-27.
PubMed Abstract»Fabrizi F, Takkouche B, Lunghi G, Dixit V, Messa P, Martin P. The impact of hepatitis C virus infection on survival in dialysis patients: meta-analysis of observational studies. J Viral Hepat. 2007;14:697-703.
PubMed Abstract»Finelli L, Miller JT, Tokars JI, Alter MJ, Arduino MJ. National surveillance of dialysis-associated diseases in the United States, 2002. Semin Dial. 2005;18:52-61.
PubMed Abstract»Fissell RB, Bragg-Gresham JL, Woods JD, et al. Patterns of hepatitis C prevalence and seroconversion in hemodialysis units from three continents: the DOPPS. Kidney Int. 2004;65:2335-42.
PubMed Abstract»Ghany MG, Strader DB, Thomas DL, Seeff LB; American Association for the Study of Liver Diseases. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335-74.
AASLD Practice Guidelines»Gordon CE, Uhlig K, Lau J, Schmid CH, Levey AS, Wong JB. Interferon treatment in hemodialysis patients with chronic hepatitis C virus infection: a systematic review of the literature and meta-analysis of treatment efficacy and harms. Am J Kidney Dis. 2008;51:263-77.
PubMed Abstract»Gordon SC, Moonka D, Brown KA, et al. Risk for renal cell carcinoma in chronic hepatitis C infection. Cancer Epidemiol Biomarkers Prev. 2010;19:1066-73.
PubMed Abstract»Inker LA, Astor BC, Fox CH, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63:713-35.
PubMed Abstract»Jadoul M, Bieber BA, Martin P, et al. Prevalence, incidence, and risk factors for hepatitis C virus infection in hemodialysis patients. Kidney Int. 2019;95:939-47.
PubMed Abstract»Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2013:Suppl 3:1-150.
KDIGO»Lee JJ, Lin MY, Chang JS, et al. Hepatitis C virus infection increases risk of developing end-stage renal disease using competing risk analysis. PLoS One. 2014;9:e100790.
PubMed Abstract»Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461-70.
PubMed Abstract»Levey AS, Coresh J, Greene T, et al. Expressing the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem. 2007;53:766-72.
PubMed Abstract»Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247-54.
PubMed Abstract»Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604-12.
PubMed Abstract»Ma Y, Huang Z, Jian Z, Wei X. The association between hepatitis C virus infection and renal cell cancer, prostate cancer, and bladder cancer: a systematic review and meta-analysis. Sci Rep. 2021;11:10833.
PubMed Abstract»Muleta D, Kainer MA, Moore-Moravian L, et al. Notes from the Field: Hepatitis C Outbreak in a Dialysis Clinic--Tennessee, 2014. MMWR Morb Mortal Wkly Rep. 2016;64:1386-7.
PubMed Abstract»Nguyen DB, Gutowski J, Ghiselli M, et al. A Large Outbreak of Hepatitis C Virus Infections in a Hemodialysis Clinic. Infect Control Hosp Epidemiol. 2016;37:125-33.
PubMed Abstract»Okuda K, Hayashi H, Kobayashi S, Irie Y. Mode of hepatitis C infection not associated with blood transfusion among chronic hemodialysis patients. J Hepatol. 1995;23:28-31.
PubMed Abstract»Ozkok A, Yildiz A. Hepatitis C virus associated glomerulopathies. World J Gastroenterol. 2014;20:7544-54.
PubMed Abstract»Patel PR, Thompson ND, Kallen AJ, Arduino MJ. Epidemiology, surveillance, and prevention of hepatitis C virus infections in hemodialysis patients. Am J Kidney Dis. 2010;56:371-8.
PubMed Abstract»Peters L, Grint D, Lundgren JD, et al. Hepatitis C virus viremia increases the incidence of chronic kidney disease in HIV-infected patients. AIDS. 2012;26:1917-26.
PubMed Abstract»Saxena V, Terrault NA. Treatment of Hepatitis C Infection in Renal Transplant Recipients: The Long Wait Is Over. Am J Transplant. 2016;16:1345-7.
PubMed Abstract»Shoker A, Hossain MA, Koru-Sengul T, Raju DL, Cockcroft D. Performance of creatinine clearance equations on the original Cockcroft-Gault population. Clin Nephrol. 2006;66:89-97.
PubMed Abstract»Thomson PC, Williams C, Aitken C, et al. A case of hepatitis C virus transmission acquired through sharing a haemodialysis machine. NDT Plus. 2011;4:32-5.
PubMed Abstract»Tsui JI, Vittinghoff E, Shlipak MG, Bertenthal D, Inadomi J, Rodriguez RA, O'Hare AM. Association of hepatitis C seropositivity with increased risk for developing end-stage renal disease. Arch Intern Med. 2007;167:1271-6.
PubMed Abstract»Winter MA, Guhr KN, Berg GM. Impact of various body weights and serum creatinine concentrations on the bias and accuracy of the Cockcroft-Gault equation. Pharmacotherapy. 2012;32:604-12.
PubMed Abstract»Wreghitt TG. Blood-borne virus infections in dialysis units--a review. Rev Med Virol. 1999;9:101-9.
PubMed Abstract»HCV Treatment Studies in Persons with CKD
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with renal impairment.
AASLD-IDSA Hepatitis C Guidance»Borgia SM, Dearden J, Yoshida EM, et al. Sofosbuvir/velpatasvir for 12 weeks in hepatitis C virus-infected patients with end-stage renal disease undergoing dialysis. J Hepatol. 2019;71:660-665.
PubMed Abstract»Bruchfeld A, Roth D, Martin P, et al. Elbasvir plus grazoprevir in patients with hepatitis C virus infection and stage 4-5 chronic kidney disease: clinical, virological, and health-related quality-of-life outcomes from a phase 3, multicentre, randomised, double-blind, placebo-controlled trial. Lancet Gastroenterol Hepatol. 2017;2:585-94.
PubMed Abstract»Butt AA, Ren Y, Puenpatom A, Arduino JM, Kumar R, Abou-Samra AB. Effectiveness, treatment completion and safety of sofosbuvir/ledipasvir and paritaprevir/ritonavir/ombitasvir + dasabuvir in patients with chronic kidney disease: an ERCHIVES study. Aliment Pharmacol Ther. 2018;48:35-43.
PubMed Abstract»Desnoyer A, Pospai D, Lê MP, et al. Pharmacokinetics, safety and efficacy of a full dose sofosbuvir-based regimen given daily in hemodialysis patients with chronic hepatitis C. J Hepatol. 2016;65:40-47.
PubMed Abstract»Elbasha E, Greaves W, Roth D, Nwankwo C. Cost-effectiveness of elbasvir/grazoprevir use in treatment-naive and treatment-experienced patients with hepatitis C virus genotype 1 infection and chronic kidney disease in the United States. J Viral Hepat. 2017;24:268-279.
PubMed Abstract»Fabrizi F, Dixit V, Martin P, Messa P. Combined antiviral therapy of hepatitis C virus in dialysis patients: meta-analysis of clinical trials. J Viral Hepat. 2011;18:e263-9.
PubMed Abstract»Fabrizi F, Dixit V, Messa P, Martin P. Antiviral therapy (pegylated interferon and ribavirin) of hepatitis C in dialysis patients: meta-analysis of clinical studies. J Viral Hepat. 2014;21:681-9.
PubMed Abstract»Fabrizi F, Dixit V, Messa P, Martin P. Interferon therapy of acute hepatitis C in dialysis patients: meta-analysis. J Viral Hepat. 2012;19:784-91.
PubMed Abstract»Fabrizi F, Dixit V, Messa P, Martin P. Pegylated interferon monotherapy of chronic hepatitis C in dialysis patients: Meta-analysis of clinical trials. J Med Virol. 2010;82:768-75.
PubMed Abstract»Fabrizi F, Messa P, Martin P. Recent advances on hepatitis C virus in dialysis population. Kidney Blood Press Res. 2014;39:260-271.
PubMed Abstract»Fabrizi F, Messa P. Therapy of hepatitis C by direct-acting anti-virals: the end of HCV in dialysis population? Expert Rev Clin Pharmacol. 2015;8:785-93.
PubMed Abstract»Fabrizi F, Takkouche B, Lunghi G, Dixit V, Messa P, Martin P. The impact of hepatitis C virus infection on survival in dialysis patients: meta-analysis of observational studies. J Viral Hepat. 2007;14:697-703.
PubMed Abstract»Fabrizi F. Hepatitis C virus infection and dialysis: 2012 update. ISRN Nephrol. 2012;2013:159760.
PubMed Abstract»Gane E, Lawitz E, Pugatch D, et al. Glecaprevir and Pibrentasvir in Patients with HCV and Severe Renal Impairment. N Engl J Med. 2017;377:1448-55.
PubMed Abstract»Garimella T, Wang R, Luo WL, et al. Single-dose pharmacokinetics and safety of daclatasvir in subjects with renal function impairment. Antivir Ther. 2015;20:535-43.
PubMed Abstract»Gordon CE, Uhlig K, Lau J, Schmid CH, Levey AS, Wong JB. Interferon treatment in hemodialysis patients with chronic hepatitis C virus infection: a systematic review of the literature and meta-analysis of treatment efficacy and harms. Am J Kidney Dis. 2008;51:263-77.
PubMed Abstract»Gordon CE, Uhlig K, Schmid CH, Levey AS, Wong JB. Long-term viral negativity after interferon for chronic hepatitis C virus infection in hemodialysis. Clin J Am Soc Nephrol. 2011;6:2226-34.
PubMed Abstract»Gupta SK, Kantesaria B, Glue P. Pharmacokinetics, safety, and tolerability of ribavirin in hemodialysis-dependent patients. Eur J Clin Pharmacol. 2011;68:415-8.
PubMed Abstract»Kalyan Ram B, Frank C, Adam P, et al. Safety, efficacy and tolerability of half-dose sofosbuvir plus simeprevir in treatment of Hepatitis C in patients with end stage renal disease. J Hepatol. 2015;63:763-5.
PubMed Abstract»Kidney Disease Outcome Quality Initiative (KDOQI) Clinical Practice Guidelines. Hepatitis C Management in Kidney Transplantation.
KDOQI»Lawitz E, Flisiak R, Abunimeh M, et al. Efficacy and safety of glecaprevir/pibrentasvir in renally impaired patients with chronic HCV infection. Liver Int. 2020;40:1032-41.
PubMed Abstract»Liu CH, Huang CF, Liu CJ, et al. Pegylated interferon-α2a with or without low-dose ribavirin for treatment-naive patients with hepatitis C virus genotype 1 receiving hemodialysis: a randomized trial. Ann Intern Med. 2013;159:729-38.
PubMed Abstract»Liu CH, Liang CC, Lin JW, et al. Pegylated interferon alpha-2a versus standard interferon alpha-2a for treatment-naive dialysis patients with chronic hepatitis C: a randomised study. Gut. 2007;57:525-30.
PubMed Abstract»Liu CH, Liang CC, Liu CJ, et al. Pegylated interferon alfa-2a monotherapy for hemodialysis patients with acute hepatitis C. Clin Infect Dis. 2010;51:541-9.
PubMed Abstract»Liu CH, Liu CJ, Huang CF, et al. Peginterferon alfa-2a with or without low-dose ribavirin for treatment-naive patients with hepatitis C virus genotype 2 receiving haemodialysis: a randomised trial. Gut. 2015;64:303-11.
PubMed Abstract»Maruyama A, Partovi N, Yoshida EM, Erb SR, Azalgara VM, Hussaini T. A review of direct-acting antivirals for the treatment of hepatitis C in patients with advanced chronic kidney disease. Nephrol Dial Transplant. 2017;32:35-41.
PubMed Abstract»Mauss S, Hueppe D, Alshuth U. Renal impairment is frequent in chronic hepatitis C patients under triple therapy with telaprevir or boceprevir. Hepatology. 2013;59:46-8.
PubMed Abstract»Nazario HE, Ndungu M, Modi AA. Sofosbuvir and simeprevir in hepatitis C genotype 1-patients with end-stage renal disease on haemodialysis or GFR <30 ml/min. Liver Int. 2016;36:798-801.
PubMed Abstract»Pockros PJ, Reddy KR, Mantry PS, et al. Efficacy of Direct-Acting Antiviral Combination for Patients With Hepatitis C Virus Genotype 1 Infection and Severe Renal Impairment or End-Stage Renal Disease. Gastroenterology. 2016;150:1590-8.
PubMed Abstract»Roth D, Nelson DR, Bruchfeld A, et al. Grazoprevir plus elbasvir in treatment-naive and treatment-experienced patients with hepatitis C virus genotype 1 infection and stage 4-5 chronic kidney disease (the C-SURFER study): a combination phase 3 study. Lancet. 2015;386:1537-45.
PubMed Abstract»Russo MW, Goldsweig CD, Jacobson IM, Brown RS Jr. Interferon monotherapy for dialysis patients with chronic hepatitis C: an analysis of the literature on efficacy and safety. Am J Gastroenterol. 2003;98:1610-5.
PubMed Abstract»Saadoun D, Resche Rigon M, Thibault V, et al. Peg-IFNα/ribavirin/protease inhibitor combination in hepatitis C virus associated mixed cryoglobulinemia vasculitis: results at week 24. Ann Rheum Dis. 2013;73:831-7.
PubMed Abstract»Sawinski D, Kaur N, Ajeti A, et al. Successful Treatment of Hepatitis C in Renal Transplant Recipients With Direct-Acting Antiviral Agents. Am J Transplant. 2016;16:1588-95.
PubMed Abstract»Saxena V, Koraishy FM, Sise ME, et al. Safety and efficacy of sofosbuvir-containing regimens in hepatitis C-infected patients with impaired renal function. Liver Int. 2016;36:807-16.
PubMed Abstract»Tempestilli M, Lionetti R, D'Offizi G, et al. Increased plasma concentration of ribavirin as a result of renal dysfunction in hepatitis C virus patients treated with telaprevir. Hepatology. 2014;60:1109-10.
PubMed Abstract»Tseng PL, Chen TC, Chien YS, et al. Efficacy and safety of pegylated interferon alfa-2b and ribavirin combination therapy versus pegylated interferon monotherapy in hemodialysis patients: a comparison of 2 sequentially treated cohorts. Am J Kidney Dis. 2013;62:789-95.
PubMed Abstract»Wang KL, Xing HQ, Zhao H, et al. Efficacy and tolerability of low-dose interferon-α in hemodialysis patients with chronic hepatitis C virus infection. World J Gastroenterol. 2014;20:4071-5.
PubMed Abstract»HCV Treatment in Persons with CKD
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with renal impairment.
AASLD-IDSA Hepatitis C Guidance»Cox-North P, Hawkins KL, Rossiter ST, Hawley MN, Bhattacharya R, Landis CS. Sofosbuvir-based regimens for the treatment of chronic hepatitis C in severe renal dysfunction. Hepatol Commun. 2017;1:248-255.
PubMed Abstract»Desnoyer A, Pospai D, Lê MP, et al. Pharmacokinetics, safety and efficacy of a full dose sofosbuvir-based regimen given daily in hemodialysis patients with chronic hepatitis C. J Hepatol. 2016;65:40-47.
PubMed Abstract»Gupta SK, Pittenger AL, Swan SK, et al. Single-dose pharmacokinetics and safety of pegylated interferon-alpha2b in patients with chronic renal dysfunction. J Clin Pharmacol. 2002;42:1109-15.
PubMed Abstract»Kidney Disease Improving Global Outcomes (KDIGO) Guideline for the Prevention, Diagnosis, Evaluation and Treatment of Hepatitis C in Chronic Kidney Disease.
KDIGO»Maruyama A, Partovi N, Yoshida EM, Erb SR, Azalgara VM, Hussaini T. A review of direct-acting antivirals for the treatment of hepatitis C in patients with advanced chronic kidney disease. Nephrol Dial Transplant. 2017;32:35-41.
PubMed Abstract»Peginterferon alfa-2a (Pegasys) Full Prescribing Information
Hoffman-La Roche, Inc. and Genetech, Inc.»Rostaing L, Chatelut E, Payen JL, et al. Pharmacokinetics of alphaIFN-2b in chronic hepatitis C virus patients undergoing chronic hemodialysis or with normal renal function: clinical implications. J Am Soc Nephrol. 1998;9:2344-8.
PubMed Abstract»Saxena V, Koraishy FM, Sise ME, et al. Safety and efficacy of sofosbuvir-containing regimens in hepatitis C-infected patients with impaired renal function. Liver Int. 2016;36:807-16.
PubMed Abstract»Sperl J, Frankova S, Kreidlova M, Merta D, Tothova M, Spicak J. Combination of sofosbuvir and daclatasvir in the treatment of genotype 3 chronic hepatitis C virus infection in patients on maintenance hemodialysis. Ther Clin Risk Manag. 2017;13:733-738.
PubMed Abstract»Talal AH, LaFleur J, Hoop R, et al. Absolute and relative contraindications to pegylated-interferon or ribavirin in the US general patient population with chronic hepatitis C: results from a US database of over 45 000 HCV-infected, evaluated patients. Aliment Pharmacol Ther. 2013;37:473-81.
PubMed Abstract»Yee HS, Chang MF, Pocha C, et al. Update on the management and treatment of hepatitis C virus infection: recommendations from the Department of Veterans Affairs Hepatitis C Resource Center Program and the National Hepatitis C Program Office. Am J Gastroenterol. 2012;107:669-89.
PubMed Abstract»Treatment of HCV in Setting of Renal Transplantation
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: kidney transplant patients.
AASLD/IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with renal impairment.
AASLD-IDSA Hepatitis C Guidance»Aleyadeh W, Verna EC, Elbeshbeshy H, et al. Outcomes of early vs late treatment initiation in solid organ transplantation from hepatitis C virus nucleic acid test-positive donors to hepatitis C virus-uninfected recipients: Results from the HCV-TARGET study. Am J Transplant. 2023:S1600-6135(23)00796-7.
PubMed Abstract»Baid-Agrawal S, Pascual M, Moradpour D, Somasundaram R, Muche M. Hepatitis C virus infection and kidney transplantation in 2014: what's new? Am J Transplant. 2014;14:2206-20.
PubMed Abstract»Carbone M, Cockwell P, Neuberger J. Hepatitis C and kidney transplantation. Int J Nephrol. 2011;2011:593291.
PubMed Abstract»Colombo M, Aghemo A, Liu H, et al. Treatment With Ledipasvir-Sofosbuvir for 12 or 24 Weeks in Kidney Transplant Recipients With Chronic Hepatitis C Virus Genotype 1 or 4 Infection: A Randomized Trial. Ann Intern Med. 2017;166:109-117.
PubMed Abstract»Cruzado JM, Casanovas-Taltavull T, Torras J, Baliellas C, Gil-Vernet S, Grinyó JM. Pretransplant interferon prevents hepatitis C virus-associated glomerulonephritis in renal allografts by HCV-RNA clearance. Am J Transplant. 2003;3:357-60.
PubMed Abstract»Fabrizi F, Penatti A, Messa P, Martin P. Treatment of hepatitis C after kidney transplant: a pooled analysis of observational studies. J Med Virol. 2014;86:933-40.
PubMed Abstract»Gordon CE, Adam GP, Jadoul M, Martin P, Balk EM. Kidney Transplantation From Hepatitis C Virus-Infected Donors to Uninfected Recipients: A Systematic Review for the KDIGO 2022 Hepatitis C Clinical Practice Guideline Update. Am J Kidney Dis. 2023;82:410-18.
PubMed Abstract»Hussein NR, Saleem ZS. Successful Treatment of Hepatitis C Virus Genotype 4 in Renal Transplant Recipients With Direct-Acting Antiviral Agents. Am J Transplant. 2016;16:2237-8.
PubMed Abstract»Kamar N, Marion O, Rostaing L, et al. Efficacy and Safety of Sofosbuvir-Based Antiviral Therapy to Treat Hepatitis C Virus Infection After Kidney Transplantation. Am J Transplant. 2016;16:1474-9.
PubMed Abstract»Kidney Disease Improving Global Outcomes (KDIGO) Guideline for the Prevention, Diagnosis, Evaluation and Treatment of Hepatitis C in Chronic Kidney Disease.
KDIGO»Kidney Disease Outcome Quality Initiative (KDOQI) Clinical Practice Guidelines. Hepatitis C Management in Kidney Transplantation.
KDOQI»Mahmoud IM, Sobh MA, El-Habashi AF, et al. Interferon therapy in hemodialysis patients with chronic hepatitis C: study of tolerance, efficacy and post-transplantation course. Nephron Clin Pract. 2005;100:c133-9.
PubMed Abstract»Pereira BJ, Natov SN, Bouthot BA, et al. Effects of hepatitis C infection and renal transplantation on survival in end-stage renal disease. The New England Organ Bank Hepatitis C Study Group. Kidney Int. 1998;53:1374-81.
PubMed Abstract»Reau N, Kwo PY, Rhee S, et al. Glecaprevir/Pibrentasvir Treatment in Liver or Kidney Transplant Patients With Hepatitis C Virus Infection. Hepatology. 2018;68:1298-1307.
PubMed Abstract»Rendina M, Schena A, Castellaneta NM, et al. The treatment of chronic hepatitis C with peginterferon alfa-2a (40 kDa) plus ribavirin in haemodialysed patients awaiting renal transplant. J Hepatol. 2007;46:768-74.
PubMed Abstract»Sawinski D, Kaur N, Ajeti A, et al. Successful Treatment of Hepatitis C in Renal Transplant Recipients With Direct-Acting Antiviral Agents. Am J Transplant. 2016;16:1588-95.
PubMed Abstract»Saxena V, Khungar V, Verna EC, et al. Safety and efficacy of current direct-acting antiviral regimens in kidney and liver transplant recipients with hepatitis C: Results from the HCV-TARGET study. Hepatology. 2017;66:1090-1101.
PubMed Abstract»Saxena V, Terrault NA. Treatment of Hepatitis C Infection in Renal Transplant Recipients: The Long Wait Is Over. Am J Transplant. 2016;16:1345-7.
PubMed Abstract»Sise ME, Goldberg DS, Schaubel DE, et al. One-Year Outcomes of the Multi-Center StudY to Transplant Hepatitis C-InfeCted kidneys (MYTHIC) Trial. Kidney Int Rep. 2022;7:241-50.
PubMed Abstract»Terrault NA, Adey DB. The kidney transplant recipient with hepatitis C infection: pre- and posttransplantation treatment. Clin J Am Soc Nephrol. 2007;2:563-75.
PubMed Abstract»Wei F, Liu J, Liu F, Hu H, Ren H, Hu P. Interferon-based anti-viral therapy for hepatitis C virus infection after renal transplantation: an updated meta-analysis. PLoS One. 2014;9:e90611.
PubMed Abstract»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: patients with renal impairment.
AASLD-IDSA Hepatitis C Guidance»Awan AAY, Berenguer MC, Bruchfeld A, et al. Prevention, Diagnosis, Evaluation, and Treatment of Hepatitis C in Chronic Kidney Disease: Synopsis of the Kidney Disease: Improving Global Outcomes 2022 Clinical Practice Guideline. Ann Intern Med. 2023;176:1648-55.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Recommendations for preventing transmission of infections among chronic hemodialysis patients. MMWR Recomm Rep. 2001;50:1-43.
PubMed Abstract»Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31-41.
PubMed Abstract»Fabrizi F, Messa P. Therapy of hepatitis C by direct-acting anti-virals: the end of HCV in dialysis population? Expert Rev Clin Pharmacol. 2015;8:785-93.
PubMed Abstract»Fabrizi F, Takkouche B, Lunghi G, Dixit V, Messa P, Martin P. The impact of hepatitis C virus infection on survival in dialysis patients: meta-analysis of observational studies. J Viral Hepat. 2007;14:697-703.
PubMed Abstract»Finelli L, Miller JT, Tokars JI, Alter MJ, Arduino MJ. National surveillance of dialysis-associated diseases in the United States, 2002. Semin Dial. 2005;18:52-61.
PubMed Abstract»Gane E, Lawitz E, Pugatch D, et al. Glecaprevir and Pibrentasvir in Patients with HCV and Severe Renal Impairment. N Engl J Med. 2017;377:1448-55.
PubMed Abstract»Gupta SK, Kantesaria B, Glue P. Pharmacokinetics, safety, and tolerability of ribavirin in hemodialysis-dependent patients. Eur J Clin Pharmacol. 2011;68:415-8.
PubMed Abstract»Kaya S, Aksoz S, Baysal B, Ay N, Danis R. Evaluation of telaprevir-containing triple therapy in the treatment of chronic hepatitis C in hemodialysed patients. Infect Dis (Lond). 2015;:1-4.
PubMed Abstract»Kidney Disease Improving Global Outcomes (KDIGO) Guideline for the Prevention, Diagnosis, Evaluation and Treatment of Hepatitis C in Chronic Kidney Disease.
KDIGO»Kidney Disease Outcome Quality Initiative (KDOQI) Clinical Practice Guidelines. Hepatitis C Management in Kidney Transplantation.
KDOQI»Kosloski MP, Zhao W, Marbury TC, et al. Effects of Renal Impairment and Hemodialysis on the Pharmacokinetics and Safety of the Glecaprevir and Pibrentasvir Combination in Hepatitis C Virus-Negative Subjects. Antimicrob Agents Chemother. 2018;62:e01990-17.
PubMed Abstract»Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247-54.
PubMed Abstract»Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604-12.
PubMed Abstract»Maruyama A, Partovi N, Yoshida EM, Erb SR, Azalgara VM, Hussaini T. A review of direct-acting antivirals for the treatment of hepatitis C in patients with advanced chronic kidney disease. Nephrol Dial Transplant. 2017;32:35-41.
PubMed Abstract»Muleta D, Kainer MA, Moore-Moravian L, et al. Notes from the Field: Hepatitis C Outbreak in a Dialysis Clinic--Tennessee, 2014. MMWR Morb Mortal Wkly Rep. 2016;64:1386-7.
PubMed Abstract»Nguyen DB, Gutowski J, Ghiselli M, et al. A Large Outbreak of Hepatitis C Virus Infections in a Hemodialysis Clinic. Infect Control Hosp Epidemiol. 2016;37:125-33.
PubMed Abstract»Patel PR, Thompson ND, Kallen AJ, Arduino MJ. Epidemiology, surveillance, and prevention of hepatitis C virus infections in hemodialysis patients. Am J Kidney Dis. 2010;56:371-8.
PubMed Abstract»Peters L, Grint D, Lundgren JD, et al. Hepatitis C virus viremia increases the incidence of chronic kidney disease in HIV-infected patients. AIDS. 2012;26:1917-26.
PubMed Abstract»Pockros PJ, Reddy KR, Mantry PS, et al. Efficacy of Direct-Acting Antiviral Combination for Patients With Hepatitis C Virus Genotype 1 Infection and Severe Renal Impairment or End-Stage Renal Disease. Gastroenterology. 2016;150:1590-8.
PubMed Abstract»Roth D, Nelson DR, Bruchfeld A, et al. Grazoprevir plus elbasvir in treatment-naive and treatment-experienced patients with hepatitis C virus genotype 1 infection and stage 4-5 chronic kidney disease (the C-SURFER study): a combination phase 3 study. Lancet. 2015;386:1537-45.
PubMed Abstract»Sawinski D, Kaur N, Ajeti A, et al. Successful Treatment of Hepatitis C in Renal Transplant Recipients With Direct-Acting Antiviral Agents. Am J Transplant. 2016;16:1588-95.
PubMed Abstract»Tempestilli M, Lionetti R, D'Offizi G, et al. Increased plasma concentration of ribavirin as a result of renal dysfunction in hepatitis C virus patients treated with telaprevir. Hepatology. 2014;60:1109-10.
PubMed Abstract»Tsui JI, Vittinghoff E, Shlipak MG, Bertenthal D, Inadomi J, Rodriguez RA, O'Hare AM. Association of hepatitis C seropositivity with increased risk for developing end-stage renal disease. Arch Intern Med. 2007;167:1271-6.
PubMed Abstract»Lesson 3. Treatment of HCV in Persons with Substance Use
Background
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Aspinall EJ, Corson S, Doyle JS, et al. Treatment of hepatitis C virus infection among people who are actively injecting drugs: a systematic review and meta-analysis. Clin Infect Dis. 2013;57 Suppl 2:S80-9.
PubMed Abstract»Center for Behavioral Health Statistics and Quality (CBHSQ), Substance Abuse and Mental Health Services Administration (SAMHSA), and U.S. Department of Health and Human Services (HHS). Results from the 2015 National Survey on Drug Use and Health:Detailed Tables
SAMHSA»Durham DP, Skrip LA, Bruce RD, et al. The Impact of Enhanced Screening and Treatment on Hepatitis C in the United States. Clin Infect Dis. 2015;62:298-304.
PubMed Abstract»Grebely J, Robaeys G, Bruggmann P, et al. Recommendations for the management of hepatitis C virus infection among people who inject drugs. Int J Drug Policy. 2015;26:1028-38.
PubMed Abstract»Substance Abuse and Mental Health Services Administration (SAMHSA). (2019). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19-5068, NSDUH Series H-54). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration.
SAMHSA»Substance Abuse and Mental Health Services Administration (SAMHSA). (2022). Key substance use and mental health indicators in the United States: Results from the 2022 National Survey on Drug Use and Health (HHS Publication No. PEP23-07-01-006, NSDUH Series H-58). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration.
SAMHSA»Approach to HCV Treatment in Persons with Substance Use
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Key populations: identification and management of HCV in people who inject drugs.
AASLD/IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Anand BS, Currie S, Dieperink E, et al. Alcohol use and treatment of hepatitis C virus: results of a national multicenter study. Gastroenterology. 2006;130:1607-16.
PubMed Abstract»Aspinall EJ, Corson S, Doyle JS, et al. Treatment of hepatitis C virus infection among people who are actively injecting drugs: a systematic review and meta-analysis. Clin Infect Dis. 2013;57 Suppl 2:S80-9.
PubMed Abstract»Backmund M, Meyer K, Von Zielonka M, Eichenlaub D. Treatment of hepatitis C infection in injection drug users. Hepatology. 2001;34:188-93.
PubMed Abstract»Bruggmann P, Dampz M, Gerlach T, Kravecz L, Falcato L. Treatment outcome in relation to alcohol consumption during hepatitis C therapy: an analysis of the Swiss Hepatitis C Cohort Study. Drug Alcohol Depend. 2010;110:167-71.
PubMed Abstract»Cachay ER, Wyles D, Hill L, et al. The Impact of Direct-Acting Antivirals in the Hepatitis C-Sustained Viral Response in Human Immunodeficiency Virus-Infected Patients With Ongoing Barriers to Care. Open Forum Infect Dis. 2015;2:ofv168.
PubMed Abstract»Dimova RB, Zeremski M, Jacobson IM, Hagan H, Des Jarlais DC, Talal AH. Determinants of hepatitis C virus treatment completion and efficacy in drug users assessed by meta-analysis. Clin Infect Dis. 2013;56:806-16.
PubMed Abstract»Dore GJ, Altice F, Litwin AH, et al. Elbasvir-Grazoprevir to Treat Hepatitis C Virus Infection in Persons Receiving Opioid Agonist Therapy: A Randomized Trial. Ann Intern Med. 2016;165:625-634.
PubMed Abstract»Durham DP, Skrip LA, Bruce RD, et al. The Impact of Enhanced Screening and Treatment on Hepatitis C in the United States. Clin Infect Dis. 2015;62:298-304.
PubMed Abstract»Foster GR, Dore GJ, Wang S, et al. Glecaprevir/pibrentasvir in patients with chronic HCV and recent drug use: An integrated analysis of 7 phase III studies. Drug Alcohol Depend. 2019;194:487-94.
PubMed Abstract»Gidding HF, Law MG, Amin J, et al. Hepatitis C treatment outcomes in Australian clinics. Med J Aust. 2012;196:633-7.
PubMed Abstract»Grebely J, Dalgard O, Conway B, et al. Sofosbuvir and velpatasvir for hepatitis C virus infection in people with recent injection drug use (SIMPLIFY): an open-label, single-arm, phase 4, multicentre trial. Lancet Gastroenterol Hepatol. 2018;3:153-61.
PubMed Abstract»Grebely J, Dore GJ, Alami NN, et al. Safety and efficacy of glecaprevir/pibrentasvir in patients with chronic hepatitis C genotypes 1-6 receiving opioid substitution therapy. Int J Drug Policy. 2019;66:73-9.
PubMed Abstract»Grebely J, Dore GJ, Zeuzem S, et al. Efficacy and Safety of Sofosbuvir/Velpatasvir in Patients With Chronic Hepatitis C Virus Infection Receiving Opioid Substitution Therapy: Analysis of Phase 3 ASTRAL Trials. Clin Infect Dis. 2016;63:1479-1481.
PubMed Abstract»Grebely J, Feld JJ, Wyles D, et al. Sofosbuvir-Based Direct-Acting Antiviral Therapies for HCV in People Receiving Opioid Substitution Therapy: An Analysis of Phase 3 Studies. Open Forum Infect Dis. 2018;5:ofy001.
PubMed Abstract»Grebely J, Hajarizadeh B, Dore GJ. Direct-acting antiviral agents for HCV infection affecting people who inject drugs. Nat Rev Gastroenterol Hepatol. 2017;14:641-651.
PubMed Abstract»Grebely J, Mauss S, Brown A, et al. Efficacy and Safety of Ledipasvir/Sofosbuvir With and Without Ribavirin in Patients With Chronic HCV Genotype 1 Infection Receiving Opioid Substitution Therapy: Analysis of Phase 3 ION Trials. Clin Infect Dis. 2016;63:1405-11.
PubMed Abstract»Grebely J, Raffa JD, Meagher C, et al. Directly observed therapy for the treatment of hepatitis C virus infection in current and former injection drug users. J Gastroenterol Hepatol. 2007;22:1519-25.
PubMed Abstract»Grebely J, Robaeys G, Bruggmann P, et al. Recommendations for the management of hepatitis C virus infection among people who inject drugs. Int J Drug Policy. 2015;26:1028-38.
PubMed Abstract»Hagan H, Pouget ER, Des Jarlais DC. A systematic review and meta-analysis of interventions to prevent hepatitis C virus infection in people who inject drugs. J Infect Dis. 2011;204:74-83.
PubMed Abstract»Hajarizadeh B, Cunningham EB, Reid H, Law M, Dore GJ, Grebely J. Direct-acting antiviral treatment for hepatitis C among people who use or inject drugs: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2018;3:754-67.
PubMed Abstract»Hellard M, Sacks-Davis R, Gold J. Hepatitis C treatment for injection drug users: a review of the available evidence. Clin Infect Dis. 2009;49:561-73.
PubMed Abstract»Le Lan C, Guillygomarc'h A, Danielou H, et al. A multi-disciplinary approach to treating hepatitis C with interferon and ribavirin in alcohol-dependent patients with ongoing abuse. J Hepatol. 2012;56:334-40.
PubMed Abstract»Litwin AH, Lum PJ, Taylor LE, et al. Patient-centred models of hepatitis C treatment for people who inject drugs: a multicentre, pragmatic randomised trial. Lancet Gastroenterol Hepatol. 2022;7:1112-27.
PubMed Abstract»Martin NK, Hickman M, Hutchinson SJ, Goldberg DJ, Vickerman P. Combination interventions to prevent HCV transmission among people who inject drugs: modeling the impact of antiviral treatment, needle and syringe programs, and opiate substitution therapy. Clin Infect Dis. 2013;57 Suppl 2:S39-45.
PubMed Abstract»Martin NK, Vickerman P, Grebely J, et al. Hepatitis C virus treatment for prevention among people who inject drugs: Modeling treatment scale-up in the age of direct-acting antivirals. Hepatology. 2013;58:1598-609.
PubMed Abstract»Martin NK, Vickerman P, Miners A, Foster GR, Hutchinson SJ, Goldberg DJ, Hickman M. Cost-effectiveness of hepatitis C virus antiviral treatment for injection drug user populations. Hepatology. 2012;55:49-57.
PubMed Abstract»Riley DE, Liu L, Cohen B, Robinson S, Groessl EJ, Ho SB. Characteristics and impact of methamphetamine use in patients with chronic hepatitis C. J Addict Med. 2014;8:25-32.
PubMed Abstract»Russell M, Pauly MP, Moore CD, et al. The impact of lifetime alcohol use on hepatitis C treatment outcomes in privately insured members of an integrated health care plan. Hepatology. 2012;56:1223-30.
PubMed Abstract»Seal KH, Currie SL, Shen H, et al. Hepatitis C treatment candidacy and outcomes among 4318 US veterans with chronic hepatitis C virus infection: does a history of injection drug use matter? J Clin Gastroenterol. 2007;41:199-205.
PubMed Abstract»Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of Late Relapse or Reinfection With Hepatitis C Virus After Achieving a Sustained Virological Response: A Systematic Review and Meta-analysis. Clin Infect Dis. 2016;62:683-94.
PubMed Abstract»Sylvestre DL, Litwin AH, Clements BJ, Gourevitch MN. The impact of barriers to hepatitis C virus treatment in recovering heroin users maintained on methadone. J Subst Abuse Treat. 2005;29:159-65.
PubMed Abstract»Tsui JI, Williams EC, Green PK, Berry K, Su F, Ioannou GN. Alcohol use and hepatitis C virus treatment outcomes among patients receiving direct antiviral agents. Drug Alcohol Depend. 2016;169:101-9.
PubMed Abstract»Ward Z, Platt L, Sweeney S, et al. Impact of current and scaled-up levels of hepatitis C prevention and treatment interventions for people who inject drugs in three UK settings-what is required to achieve the WHO's HCV elimination targets? Addiction. 2018. doi: 10.1111/add.14217.
PubMed Abstract»HCV Treatment in Persons with Opioid Use
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Key populations: identification and management of HCV in people who inject drugs.
AASLD/IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Akiyama MJ, Norton BL, Arnsten JH, Agyemang L, Heo M, Litwin AH. Intensive Models of Hepatitis C Care for People Who Inject Drugs Receiving Opioid Agonist Therapy: A Randomized Controlled Trial. Ann Intern Med. 2019;170:594-603.
PubMed Abstract»Brunet L, Moodie EE, Cox J, et al. Opioid use and risk of liver fibrosis in HIV/hepatitis C virus-coinfected patients in Canada. HIV Med. 2016;17:36-45.
PubMed Abstract»Butner JL, Gupta N, Fabian C, Henry S, Shi JM, Tetrault JM. Onsite treatment of HCV infection with direct acting antivirals within an opioid treatment program. J Subst Abuse Treat. 2017;75:49-53.
PubMed Abstract»Cachay ER, Wyles D, Hill L, et al. The Impact of Direct-Acting Antivirals in the Hepatitis C-Sustained Viral Response in Human Immunodeficiency Virus-Infected Patients With Ongoing Barriers to Care. Open Forum Infect Dis. 2015;2:ofv168.
PubMed Abstract»Coffin PO, Santos GM, Behar E, et al. Randomized feasibility trial of directly observed versus unobserved hepatitis C treatment with ledipasvir-sofosbuvir among people who inject drugs. PLoS One. 2019;14:e0217471.
PubMed Abstract»Compton WM, Jones CM, Baldwin GT. Relationship between Nonmedical Prescription-Opioid Use and Heroin Use. N Engl J Med. 2016;374:154-63.
PubMed Abstract»Dore GJ, Altice F, Litwin AH, et al. Elbasvir-Grazoprevir to Treat Hepatitis C Virus Infection in Persons Receiving Opioid Agonist Therapy: A Randomized Trial. Ann Intern Med. 2016;165:625-634.
PubMed Abstract»Durham DP, Skrip LA, Bruce RD, et al. The Impact of Enhanced Screening and Treatment on Hepatitis C in the United States. Clin Infect Dis. 2015;62:298-304.
PubMed Abstract»Eckhardt B, Mateu-Gelabert P, Aponte-Melendez Y, et al. Accessible Hepatitis C Care for People Who Inject Drugs: A Randomized Clinical Trial. JAMA Intern Med. 2022;182:494-502.
PubMed Abstract»Elsherif O, Bannan C, Keating S, McKiernan S, Bergin C, Norris S. Outcomes from a large 10 year hepatitis C treatment programme in people who inject drugs: No effect of recent or former injecting drug use on treatment adherence or therapeutic response. PLoS One. 2017;12:e0178398.
PubMed Abstract»Gonzalez-Serna A, Macias J, Corma-Gomez A, et al. High efficacy of glecaprevir/pibrentasvir for HCV-infected individuals with active drug use. J Infect. 2022;85:322-6.
PubMed Abstract»Grebely J, Dalgard O, Conway B, et al. Sofosbuvir and velpatasvir for hepatitis C virus infection in people with recent injection drug use (SIMPLIFY): an open-label, single-arm, phase 4, multicentre trial. Lancet Gastroenterol Hepatol. 2018;3:153-61.
PubMed Abstract»Grebely J, Dore GJ, Alami NN, et al. Safety and efficacy of glecaprevir/pibrentasvir in patients with chronic hepatitis C genotypes 1-6 receiving opioid substitution therapy. Int J Drug Policy. 2019;66:73-9.
PubMed Abstract»Grebely J, Dore GJ, Zeuzem S, et al. Efficacy and Safety of Sofosbuvir/Velpatasvir in Patients With Chronic Hepatitis C Virus Infection Receiving Opioid Substitution Therapy: Analysis of Phase 3 ASTRAL Trials. Clin Infect Dis. 2016;63:1479-1481.
PubMed Abstract»Grebely J, Feld JJ, Wyles D, et al. Sofosbuvir-Based Direct-Acting Antiviral Therapies for HCV in People Receiving Opioid Substitution Therapy: An Analysis of Phase 3 Studies. Open Forum Infect Dis. 2018;5:ofy001.
PubMed Abstract»Grebely J, Hajarizadeh B, Dore GJ. Direct-acting antiviral agents for HCV infection affecting people who inject drugs. Nat Rev Gastroenterol Hepatol. 2017;14:641-651.
PubMed Abstract»Grebely J, Matthews GV, Lloyd AR, Dore GJ. Elimination of hepatitis C virus infection among people who inject drugs through treatment as prevention: feasibility and future requirements. Clin Infect Dis. 2013;57:1014-20.
PubMed Abstract»Grebely J, Mauss S, Brown A, et al. Efficacy and Safety of Ledipasvir/Sofosbuvir With and Without Ribavirin in Patients With Chronic HCV Genotype 1 Infection Receiving Opioid Substitution Therapy: Analysis of Phase 3 ION Trials. Clin Infect Dis. 2016;63:1405-11.
PubMed Abstract»Grebely J, Raffa JD, Meagher C, et al. Directly observed therapy for the treatment of hepatitis C virus infection in current and former injection drug users. J Gastroenterol Hepatol. 2007;22:1519-25.
PubMed Abstract»Hajarizadeh B, Carson JM, Byrne M, et al. Incidence of hepatitis C virus infection in the prison setting: The SToP-C study. J Viral Hepat. 2024;31:21-34.
PubMed Abstract»Hajarizadeh B, Cunningham EB, Reid H, Law M, Dore GJ, Grebely J. Direct-acting antiviral treatment for hepatitis C among people who use or inject drugs: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2018;3:754-67.
PubMed Abstract»Hajarizadeh B, Cunningham EB, Valerio H, et al. Hepatitis C reinfection after successful antiviral treatment among people who inject drugs: A meta-analysis. J Hepatol. 2020;72:643-57.
PubMed Abstract»Hajarizadeh B, Grebely J, Byrne M, et al. Evaluation of hepatitis C treatment-as-prevention within Australian prisons (SToP-C): a prospective cohort study. Lancet Gastroenterol Hepatol. 2021;6:533-46.
PubMed Abstract»Huang CF, Dai CY, Wang CW, et al. Therapy as prevention toward HCV elimination in maintenance hemodialysis: a multi-center, prospective cohort study. Clin Kidney J. 2023;16:2429-36.
PubMed Abstract»Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers - United States, 2002-2004 and 2008-2010. Drug Alcohol Depend. 2013;132:95-100.
PubMed Abstract»Krook AL, Stokka D, Heger B, Nygaard E. Hepatitis C treatment of opioid dependants receiving maintenance treatment: results of a Norwegian pilot study. Eur Addict Res. 2007;13:216-21.
PubMed Abstract»Litwin AH, Lum PJ, Taylor LE, et al. Patient-centred models of hepatitis C treatment for people who inject drugs: a multicentre, pragmatic randomised trial. Lancet Gastroenterol Hepatol. 2022;7:1112-27.
PubMed Abstract»McCance-Katz EF, Sullivan LE, Nallani S. Drug interactions of clinical importance among the opioids, methadone and buprenorphine, and other frequently prescribed medications: a review. Am J Addict. 2010;19:4-16.
PubMed Abstract»Meemken L, Hanhoff N, Tseng A, Christensen S, Gillessen A. Drug-Drug Interactions With Antiviral Agents in People Who Inject Drugs Requiring Substitution Therapy. Ann Pharmacother. 2015;49:796-807.
PubMed Abstract»Munari SC, Traeger MW, Menon V, et al. Determining reinfection rates by hepatitis C testing interval among key populations: A systematic review and meta-analysis. Liver Int. 2023;43:2625-44.
PubMed Abstract»Olafsson S, Fridriksdottir RH, Love TJ, et al. Cascade of care during the first 36 months of the treatment as prevention for hepatitis C (TraP HepC) programme in Iceland: a population-based study. Lancet Gastroenterol Hepatol. 2021;6:628-37.
PubMed Abstract»Schwarz T, Horváth I, Fenz L, Schmutterer I, Rosian-Schikuta I, Mårdh O. Interventions to increase linkage to care and adherence to treatment for hepatitis C among people who inject drugs: A systematic review and practical considerations from an expert panel consultation. Int J Drug Policy. 2022;102:103588.
PubMed Abstract»Seal KH, Currie SL, Shen H, et al. Hepatitis C treatment candidacy and outcomes among 4318 US veterans with chronic hepatitis C virus infection: does a history of injection drug use matter? J Clin Gastroenterol. 2007;41:199-205.
PubMed Abstract»Seidenberg A, Rosemann T, Senn O. Patients receiving opioid maintenance treatment in primary care: successful chronic hepatitis C care in a real world setting. BMC Infect Dis. 2013;13:9.
PubMed Abstract»Tsui JI, Evans JL, Lum PJ, Hahn JA, Page K. Association of opioid agonist therapy with lower incidence of hepatitis C virus infection in young adult injection drug users. JAMA Intern Med. 2014;174:1974-81.
PubMed Abstract»Tsui JI, Williams EC, Green PK, Berry K, Su F, Ioannou GN. Alcohol use and hepatitis C virus treatment outcomes among patients receiving direct antiviral agents. Drug Alcohol Depend. 2016;169:101-9.
PubMed Abstract»HCV Treatment in Persons with Stimulant Use
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Key populations: identification and management of HCV in people who inject drugs.
AASLD/IDSA Hepatitis C Guidance»Caiaffa WT, Zocratto KF, Osimani ML, et al. Hepatitis C virus among non-injecting cocaine users (NICUs) in South America: can injectors be a bridge? Addiction. 2011;106:143-51.
PubMed Abstract»Chou C, Yimam KK, Frederick RT, Swenson SL. A Rare Case of Icteric Acute Hepatitis C Infection Acquired Through Intranasal Methamphetamine Use. ACG Case Rep J. 2014;1:112-4.
PubMed Abstract»Coffin PO, Santos GM, Das M, et al. Aripiprazole for the treatment of methamphetamine dependence: a randomized, double-blind, placebo-controlled trial. Addiction. 2013;108:751-61.
PubMed Abstract»Coffin PO, Santos GM, Hern J, et al. Effects of Mirtazapine for Methamphetamine Use Disorder Among Cisgender Men and Transgender Women Who Have Sex With Men: A Placebo-Controlled Randomized Clinical Trial. JAMA Psychiatry. 2020;77:246-55.
PubMed Abstract»Coffin PO, Santos GM, Hern J, et al. Extended-release naltrexone for methamphetamine dependence among men who have sex with men: a randomized placebo-controlled trial. Addiction. 2018;113:268-278.
PubMed Abstract»Colfax GN, Santos GM, Das M, et al. Mirtazapine to reduce methamphetamine use: a randomized controlled trial. Archives of general psychiatry. 2011;68:1168-75.
PubMed Abstract»Cunningham EB, Jacka B, DeBeck K, et al. Methamphetamine injecting is associated with phylogenetic clustering of hepatitis C virus infection among street-involved youth in Vancouver, Canada. Drug Alcohol Depend. 2015;152:272-6.
PubMed Abstract»Elkashef AM, Rawson RA, Anderson AL, et al. Bupropion for the treatment of methamphetamine dependence. Neuropsychopharmacology. 2008;33:1162-70.
PubMed Abstract»Gonzales R, Marinelli-Casey P, Shoptaw S, Ang A, Rawson RA. Hepatitis C virus infection among methamphetamine-dependent individuals in outpatient treatment. J Subst Abuse Treat. 2006;31:195-202.
PubMed Abstract»Grebely J, Dalgard O, Conway B, et al. Sofosbuvir and velpatasvir for hepatitis C virus infection in people with recent injection drug use (SIMPLIFY): an open-label, single-arm, phase 4, multicentre trial. Lancet Gastroenterol Hepatol. 2018;3:153-61.
PubMed Abstract»Hagan H, Jordan AE, Neurer J, Cleland CM. Incidence of sexually transmitted hepatitis C virus infection in HIV-positive men who have sex with men. AIDS. 2015;29:2335-45.
PubMed Abstract»Karila L, Weinstein A, Aubin HJ, Benyamina A, Reynaud M, Batki SL. Pharmacological approaches to methamphetamine dependence: a focused review. Br J Clin Pharmacol. 2010;69:578-92.
PubMed Abstract»Litwin AH, Lum PJ, Taylor LE, et al. Patient-centred models of hepatitis C treatment for people who inject drugs: a multicentre, pragmatic randomised trial. Lancet Gastroenterol Hepatol. 2022;7:1112-27.
PubMed Abstract»Meemken L, Hanhoff N, Tseng A, Christensen S, Gillessen A. Drug-Drug Interactions With Antiviral Agents in People Who Inject Drugs Requiring Substitution Therapy. Ann Pharmacother. 2015;49:796-807.
PubMed Abstract»Riley DE, Liu L, Cohen B, Robinson S, Groessl EJ, Ho SB. Characteristics and impact of methamphetamine use in patients with chronic hepatitis C. J Addict Med. 2014;8:25-32.
PubMed Abstract»Shearer J, Darke S, Rodgers C, et al. A double-blind, placebo-controlled trial of modafinil (200 mg/day) for methamphetamine dependence. Addiction. 2009;104:224-33.
PubMed Abstract»Trivedi MH, Walker R, Ling W, et al. Bupropion and Naltrexone in Methamphetamine Use Disorder. N Engl J Med. 2021;384:140-53.
PubMed Abstract»HCV Treatment in Persons who Consume Alcohol
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Anand BS, Currie S, Dieperink E, et al. Alcohol use and treatment of hepatitis C virus: results of a national multicenter study. Gastroenterology. 2006;130:1607-16.
PubMed Abstract»Bruggmann P, Dampz M, Gerlach T, Kravecz L, Falcato L. Treatment outcome in relation to alcohol consumption during hepatitis C therapy: an analysis of the Swiss Hepatitis C Cohort Study. Drug Alcohol Depend. 2010;110:167-71.
PubMed Abstract»Garbutt JC. The state of pharmacotherapy for the treatment of alcohol dependence. Journal of substance abuse treatment. 2009;36:S15-23; quiz S24-15.
PubMed Abstract»Innes HA, Hutchinson SJ, Barclay S, et al. Quantifying the fraction of cirrhosis attributable to alcohol among chronic HCV patients: Implications for treatment cost-effectiveness. Hepatology. 2012;57:451-60.
PubMed Abstract»Knight R, Roux P, Vilotitch A, et al. Significant reductions in alcohol use after hepatitis C treatment: results from the ANRS CO13-HEPAVIH cohort. Addiction. 2017;112:1669-1679.
PubMed Abstract»Le Lan C, Guillygomarc'h A, Danielou H, et al. A multi-disciplinary approach to treating hepatitis C with interferon and ribavirin in alcohol-dependent patients with ongoing abuse. J Hepatol. 2012;56:334-40.
PubMed Abstract»McMahon BJ, Bruden D, Bruce MG, et al. Adverse outcomes in Alaska Natives who recovered from or have chronic hepatitis C infection. Gastroenterology. 2010;138:922-31.
PubMed Abstract»Patel YA, Yao J, Proeschold-Bell RJ, Niedzwiecki D, Goacher E, Muir AJ. Reduced Alcohol Use Is Sustained in Patients Provided Alcohol-Related Counseling During Direct-Acting Antiviral Therapy for Hepatitis C. Dig Dis Sci. 2020 Sep 23. Online ahead of print.
PubMed Abstract»Perzynski AT, McCormick R, Webster NJ, et al. Psychosocial correlates of alcohol use and reduction for individuals with hepatitis C. Journal of studies on alcohol and drugs. 2011;72:787-98.
PubMed Abstract»Poynard T, Bedossa P, Opolon P. Lancet. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825-32.
PubMed Abstract»Russell M, Pauly MP, Moore CD, et al. The impact of lifetime alcohol use on hepatitis C treatment outcomes in privately insured members of an integrated health care plan. Hepatology. 2012;56:1223-30.
PubMed Abstract»Tsui JI, Williams EC, Green PK, Berry K, Su F, Ioannou GN. Alcohol use and hepatitis C virus treatment outcomes among patients receiving direct antiviral agents. Drug Alcohol Depend. 2016;169:101-9.
PubMed Abstract»Wiley TE, McCarthy M, Breidi L, McCarthy M, Layden TJ. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology. 1998;28:805-9.
PubMed Abstract»HCV Treatment in Persons who Use Cannabis
Brunet L, Moodie EE, Rollet K, et al. Marijuana smoking does not accelerate progression of liver disease in HIV-hepatitis C coinfection: A longitudinal cohort analysis. Clin Infect Dis. 2013;57:663-70.
PubMed Abstract»El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142:1264-1273.e1.
PubMed Abstract»Hézode C, Lonjon I, Roudot-Thoraval F, Mavier JP, Pawlotsky JM, Zafrani ES, Dhumeaux D. Impact of smoking on histological liver lesions in chronic hepatitis C. Gut. 2003;52:126-9.
PubMed Abstract»Ishida JH, Peters MG, Jin C, Louie K, Tan V, Bacchetti P, Terrault NA. Influence of cannabis use on severity of hepatitis C disease. Clin Gastroenterol Hepatol. 2008;6:69-75.
PubMed Abstract»Nordmann S, Vilotitch A, Roux P, et al. Daily cannabis and reduced risk of steatosis in human immunodeficiency virus and hepatitis C virus-co-infected patients (ANRS CO13-HEPAVIH). J Viral Hepat. 2018;25:171-179.
PubMed Abstract»Purohit V, Rapaka R, Shurtleff D. Role of cannabinoids in the development of fatty liver (steatosis). The AAPS journal. 2010;12:233-7.
PubMed Abstract»Sylvestre DL, Clements BJ, Malibu Y. Cannabis use improves retention and virological outcomes in patients treated for hepatitis C. Eur J Gastroenterol Hepatol. 2006;18:1057-63.
PubMed Abstract»Zimmermann T, Hueppe D, Mauss S, et al. Effects of Smoking on Pegylated Interferon alpha 2a and First Generation Protease Inhibitor-based Antiviral Therapy in Naïve Patients Infected with Hepatitis C Virus Genotype 1. J Gastrointestin Liver Dis. 2016;25:15-24.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Key populations: identification and management of HCV in people who inject drugs.
AASLD/IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. When and in whom to initiate HCV therapy.
AASLD-IDSA Hepatitis C Guidance»Akiyama MJ, Agyemang L, Arnsten JH, et al. Rationale, design, and methodology of a trial evaluating three models of care for HCV treatment among injection drug users on opioid agonist therapy. BMC Infect Dis. 2018;18:74.
PubMed Abstract»Bruggmann P, Dampz M, Gerlach T, Kravecz L, Falcato L. Treatment outcome in relation to alcohol consumption during hepatitis C therapy: an analysis of the Swiss Hepatitis C Cohort Study. Drug Alcohol Depend. 2010;110:167-71.
PubMed Abstract»Brunet L, Moodie EE, Rollet K, et al. Marijuana smoking does not accelerate progression of liver disease in HIV-hepatitis C coinfection: A longitudinal cohort analysis. Clin Infect Dis. 2013;57:663-70.
PubMed Abstract»Dore GJ, Altice F, Litwin AH, et al. Elbasvir-Grazoprevir to Treat Hepatitis C Virus Infection in Persons Receiving Opioid Agonist Therapy: A Randomized Trial. Ann Intern Med. 2016;165:625-634.
PubMed Abstract»Durham DP, Skrip LA, Bruce RD, et al. The Impact of Enhanced Screening and Treatment on Hepatitis C in the United States. Clin Infect Dis. 2015;62:298-304.
PubMed Abstract»Esmat G, El Raziky M, El Kassas M, Hassany M, Gamil ME. The future for the treatment of genotype 4 chronic hepatitis C. Liver Int. 2012;32 Suppl 1:146-50.
PubMed Abstract»Esmat G, Elbaz T, El Raziky M, et al. Effectiveness of ravidasvir plus sofosbuvir in interferon-naïve and treated patients with chronic hepatitis C genotype-4. J Hepatol. 2017.pii: S0168-8278(17)32286-9.
PubMed Abstract»Garbutt JC. The state of pharmacotherapy for the treatment of alcohol dependence. Journal of substance abuse treatment. 2009;36:S15-23; quiz S24-15.
PubMed Abstract»Grebely J, Dalgard O, Conway B, et al. Sofosbuvir and velpatasvir for hepatitis C virus infection in people with recent injection drug use (SIMPLIFY): an open-label, single-arm, phase 4, multicentre trial. Lancet Gastroenterol Hepatol. 2018;3:153-61.
PubMed Abstract»Grebely J, Dore GJ, Zeuzem S, et al. Efficacy and Safety of Sofosbuvir/Velpatasvir in Patients With Chronic Hepatitis C Virus Infection Receiving Opioid Substitution Therapy: Analysis of Phase 3 ASTRAL Trials. Clin Infect Dis. 2016;63:1479-1481.
PubMed Abstract»Grebely J, Hajarizadeh B, Dore GJ. Direct-acting antiviral agents for HCV infection affecting people who inject drugs. Nat Rev Gastroenterol Hepatol. 2017;14:641-651.
PubMed Abstract»Hafez E, Elbaz T, El Kassas M, Esmat G. A New Potent NS5A Inhibitor in the Management of Hepatitis C Virus: Ravidasvir. Curr Drug Discov Technol. 2018;15:24-31.
PubMed Abstract»Hagan H, Pouget ER, Des Jarlais DC. A systematic review and meta-analysis of interventions to prevent hepatitis C virus infection in people who inject drugs. J Infect Dis. 2011;204:74-83.
PubMed Abstract»Hajarizadeh B, Cunningham EB, Valerio H, et al. Hepatitis C reinfection after successful antiviral treatment among people who inject drugs: A meta-analysis. J Hepatol. 2020;72:643-57.
PubMed Abstract»Hajarizadeh B, Grebely J, Byrne M, et al. Evaluation of hepatitis C treatment-as-prevention within Australian prisons (SToP-C): a prospective cohort study. Lancet Gastroenterol Hepatol. 2021;6:533-46.
PubMed Abstract»Innes HA, Hutchinson SJ, Barclay S, et al. Quantifying the fraction of cirrhosis attributable to alcohol among chronic HCV patients: Implications for treatment cost-effectiveness. Hepatology. 2012;57:451-60.
PubMed Abstract»Ishida JH, Peters MG, Jin C, Louie K, Tan V, Bacchetti P, Terrault NA. Influence of cannabis use on severity of hepatitis C disease. Clin Gastroenterol Hepatol. 2008;6:69-75.
PubMed Abstract»Kosloski MP, Zhao W, Asatryan A, Kort J, Geoffroy P, Liu W. No Clinically Relevant Drug-Drug Interactions between Methadone or Buprenorphine-Naloxone and Antiviral Combination Glecaprevir and Pibrentasvir. Antimicrob Agents Chemother. 2017;61:e00958-17.
PubMed Abstract»Le Lan C, Guillygomarc'h A, Danielou H, et al. A multi-disciplinary approach to treating hepatitis C with interferon and ribavirin in alcohol-dependent patients with ongoing abuse. J Hepatol. 2012;56:334-40.
PubMed Abstract»Litwin AH, Lum PJ, Taylor LE, et al. Patient-centred models of hepatitis C treatment for people who inject drugs: a multicentre, pragmatic randomised trial. Lancet Gastroenterol Hepatol. 2022;7:1112-27.
PubMed Abstract»Martin NK, Hickman M, Hutchinson SJ, Goldberg DJ, Vickerman P. Combination interventions to prevent HCV transmission among people who inject drugs: modeling the impact of antiviral treatment, needle and syringe programs, and opiate substitution therapy. Clin Infect Dis. 2013;57 Suppl 2:S39-45.
PubMed Abstract»Martin NK, Vickerman P, Grebely J, et al. Hepatitis C virus treatment for prevention among people who inject drugs: Modeling treatment scale-up in the age of direct-acting antivirals. Hepatology. 2013;58:1598-609.
PubMed Abstract»McMahon BJ, Bruden D, Bruce MG, et al. Adverse outcomes in Alaska Natives who recovered from or have chronic hepatitis C infection. Gastroenterology. 2010;138:922-31.
PubMed Abstract»Nordmann S, Vilotitch A, Roux P, et al. Daily cannabis and reduced risk of steatosis in human immunodeficiency virus and hepatitis C virus-co-infected patients (ANRS CO13-HEPAVIH). J Viral Hepat. 2018;25:171-179.
PubMed Abstract»Norton BL, Fleming J, Bachhuber MA, et al. High HCV cure rates for people who use drugs treated with direct acting antiviral therapy at an urban primary care clinic. Int J Drug Policy. 2017;47:196-201.
PubMed Abstract»Olafsson S, Fridriksdottir RH, Love TJ, et al. Cascade of care during the first 36 months of the treatment as prevention for hepatitis C (TraP HepC) programme in Iceland: a population-based study. Lancet Gastroenterol Hepatol. 2021;6:628-37.
PubMed Abstract»Pockros PJ, Jensen D, Tsai N, et al. JUMP-C: a randomized trial of mericitabine plus pegylated interferon alpha-2a/ribavirin for 24 weeks in treatment-naïve HCV genotype 1/4 patients. Hepatology. 2013;58:514-23.
PubMed Abstract»Poynard T, Bedossa P, Opolon P. Lancet. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825-32.
PubMed Abstract»Purohit V, Rapaka R, Shurtleff D. Role of cannabinoids in the development of fatty liver (steatosis). The AAPS journal. 2010;12:233-7.
PubMed Abstract»Rossignol JF, Elfert A, El-Gohary Y, Keeffe EB. Improved virologic response in chronic hepatitis C genotype 4 treated with nitazoxanide, peginterferon, and ribavirin. Gastroenterology. 2009;136:856-62.
PubMed Abstract»Rossignol JF1, Elfert A, Keeffe EB. Treatment of chronic hepatitis C using a 4-week lead-in with nitazoxanide before peginterferon plus nitazoxanide. J Clin Gastroenterol. 2010;44:504-9.
PubMed Abstract»Russell M, Pauly MP, Moore CD, et al. The impact of lifetime alcohol use on hepatitis C treatment outcomes in privately insured members of an integrated health care plan. Hepatology. 2012;56:1223-30.
PubMed Abstract»Shehab HM, Elbaz TM, Deraz DM. Nitazoxanide plus pegylated interferon and ribavirin in the treatment of genotype 4 chronic hepatitis C, a randomized controlled trial. Liver Int. 2014;34:259-65.
PubMed Abstract»Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of Late Relapse or Reinfection With Hepatitis C Virus After Achieving a Sustained Virological Response: A Systematic Review and Meta-analysis. Clin Infect Dis. 2016;62:683-94.
PubMed Abstract»Sylvestre DL, Clements BJ, Malibu Y. Cannabis use improves retention and virological outcomes in patients treated for hepatitis C. Eur J Gastroenterol Hepatol. 2006;18:1057-63.
PubMed Abstract»Tsui JI, Evans JL, Lum PJ, Hahn JA, Page K. Association of opioid agonist therapy with lower incidence of hepatitis C virus infection in young adult injection drug users. JAMA Intern Med. 2014;174:1974-81.
PubMed Abstract»Tsui JI, Williams EC, Green PK, Berry K, Su F, Ioannou GN. Alcohol use and hepatitis C virus treatment outcomes among patients receiving direct antiviral agents. Drug Alcohol Depend. 2016;169:101-9.
PubMed Abstract»Wedemeyer H, Jensen D, Herring R Jr, et al. PROPEL: a randomized trial of mericitabine plus peginterferon alpha-2a/ribavirin therapy in treatment-naïve HCV genotype 1/4 patients. Hepatology. 2013;58:524-37.
PubMed Abstract»Wiley TE, McCarthy M, Breidi L, McCarthy M, Layden TJ. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology. 1998;28:805-9.
PubMed Abstract»Ye L, Peng JS, Wang X, Wang YJ, Luo GX, Ho WZ. Methamphetamine enhances Hepatitis C virus replication in human hepatocytes. J Viral Hepat. 2008;15:261-70.
PubMed Abstract»Zelenev A, Li J, Mazhnaya A, Basu S, Altice FL. Hepatitis C virus treatment as prevention in an extended network of people who inject drugs in the USA: a modelling study. Lancet Infect Dis. 2018;18:215-24.
PubMed Abstract»Zhong M, Peng E, Huang N, et al. Discovery of ravidasvir (PPI-668) as a potent pan-genotypic HCV NS5A inhibitor. Bioorg Med Chem Lett. 2016;26:4508-4512.
PubMed Abstract»Lesson 4. Treatment of HCV in a Correctional Setting
Epidemiology of HCV in Corrections
Coalition of Correctional Health Authorities American Correctional Association. Hepatitis C in Correctional Settings: Challenges and Opportunities
ACA»Denniston MM, Jiles RB, Drobeniuc J, et al. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med. 2014;160:293-300.
PubMed Abstract»Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015;62:1353-63.
PubMed Abstract»Hammett TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and releasees from US correctional facilities, 1997. Am J Public Health. 2002;92:1789-94.
PubMed Abstract»He T, Li K, Roberts MS, et al. Prevention of Hepatitis C by Screening and Treatment in U.S. Prisons. Ann Intern Med. 2016;164:84-92.
PubMed Abstract»Kim AY, Nagami EH, Birch CE, Bowen MJ, Lauer GM, McGovern BH. A simple strategy to identify acute hepatitis C virus infection among newly incarcerated injection drug users. Hepatology. 2013;57:944-52.
PubMed Abstract»Lewis KC, Barker LK, Jiles RB, Gupta N. Estimated Prevalence and Awareness of Hepatitis C Virus Infection Among US Adults: National Health and Nutrition Examination Survey, January 2017-March 2020. Clin Infect Dis. 2023;77:1413-5.
PubMed Abstract»Ruiz JD, Molitor F, Sun RK, et al. Prevalence and correlates of hepatitis C virus infection among inmates entering the California correctional system. West J Med. 1999;170:156-60.
PubMed Abstract»Spaulding A, Greene C, Davidson K, Schneidermann M, Rich J. Hepatitis C in state correctional facilities. Prev Med. 1999;28:92-100.
PubMed Abstract»Spaulding AC, Adee MG, Lawrence RT, Chhatwal J, von Oehsen W. Five Questions Concerning Managing Hepatitis C in the Justice System: Finding Practical Solutions for Hepatitis C Virus Elimination. Infect Dis Clin North Am. 2018;32:323-345.
PubMed Abstract»Spaulding AC, Anderson EJ, Khan MA, Taborda-Vidarte CA, Phillips JA. HIV and HCV in U.S. Prisons and Jails: The Correctional Facility as a Bellwether Over Time for the Community's Infections. AIDS Rev. 2017;19:134-147.
PubMed Abstract»Spaulding AC, Kennedy SS, Osei J, et al. Estimates of Hepatitis C Seroprevalence and Viremia in State Prison Populations in the United States. J Infect Dis. 2023;228:S160-S167.
PubMed Abstract»Varan AK, Mercer DW, Stein MS, Spaulding AC. Hepatitis C seroprevalence among prison inmates since 2001: still high but declining. Public Health Rep. 2014;129:187-95.
PubMed Abstract»Weinbaum C, Lyerla R, Margolis HS. Prevention and control of infections with hepatitis viruses in correctional settings. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2003;52:1-36.
PubMed Abstract»HCV Screening in Correctional Settings
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Key populations: HCV testing and treatment in correctional settings.
AASLD/IDSA Hepatitis C Guidance»Akiyama MJ, Kaba F, Rosner Z, Alper H, Holzman RS, MacDonald R. Hepatitis C Screening of the "Birth Cohort" (Born 1945-1965) and Younger Inmates of New York City Jails. Am J Public Health. 2016;106:1276-7.
PubMed Abstract»Assoumou SA, Tasillo A, Vellozzi C, et al. Cost-effectiveness and Budgetary Impact of Hepatitis C Virus Testing, Treatment, and Linkage to Care in US Prisons. Clin Infect Dis. 2020;70:1388-96.
PubMed Abstract»de la Flor C, Porsa E, Nijhawan AE. Opt-out HIV and Hepatitis C Testing at the Dallas County Jail: Uptake, Prevalence, and Demographic Characteristics of Testers. Public Health Rep. 2017;132:617-621.
PubMed Abstract»Denniston MM, Jiles RB, Drobeniuc J, et al. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med. 2014;160:293-300.
PubMed Abstract»Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015;62:1353-63.
PubMed Abstract»Federal Bureau of Prisons. Evaluation and management of chronic hepatitis C virus (HCV) infection. January 2018.
Federal Bureau of Prisons»Federal Bureau of Prisons. Evaluation and management of hepatitis C virus (HCV) infection. March 2021.
Federal Bureau of Prisons»Fox RK, Currie SL, Evans J, et al. Hepatitis C virus infection among prisoners in the California state correctional system. Clin Infect Dis. 2005;41:177-86.
PubMed Abstract»He T, Li K, Roberts MS, et al. Prevention of Hepatitis C by Screening and Treatment in U.S. Prisons. Ann Intern Med. 2016;164:84-92.
PubMed Abstract»Kuncio DE, Newbern EC, Fernandez-Viña MH, Herdman B, Johnson CC, Viner KM. Comparison of risk-based hepatitis C screening and the true seroprevalence in an urban prison system. J Urban Health. 2015;92:379-86.
PubMed Abstract»Larney S, Mahowald MK, Scharff N, Flanigan TP, Beckwith CG, Zaller ND. Epidemiology of hepatitis C virus in Pennsylvania state prisons, 2004-2012: limitations of 1945-1965 birth cohort screening in correctional settings. Am J Public Health. 2014;104:e69-74.
PubMed Abstract»Martin NK, Vickerman P, Dore GJ, Hickman M. The hepatitis C virus epidemics in key populations (including people who inject drugs, prisoners and MSM): the use of direct-acting antivirals as treatment for prevention. Curr Opin HIV AIDS. 2015;10:374-80.
PubMed Abstract»Morris MD, Brown B, Allen SA. Universal opt-out screening for hepatitis C virus (HCV) within correctional facilities is an effective intervention to improve public health. Int J Prison Health. 2017;13:192-199.
PubMed Abstract»Moyer VA; U.S. Preventive Services Task Force. Screening for hepatitis C virus infection in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:51-60.
PubMed Abstract»Rich JD, Allen SA, Williams BA. Responding to hepatitis C through the criminal justice system. N Engl J Med. 2014;370:1871-4.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Spaulding AC, Thomas DL. Screening for HCV infection in jails. JAMA. 2012;307:1259-60.
PubMed Abstract»US Preventive Services Task Force, Owens DK, Davidson KW, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;323:970-5.
PubMed Abstract»Varan AK, Mercer DW, Stein MS, Spaulding AC. Hepatitis C seroprevalence among prison inmates since 2001: still high but declining. Public Health Rep. 2014;129:187-95.
PubMed Abstract»Management of HCV in Jails versus Prisons
Kaeble D, Cowhig. Correctional Populations in the United States, 2016. Bureau of Justice Statistics; Washington, DC. April 2018.
Bureau of Justice Statistics»Maru DS, Bruce RD, Basu S, Altice FL. Clinical outcomes of hepatitis C treatment in a prison setting: feasibility and effectiveness for challenging treatment populations. Clin Infect Dis. 2008;47:952-61.
PubMed Abstract»Spaulding AC, Adee MG, Lawrence RT, Chhatwal J, von Oehsen W. Five Questions Concerning Managing Hepatitis C in the Justice System: Finding Practical Solutions for Hepatitis C Virus Elimination. Infect Dis Clin North Am. 2018;32:323-345.
PubMed Abstract»Spaulding AC, Thomas DL. Screening for HCV infection in jails. JAMA. 2012;307:1259-60.
PubMed Abstract»Spaulding AC, Weinbaum CM, Lau DT, et al. A framework for management of hepatitis C in prisons. Ann Intern Med. 2006;144:762-9.
PubMed Abstract»Spaulding AS, Kim AY, Harzke AJ, et al. Impact of new therapeutics for hepatitis C virus infection in incarcerated populations. Top Antivir Med. 2013;21:27-35.
PubMed Abstract»HCV Treatment Eligibility in Corrections
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Key populations: HCV testing and treatment in correctional settings.
AASLD/IDSA Hepatitis C Guidance»Asselah T, Marcellin P, Schinazi RF. Treatment of hepatitis C virus infection with direct-acting antiviral agents: 100% cure? Liver Int. 2018;38 Suppl 1:7-13.
PubMed Abstract»Beckman AL, Bilinski A, Boyko R, et al. New Hepatitis C Drugs Are Very Costly And Unavailable To Many State Prisoners. Health Aff (Millwood). 2016;35:1893-1901.
PubMed Abstract»Federal Bureau of Prisons. Evaluation and management of chronic hepatitis C virus (HCV) infection. January 2018.
Federal Bureau of Prisons»Federal Bureau of Prisons. Evaluation and management of hepatitis C virus (HCV) infection. March 2021.
Federal Bureau of Prisons»Hochstatter KR, Stockman LJ, Holzmacher R, et al. The continuum of hepatitis C care for criminal justice involved adults in the DAA era: a retrospective cohort study demonstrating limited treatment uptake and inconsistent linkage to community-based care. Health Justice. 2017;5:10.
PubMed Abstract»Interim Guidance for the Management of Chronic Hepatitis C Infection. Federal Bureau of Prisons Clinical Guidelines. June, 2014.
Federal Bureau of Prisons Clinical Guidelines.»Marcellin F, Roux P, Protopopescu C, Duracinsky M, Spire B, Carrieri MP. Patient-reported outcomes with direct-acting antivirals for the treatment of chronic hepatitis C: current knowledge and outstanding issues. Expert Rev Gastroenterol Hepatol. 2017;11:259-268.
PubMed Abstract»Rich JD, Allen SA, Williams BA. Responding to hepatitis C through the criminal justice system. N Engl J Med. 2014;370:1871-4.
PubMed Abstract»Roberts TD. Right to treatment for the civilly committed: a new Eighth Amendment basis. Univ Chic Law Rev. 1978;45:731-52.
PubMed Abstract»Rosenfeld J. The Origin of Prisoner's Rights: Estelle v. Gamble 429 U.S. 97;75-929 (1976).
National Law Review»Spaulding AC, Adee MG, Lawrence RT, Chhatwal J, von Oehsen W. Five Questions Concerning Managing Hepatitis C in the Justice System: Finding Practical Solutions for Hepatitis C Virus Elimination. Infect Dis Clin North Am. 2018;32:323-345.
PubMed Abstract»Spaulding AS, Kim AY, Harzke AJ, et al. Impact of new therapeutics for hepatitis C virus infection in incarcerated populations. Top Antivir Med. 2013;21:27-35.
PubMed Abstract»Sterling RK, Cherian R, Lewis S, et al. Treatment of HCV in the Department of Corrections in the Era of Oral Medications. J Correct Health Care. 2018;24:127-136.
PubMed Abstract»Providing HCV Treatment in Correctional Settings
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Key populations: HCV testing and treatment in correctional settings.
AASLD/IDSA Hepatitis C Guidance»Allen SA, Spaulding AC, Osei AM, Taylor LE, Cabral AM, Rich JD. Treatment of chronic hepatitis C in a state correctional facility. Ann Intern Med. 2003;138:187-90.
PubMed Abstract»Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364:2199-207.
PubMed Abstract»Federal Bureau of Prisons. Evaluation and management of chronic hepatitis C virus (HCV) infection. January 2018.
Federal Bureau of Prisons»Federal Bureau of Prisons. Evaluation and management of hepatitis C virus (HCV) infection. March 2021.
Federal Bureau of Prisons»Maru DS, Bruce RD, Basu S, Altice FL. Clinical outcomes of hepatitis C treatment in a prison setting: feasibility and effectiveness for challenging treatment populations. Clin Infect Dis. 2008;47:952-61.
PubMed Abstract»Mokkarala S, Johnson C, Sarkar S, Rudas RJ. Family Practitioner-Directed Hepatitis C Therapy With Direct-Acting Antivirals Achieves High-Sustained Virologic Response in Prison Population. J Correct Health Care. 2019;25:134-42.
PubMed Abstract»Rice JP, Burnett D, Tsotsis H, et al. Comparison of hepatitis C virus treatment between incarcerated and community patients. Hepatology. 2012;56:1252-60.
PubMed Abstract»Sterling RK, Cherian R, Lewis S, et al. Treatment of HCV in the Department of Corrections in the Era of Oral Medications. J Correct Health Care. 2018;24:127-136.
PubMed Abstract»Ongoing Care after HCV Treatment
Bate JP, Colman AJ, Frost PJ, Shaw DR, Harley HA. High prevalence of late relapse and reinfection in prisoners treated for chronic hepatitis C. J Gastroenterol Hepatol. 2010;25:1276-80.
PubMed Abstract»Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020-2.
PubMed Abstract»Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922-38.
AASLD Practice Guidelines»Grady BP, Schinkel J, Thomas XV, Dalgard O. Hepatitis C virus reinfection following treatment among people who use drugs. Clin Infect Dis. 2013;57 Suppl 2:S105-10.
PubMed Abstract»Hagan H, Pouget ER, Des Jarlais DC. A systematic review and meta-analysis of interventions to prevent hepatitis C virus infection in people who inject drugs. J Infect Dis. 2011;204:74-83.
PubMed Abstract»Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-80.
PubMed Abstract»Macalino GE, Vlahov D, Sanford-Colby S, et al. Prevalence and incidence of HIV, hepatitis B virus, and hepatitis C virus infections among males in Rhode Island prisons. Am J Public Health. 2004;94:1218-23.
PubMed Abstract»Marco A, Esteban JI, Solé C, et al. Hepatitis C virus reinfection among prisoners with sustained virological response after treatment for chronic hepatitis C. J Hepatol. 2013;59:45-51.
PubMed Abstract»Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of Late Relapse or Reinfection With Hepatitis C Virus After Achieving a Sustained Virological Response: A Systematic Review and Meta-analysis. Clin Infect Dis. 2016;62:683-694.
PubMed Abstract»Public Health Opportunity
He T, Li K, Roberts MS, et al. Prevention of Hepatitis C by Screening and Treatment in U.S. Prisons. Ann Intern Med. 2016;164:84-92.
PubMed Abstract»Hochstatter KR, Stockman LJ, Holzmacher R, et al. The continuum of hepatitis C care for criminal justice involved adults in the DAA era: a retrospective cohort study demonstrating limited treatment uptake and inconsistent linkage to community-based care. Health Justice. 2017;5:10.
PubMed Abstract»Martin NK, Vickerman P, Dore GJ, Hickman M. The hepatitis C virus epidemics in key populations (including people who inject drugs, prisoners and MSM): the use of direct-acting antivirals as treatment for prevention. Curr Opin HIV AIDS. 2015;10:374-80.
PubMed Abstract»Rich JD, Allen SA, Williams BA. Responding to hepatitis C through the criminal justice system. N Engl J Med. 2014;370:1871-4.
PubMed Abstract»Stone J, Martin NK, Hickman M, et al. Modelling the impact of incarceration and prison-based hepatitis C virus (HCV) treatment on HCV transmission among people who inject drugs in Scotland. Addiction. 2017;112:1302-1314.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection.
AASLD-IDSA Hepatitis C Guidance»Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364:2199-207.
PubMed Abstract»Bate JP, Colman AJ, Frost PJ, Shaw DR, Harley HA. High prevalence of late relapse and reinfection in prisoners treated for chronic hepatitis C. J Gastroenterol Hepatol. 2010;25:1276-80.
PubMed Abstract»Beckwith CG, Kurth AE, Bazerman LB, et al. A pilot study of rapid hepatitis C virus testing in the Rhode Island Department of Corrections. J Public Health (Oxf). 2016;38:130-7.
PubMed Abstract»Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015;62:1353-63.
PubMed Abstract»Grady BP, Schinkel J, Thomas XV, Dalgard O. Hepatitis C virus reinfection following treatment among people who use drugs. Clin Infect Dis. 2013;57 Suppl 2:S105-10.
PubMed Abstract»Hagan H, Pouget ER, Des Jarlais DC. A systematic review and meta-analysis of interventions to prevent hepatitis C virus infection in people who inject drugs. J Infect Dis. 2011;204:74-83.
PubMed Abstract»Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-80.
PubMed Abstract»Larney S, Zaller ND, Dumont DM, Willcock A, Degenhardt L. A systematic review and meta-analysis of racial and ethnic disparities in hepatitis C antibody prevalence in United States correctional populations. Ann Epidemiol. 2016;26:570-578.e2.
PubMed Abstract»Lewis KC, Barker LK, Jiles RB, Gupta N. Estimated Prevalence and Awareness of Hepatitis C Virus Infection Among US Adults: National Health and Nutrition Examination Survey, January 2017-March 2020. Clin Infect Dis. 2023;77:1413-5.
PubMed Abstract»MacDonald R, Akiyama MJ, Kopolow A, et al. Feasibility of Treating Hepatitis C in a Transient Jail Population. Open Forum Infect Dis. 2017 Summer;4:ofx142.
PubMed Abstract»Mahowald MK, Larney S, Zaller ND, et al. Characterizing the Burden of Hepatitis C Infection Among Entrants to Pennsylvania State Prisons, 2004 to 2012. J Correct Health Care. 2016;22:41-5.
PubMed Abstract»Martin NK, Vickerman P, Dore GJ, Hickman M. The hepatitis C virus epidemics in key populations (including people who inject drugs, prisoners and MSM): the use of direct-acting antivirals as treatment for prevention. Curr Opin HIV AIDS. 2015;10:374-80.
PubMed Abstract»McGovern BH, Wurcel A, Kim AY, et al. Acute hepatitis C virus infection in incarcerated injection drug users. Clin Infect Dis. 2006;42:1663-70.
PubMed Abstract»Rich JD, Chandler R, Williams BA, et al. How health care reform can transform the health of criminal justice-involved individuals. Health Aff (Millwood). 2014;33:462-7.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Schoenbachler BT, Smith BD, Seña AC, et al. Hepatitis C Virus Testing and Linkage to Care in North Carolina and South Carolina Jails, 2012-2014. Public Health Rep. 2016;131 Suppl 2:98-104.
PubMed Abstract»Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of Late Relapse or Reinfection With Hepatitis C Virus After Achieving a Sustained Virological Response: A Systematic Review and Meta-analysis. Clin Infect Dis. 2016;62:683-694.
PubMed Abstract»US Preventive Services Task Force, Owens DK, Davidson KW, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;323:970-5.
PubMed Abstract»Lesson 5. Management of Health Care Personnel Exposed to HCV
Background
Boal WL, Leiss JK, Sousa S, Lyden JT, Li J, Jagger J. The national study to prevent blood exposure in paramedics: exposure reporting. Am J Ind Med. 2008;51:213-22.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Workbook for Designing, Implementing, and Evaluating a Sharps Injury Prevention Program. 2008
CDC»Dement JM, Epling C, Ostbye T, Pompeii LA, Hunt DL. Blood and body fluid exposure risks among health care workers: results from the Duke Health and Safety Surveillance System. Am J Ind Med. 2004;46:637-48.
PubMed Abstract»Egro FM, Nwaiwu CA, Smith S, Harper JD, Spiess AM. Seroconversion rates among health care workers exposed to hepatitis C virus-contaminated body fluids: The University of Pittsburgh 13-year experience. Am J Infect Control. 2017;45:1001-1005.
PubMed Abstract»Gerberding JL. Management of occupational exposures to blood-borne viruses. N Engl J Med. 1995;332:444-51.
PebMed Abstract»Gershon RR, Pearson JM, Sherman MF, Samar SM, Canton AN, Stone PW. The prevalence and risk factors for percutaneous injuries in registered nurses in the home health care sector. Am J Infect Control. 2009;37:525-33.
PubMed Abstract»Gershon RR, Qureshi KA, Pogorzelska M, et al. Non-hospital based registered nurses and the risk of bloodborne pathogen exposure. Ind Health. 2007;45:695-704.
PubMed Abstract»International Safety Center. 2022 EPINet Report for Needlestick and Sharp Object Injuries
International Safety Center»International Safety Center. EPINet Sharps Injury and Blood and Body Fluids Exposure Surveillance Research Group. Sharps Injury Data Report for 1998-2011
International Safety Center»Moorman AC, de Perio MA, Goldschmidt R, et al. Testing and Clinical Management of Health Care Personnel Potentially Exposed to Hepatitis C Virus - CDC Guidance, United States, 2020. MMWR Recomm Rep. 2020;69:1-8.
PubMed Abstract»Panlilio AL, Orelien JG, Srivastava PU, Jagger J, Cohn RD, Cardo DM. Estimate of the annual number of percutaneous injuries among hospital-based healthcare workers in the United States, 1997-1998. Infect Control Hosp Epidemiol. 2004;25:556-62.
PubMed Abstract»Schillie S, Murphy TV, Sawyer M, et al. CDC guidance for evaluating health-care personnel for hepatitis B virus protection and for administering postexposure management. MMWR Recomm Rep. 2013;62:1-19.
PubMed Abstract»U.S. Public Health Service. Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HBV, HCV, and HIV and Recommendations for Postexposure Prophylaxis. MMWR Recomm Rep. 2001;50:1-52.
PubMed Abstract»Yun J, Umemoto K, Wang W, Vyas D. National Survey of Sharps Injuries Incidence Amongst Healthcare Workers in the United States. Int J Gen Med. 2023;16:1193-1204.
PubMed Abstract»Risk of HCV Following Occupational Exposure
Bukh J, Meuleman P, Tellier R, et al. Challenge pools of hepatitis C virus genotypes 1-6 prototype strains: replication fitness and pathogenicity in chimpanzees and human liver-chimeric mouse models. J Infect Dis. 2010;201:1381-9.
PubMed Abstract»Egro FM, Nwaiwu CA, Smith S, Harper JD, Spiess AM. Seroconversion rates among health care workers exposed to hepatitis C virus-contaminated body fluids: The University of Pittsburgh 13-year experience. Am J Infect Control. 2017;45:1001-1005.
PubMed Abstract»Farías A, Ré V, Mengarelli S, et al. Detection of hepatitis C virus (HCV) in body fluids from HCV monoinfected and HCV/HIV coinfected patients. Hepatogastroenterology. 2010;57:300-4.
PubMed Abstract»Lin HH, Kao JH, Hsu HY, et al. Possible role of high-titer maternal viremia in perinatal transmission of hepatitis C virus. J Infect Dis. 1994;169:638-41.
PubMed Abstract»Moorman AC, de Perio MA, Goldschmidt R, et al. Testing and Clinical Management of Health Care Personnel Potentially Exposed to Hepatitis C Virus - CDC Guidance, United States, 2020. MMWR Recomm Rep. 2020;69:1-8.
PubMed Abstract»Naggie S, Holland DP, Sulkowski MS, Thomas DL. Hepatitis C Virus Postexposure Prophylaxis in the Healthcare Worker: Why Direct-Acting Antivirals Don't Change a Thing. Clin Infect Dis. 2017;64:92-99.
PubMed Abstract»Ohto H, Terazawa S, Sasaki N, et al. Transmission of hepatitis C virus from mothers to infants. The Vertical Transmission of Hepatitis C Virus Collaborative Study Group. N Engl J Med. 1994;330:744-50.
PubMed Abstract»Rey D, Fritsch S, Schmitt C, Meyer P, Lang JM, Stoll-Keller F. Quantitation of hepatitis C virus RNA in saliva and serum of patients coinfected with HCV and human immunodeficiency virus. J Med Virol. 2001;63:117-9.
PubMed Abstract»Savasi V, Parrilla B, Ratti M, Oneta M, Clerici M, Ferrazzi E. Hepatitis C virus RNA detection in different semen fractions of HCV/HIV-1 co-infected men by nested PCR. Eur J Obstet Gynecol Reprod Biol. 2010;151:52-5.
PubMed Abstract»Tomkins SE, Elford J, Nichols T, et al. Occupational transmission of hepatitis C in healthcare workers and factors associated with seroconversion: UK surveillance data. J Viral Hepat. 2012;19:199-204.
PubMed Abstract»U.S. Public Health Service. Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HBV, HCV, and HIV and Recommendations for Postexposure Prophylaxis. MMWR Recomm Rep. 2001;50:1-52.
PubMed Abstract»Yazdanpanah Y, De Carli G, Migueres B, et al. Risk factors for hepatitis C virus transmission to health care workers after occupational exposure: a European case-control study. Clin Infect Dis. 2005;41:1423-30.
PubMed Abstract»Approach to Managing Occupational Exposures to HCV
Abara WE, Collier MG, Moorman A, et al. Characteristics of Deceased Solid Organ Donors and Screening Results for Hepatitis B, C, and Human Immunodeficiency Viruses - United States, 2010-2017. MMWR Morb Mortal Wkly Rep. 2019;68:61-6.
PubMed Abstract»Association of Public Health Laboratories. Interpretation of Hepatitis C Virus Test Results: Guidance for Laboratories. January 2019.
APHL»Centers for Disease Control and Prevention (CDC). 2019 Viral Hepatitis Surveillance Report—Hepatitis C. Published May 2021.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Centers for Disease Control and Prevention (CDC). Testing for HCV infection: an update of guidance for clinicians and laboratorians. MMWR Morb Mortal Wkly Rep. 2013;62:362-5.
PubMed Abstract»Egro FM, Nwaiwu CA, Smith S, Harper JD, Spiess AM. Seroconversion rates among health care workers exposed to hepatitis C virus-contaminated body fluids: The University of Pittsburgh 13-year experience. Am J Infect Control. 2017;45:1001-1005.
PubMed Abstract»Moorman AC, de Perio MA, Goldschmidt R, et al. Testing and Clinical Management of Health Care Personnel Potentially Exposed to Hepatitis C Virus - CDC Guidance, United States, 2020. MMWR Recomm Rep. 2020;69:1-8.
PubMed Abstract»Naggie S, Holland DP, Sulkowski MS, Thomas DL. Hepatitis C Virus Postexposure Prophylaxis in the Healthcare Worker: Why Direct-Acting Antivirals Don't Change a Thing. Clin Infect Dis. 2017;64:92-99.
PubMed Abstract»Schillie S, Murphy TV, Sawyer M, et al. CDC guidance for evaluating health-care personnel for hepatitis B virus protection and for administering postexposure management. MMWR Recomm Rep. 2013;62:1-19.
PubMed Abstract»U.S. Public Health Service. Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HBV, HCV, and HIV and Recommendations for Postexposure Prophylaxis. MMWR Recomm Rep. 2001;50:1-52.
PubMed Abstract»Monitoring Health Care Personnel after Occupational Exposure
Association of Public Health Laboratories. Interpretation of Hepatitis C Virus Test Results: Guidance for Laboratories. January 2019.
APHL»Glynn SA, Wright DJ, Kleinman SH, et al. Dynamics of viremia in early hepatitis C virus infection. Transfusion. 2005;45:994-1002.
PubMed Abstract»Gruener NH, Heeg M, Obermeier M, et al. Late appearance of hepatitis C virus RNA after needlestick injury: necessity for a more intensive follow-up. Infect Control Hosp Epidemiol. 2009;30:299-300.
PubMed Abstract»Hajarizadeh B, Grebely J, Applegate T, et al. Dynamics of HCV RNA levels during acute hepatitis C virus infection. J Med Virol. 2014;86:1722-9.
PubMed Abstract»Moorman AC, de Perio MA, Goldschmidt R, et al. Testing and Clinical Management of Health Care Personnel Potentially Exposed to Hepatitis C Virus - CDC Guidance, United States, 2020. MMWR Recomm Rep. 2020;69:1-8.
PubMed Abstract»Page K, Osburn W, Evans J, et al. Frequent longitudinal sampling of hepatitis C virus infection in injection drug users reveals intermittently detectable viremia and reinfection. Clin Infect Dis. 2013;56:405-13.
PubMed Abstract»Villano SA, Vlahov D, Nelson KE, Cohn S, Thomas DL. Persistence of viremia and the importance of long-term follow-up after acute hepatitis C infection. Hepatology. 1999;29:908-14.
PubMed Abstract»Management of Persons who Seroconvert to HCV
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: management of acute HCV infection.
AASLD-IDSA Hepatitis C Guidance»Deterding K, Spinner CD, Schott E, et al. Ledipasvir plus sofosbuvir fixed-dose combination for 6 weeks in patients with acute hepatitis C virus genotype 1 monoinfection (HepNet Acute HCV IV): an open-label, single-arm, phase 2 study. Lancet Infect Dis. 2017;17:215-22.
PubMed Abstract»Moorman AC, de Perio MA, Goldschmidt R, et al. Testing and Clinical Management of Health Care Personnel Potentially Exposed to Hepatitis C Virus - CDC Guidance, United States, 2020. MMWR Recomm Rep. 2020;69:1-8.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection: treatment-naive genotype 5 or 6.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Initial treatment of HCV infection.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: management of acute HCV infection.
AASLD-IDSA Hepatitis C Guidance»Abergel A, Asselah T, Metivier S, et al. Ledipasvir-sofosbuvir in patients with hepatitis C virus genotype 5 infection: an open-label, multicentre, single-arm, phase 2 study. Lancet Infect Dis. 2016;16:459-64.
PubMed Abstract»Antaki N, Abboud D, Antaki F, Craxi A. HCV genotype 5: an orphan virus. Antivir Ther. 2013;18:263-9.
PubMed Abstract»Antaki N, Hermes A, Hadad M, Ftayeh M, Antaki F, Abdo N, Kebbewar K. Efficacy of interferon plus ribavirin in the treatment of hepatitis C virus genotype 5. J Viral Hepat. 2008;15:383-6.
PubMed Abstract»Asselah T, Kowdley KV, Zadeikis N, et al. Efficacy of Glecaprevir/Pibrentasvir for 8 or 12 Weeks in Patients With Hepatitis C Virus Genotype 2, 4, 5, or 6 Infection Without Cirrhosis. Clin Gastroenterol Hepatol. 2018;16:417-26.
PubMed Abstract»Bonny C, Fontaine H, Poynard T, et al Effectiveness of interferon plus ribavirin combination in the treatment of naive patients with hepatitis C virus type 5. A French multicentre retrospective study. Aliment Pharmacol Ther. 2006;24:593-600.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Centers for Disease Control and Prevention (CDC). Testing for HCV infection: an update of guidance for clinicians and laboratorians. MMWR Morb Mortal Wkly Rep. 2013;62:362-5.
PubMed Abstract»D'Heygere F, George C, Van Vlierberghe H, et al. Efficacy of interferon-based antiviral therapy in patients with chronic hepatitis C infected with genotype 5: a meta-analysis of two large prospective clinical trials. J Med Virol. 2011;83:815-9.
PubMed Abstract»Deterding K, Spinner CD, Schott E, et al. Ledipasvir plus sofosbuvir fixed-dose combination for 6 weeks in patients with acute hepatitis C virus genotype 1 monoinfection (HepNet Acute HCV IV): an open-label, single-arm, phase 2 study. Lancet Infect Dis. 2017;17:215-22.
PubMed Abstract»Devaki P, Jencks D, Yee BE, Nguyen MH. Sustained virologic response to standard interferon or pegylated interferon and ribavirin in patients with hepatitis C virus genotype 5: systematic review and meta-analysis of ten studies and 423 patients. Hepatol Int. 2015;9:431-7.
PubMed Abstract»European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C: Final update of the series☆. J Hepatol. 2020:S0168-8278(20)30548-1.
EASL»Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 1, 2, 4, 5, and 6 Infection. N Engl J Med. 2015;373:2599-607.
PubMed Abstract»Forns X, Lee SS, Valdes J, et al. Glecaprevir plus pibrentasvir for chronic hepatitis C virus genotype 1, 2, 4, 5, or 6 infection in adults with compensated cirrhosis (EXPEDITION-1): a single-arm, open-label, multicentre phase 3 trial. Lancet Infect Dis. 2017;17:1062-1068.
PubMed Abstract»Gane EJ, Hyland RH, An D, et al. Efficacy of ledipasvir and sofosbuvir, with or without ribavirin, for 12 weeks in patients with HCV genotype 3 or 6 infection. Gastroenterology. 2015;149:1454-1461.e1.
PubMed Abstract»Glynn SA, Wright DJ, Kleinman SH, et al. Dynamics of viremia in early hepatitis C virus infection. Transfusion. 2005;45:994-1002.
PubMed Abstract»Kowdley KV, Lawitz E, Crespo I, et al. Sofosbuvir with pegylated interferon alfa-2a and ribavirin for treatment-naive patients with hepatitis C genotype-1 infection (ATOMIC): an open-label, randomised, multicentre phase 2 trial. Lancet. 2013;381:2100-7.
PubMed Abstract»Kwo PY, Poordad F, Asatryan A, et al. Glecaprevir and pibrentasvir yield high response rates in patients with HCV genotype 1-6 without cirrhosis. J Hepatol. 2017;67:263-271.
PubMed Abstract»Lam KD, Trinh HN, Do ST, et. al. Randomized controlled trial of pegylated interferon-alfa 2a and ribavirin in treatment-naive chronic hepatitis C genotype 6. Hepatology 2010;52:1573-80.
PubMed Abstract»Lawitz E, Mangia A, Wyles D, et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med. 2013;368:1878-87.
PubMed Abstract»Legrand-Abravanel F, Sandres-Sauné K, Barange K, et al. Hepatitis C virus genotype 5: epidemiological characteristics and sensitivity to combination therapy with interferon-alpha plus ribavirin. J Infect Dis. 2004;189:1397-400.
PubMed Abstract»Lenz O, Vijgen L, Berke JM, et al. Virologic response and characterisation of HCV genotype 2-6 in patients receiving TMC435 monotherapy (study TMC435-C202). J Hepatol. 2013;58:445-51.
PubMed Abstract»Mauss S, Berger F, Vogel M, et al. Treatment results of chronic hepatitis C genotype 5 and 6 infections in Germany. Z Gastroenterol. 2012;50:441-4.
PubMed Abstract»Nguyen MH, Trinh HN, Garcia R, Nguyen G, Lam KD, Keeffe EB. Higher rate of sustained virologic response in chronic hepatitis C genotype 6 treated with 48 weeks versus 24 weeks of peginterferon plus ribavirin. Am J Gastroenterol. 2008;103:1131-5.
PubMed Abstract»Ohto H, Terazawa S, Sasaki N, et al. Transmission of hepatitis C virus from mothers to infants. The Vertical Transmission of Hepatitis C Virus Collaborative Study Group. N Engl J Med. 1994;330:744-50.
PubMed Abstract»Papastergiou V, Skorda L, Lisgos P, et. al. Hepatitis C virus genotype 5: prospective evaluation of peginterferon/ribavirin treatment efficacy and predictive value of on-treatment virological responses for sustained virological response. J Clin Gastroenterol. 2014;48:160-5.
PubMed Abstract»Thuy PT, Bunchorntavakul C, Tan Dat H, Rajender Reddy K. A randomized trial of 48 versus 24 weeks of combination pegylated interferon and ribavirin therapy in genotype 6 chronic hepatitis C. J Hepatol. 2012;56:1012-8.
PubMed Abstract»Wang X, Liu F, Wei F, Ren H, Hu H. Efficacy and safety of pegylated interferon plus ribavirin therapy for chronic hepatitis C genotype 6: a meta-analysis. PLoS One. 2014;9:e100128.
PubMed Abstract»Wantuck JM, Ahmed A, Nguyen MH. Review article: the epidemiology and therapy of chronic hepatitis C genotypes 4, 5 and 6. Aliment Pharmacol Ther. 2014;39:137-47.
PubMed Abstract»Lesson 6. Perinatal HCV Transmission
Background
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»Bélec L, Legoff J, Si-Mohamed A, Bloch F, Matta M, Mbopi-Keou FX, Payan C. Cell-associated, non-replicating strand(+) hepatitis C virus-RNA shedding in cervicovaginal secretions from chronically HCV-infected women. J Clin Virol. 2003;27:247-51.
PubMed Abstract»Boaz K, Fiore AE, Schrag SJ, Gonik B, Schulkin J. Screening and counseling practices reported by obstetrician-gynecologists for patients with hepatitis C virus infection. Infect Dis Obstet Gynecol. 2003;11:39-44.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). 2019 Viral Hepatitis Surveillance Report—Hepatitis C. Published May 2021.
CDC»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Chaillon A, Rand EB, Reau N, Martin NK. Cost-effectiveness of Universal Hepatitis C Virus Screening of Pregnant Women in the United States. Clin Infect Dis. 2019;69:1888-95.
PubMed Abstract»Ely DM, Gregory ECW. Trends and Characteristics in Maternal Hepatitis C Virus Infection Rates During Pregnancy: United States, 2016–2021. National Vital Statistics Reports. 2023:72(3).
CDC Stacks»Ly KN, Jiles RB, Teshale EH, Foster MA, Pesano RL, Holmberg SD. Hepatitis C Virus Infection Among Reproductive-Aged Women and Children in the United States, 2006 to 2014. Ann Intern Med. 2017;166:775-782.
PubMed Abstract»Panagiotakopoulos L, Sandul AL, Conners EE, Foster MA, Nelson NP, Wester C. CDC Recommendations for Hepatitis C Testing Among Perinatally Exposed Infants and Children - United States, 2023. MMWR Recomm Rep. 2023;72:1-21.
PubMed Abstract»Rosenberg ES, Hall EW, Sullivan PS, et al. Estimation of State-Level Prevalence of Hepatitis C Virus Infection, US States and District of Columbia, 2010. Clin Infect Dis. 2017;64:1573-81.
PubMed Abstract»Rosenberg ES, Rosenthal EM, Hall EW, et al. Prevalence of Hepatitis C Virus Infection in US States and the District of Columbia, 2013 to 2016. JAMA Netw Open. 2018;1:e186371.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Schillie SF, Canary L, Koneru A, et al. Hepatitis C Virus in Women of Childbearing Age, Pregnant Women, and Children. Am J Prev Med. 2018;55:633-41.
PubMed Abstract»US Preventive Services Task Force, Owens DK, Davidson KW, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;323:970-5.
PubMed Abstract»Waruingi W, Mhanna MJ, Kumar D, Abughali N. Hepatitis C Virus universal screening versus risk based selective screening during pregnancy. J Neonatal Perinatal Med. 2015;8:371-8.
PubMed Abstract»HCV Screening During Pregnancy
Chaillon A, Rand EB, Reau N, Martin NK. Cost-effectiveness of Universal Hepatitis C Virus Screening of Pregnant Women in the United States. Clin Infect Dis. 2019;69:1888-95.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Factors Associated with HCV Perinatal Transmission
Ades AE, Gordon F, Scott K, et al. Overall Vertical Transmission of Hepatitis C Virus, Transmission Net of Clearance, and Timing of Transmission. Clin Infect Dis. 2023;76:905-12.
PubMed Abstract»Benova L, Mohamoud YA, Calvert C, Abu-Raddad LJ. Vertical transmission of hepatitis C virus: systematic review and meta-analysis. Clin Infect Dis. 2014;59:765-73.
PubMed Abstract»Ceci O, Margiotta M, Marello F, et al. Vertical transmission of hepatitis C virus in a cohort of 2,447 HIV-seronegative pregnant women: a 24-month prospective study. J Pediatr Gastroenterol Nutr. 2001;33:570-5.
PubMed Abstract»Cottrell EB, Chou R, Wasson N, Rahman B, Guise JM. Reducing risk for mother-to-infant transmission of hepatitis C virus: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;158:109-13.
PubMed Abstract»Dal Molin G, D'Agaro P, Ansaldi F, et al. Mother-to-infant transmission of hepatitis C virus: rate of infection and assessment of viral load and IgM anti-HCV as risk factors. J Med Virol. 2002;67:137-42.
PubMed Abstract»European Paediatric Hepatitis C Virus Network. A significant sex--but not elective cesarean section--effect on mother-to-child transmission of hepatitis C virus infection. J Infect Dis. 2005;192:1872-9.
PubMed Abstract»European Paediatric Hepatitis C Virus Network. Effects of mode of delivery and infant feeding on the risk of mother-to-child transmission of hepatitis C virus. European Paediatric Hepatitis C Virus Network. BJOG. 2001;108:371-7.
PubMed Abstract»Gibb DM, Goodall RL, Dunn DT, et al. Mother-to-child transmission of hepatitis C virus: evidence for preventable peripartum transmission. Lancet. 2000;356:904-7.
PubMed Abstract»Granovsky MO, Minkoff HL, Tess BH, et al. Hepatitis C virus infection in the mothers and infants cohort study. Pediatrics. 1998;102:355-9.
PubMed Abstract»Indolfi G, Resti M. Perinatal transmission of hepatitis C virus infection. J Med Virol. 2009;81:836-43.
PubMed Abstract»Mast EE, Hwang LY, Seto DS, Nolte FS, Nainan OV, Wurtzel H, Alter MJ. Risk factors for perinatal transmission of hepatitis C virus (HCV) and the natural history of HCV infection acquired in infancy. J Infect Dis. 2005;192:1880-9.
PubMed Abstract»Mok J, Pembrey L, Tovo PA, Newell ML. When does mother to child transmission of hepatitis C virus occur? Arch Dis Child Fetal Neonatal Ed. 2005;90:F156-60.
PubMed Abstract»Moriya T, Sasaki F, Mizui M, et al. Transmission of hepatitis C virus from mothers to infants: its frequency and risk factors revisited. Biomed Pharmacother. 1995;49:59-64.
PubMed Abstract»Ohto H, Terazawa S, Sasaki N, et al. Transmission of hepatitis C virus from mothers to infants. The Vertical Transmission of Hepatitis C Virus Collaborative Study Group. N Engl J Med. 1994;330:744-50.
PubMed Abstract»Okamoto M, Nagata I, Murakami J, et al. Prospective reevaluation of risk factors in mother-to-child transmission of hepatitis C virus: high virus load, vaginal delivery, and negative anti-NS4 antibody. J Infect Dis. 2000;182:1511-4.
PubMed Abstract»Paccagnini S, Principi N, Massironi E, et al. Perinatal transmission and manifestation of hepatitis C virus infection in a high risk population. Pediatr Infect Dis J. 1995;14:195-9.
PubMed Abstract»Page CM, Hughes BL, Rhee EHJ, Kuller JA. Hepatitis C in Pregnancy: Review of Current Knowledge and Updated Recommendations for Management. Obstet Gynecol Surv. 2017;72:347-355.
PubMed Abstract»Panagiotakopoulos L, Sandul AL, Conners EE, Foster MA, Nelson NP, Wester C. CDC Recommendations for Hepatitis C Testing Among Perinatally Exposed Infants and Children - United States, 2023. MMWR Recomm Rep. 2023;72:1-21.
PubMed Abstract»Post JJ. Update on hepatitis C and implications for pregnancy. Obstet Med. 2017;10:157-160.
PubMed Abstract»Resti M, Azzari C, Galli L, et al. Maternal drug use is a preeminent risk factor for mother-to-child hepatitis C virus transmission: results from a multicenter study of 1372 mother-infant pairs. J Infect Dis. 2002;185:567-72.
PubMed Abstract»Resti M, Azzari C, Mannelli F, et al. Mother to child transmission of hepatitis C virus: prospective study of risk factors and timing of infection in children born to women seronegative for HIV-1. Tuscany Study Group on Hepatitis C Virus Infection. BMJ. 1998;317:437-41.
PubMed Abstract»Terrault NA, Levy MT, Cheung KW, Jourdain G. Viral hepatitis and pregnancy. Nat Rev Gastroenterol Hepatol. 2020 Oct 12. [Online ahead of print]
PubMed Abstract»Thomas DL, Villano SA, Riester KA, et al. Perinatal transmission of hepatitis C virus from human immunodeficiency virus type 1-infected mothers. Women and Infants Transmission Study. J Infect Dis. 1998;177:1480-8.
PubMed Abstract»Tovo PA, Palomba E, Ferraris G, Principi N, Ruga E, Dallacasa P, Maccabruni A. Increased risk of maternal-infant hepatitis C virus transmission for women coinfected with human immunodeficiency virus type 1. Italian Study Group for HCV Infection in Children. Clin Infect Dis. 1997;25:1121-4.
PubMed Abstract»US Preventive Services Task Force, Owens DK, Davidson KW, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;323:970-5.
PubMed Abstract»Yeung LT, King SM, Roberts EA. Mother-to-infant transmission of hepatitis C virus. Hepatology. 2001;34:223-9.
PubMed Abstract»Zanetti AR, Tanzi E, Paccagnini S, et al. Mother-to-infant transmission of hepatitis C virus. Lombardy Study Group on Vertical HCV Transmission. Lancet. 1995;345:289-91.
PubMed Abstract»Impact of Chronic HCV Infection on Pregnancy
Belay T, Woldegiorgis H, Gress T, Rayyan Y. Intrahepatic cholestasis of pregnancy with concomitant hepatitis C virus infection, Joan C. Edwards SOM, Marshall University. Eur J Gastroenterol Hepatol. 2015;27:372-4.
PubMed Abstract»Connell LE, Salihu HM, Salemi JL, August EM, Weldeselasse H, Mbah AK. Maternal hepatitis B and hepatitis C carrier status and perinatal outcomes. Liver Int. 2011;31:1163-70.
PubMed Abstract»Hood RB, Miller WC, Shoben A, Harris RE, Norris AH. Maternal Hepatitis C Virus Infection and Adverse Newborn Outcomes in the US. Matern Child Health J. 2023:1343-51.
PubMed Abstract»Huang QT, Huang Q, Zhong M, et al. Chronic hepatitis C virus infection is associated with increased risk of preterm birth: a meta-analysis of observational studies. J Viral Hepat. 2015;22:1033-42.
PubMed Abstract»Hughes BL, Page CM, Kuller JA. Hepatitis C in pregnancy: screening, treatment, and management. Am J Obstet Gynecol. 2017 Nov;217:B2-B12.
PubMed Abstract»Money D, Boucoiran I, Wagner E, et al. Obstetrical and neonatal outcomes among women infected with hepatitis C and their infants. J Obstet Gynaecol Can. 2014;36:785-94.
PubMed Abstract»Pergam SA, Wang CC, Gardella CM, Sandison TG, Phipps WT, Hawes SE. Pregnancy complications associated with hepatitis C: data from a 2003-2005 Washington state birth cohort. Am J Obstet Gynecol. 2008;199:38.e1-9.
PubMed Abstract»Puljic A, Salati J, Doss A, Caughey AB. Outcomes of pregnancies complicated by liver cirrhosis, portal hypertension, or esophageal varices. J Matern Fetal Neonatal Med. 2016;29:506-9.
PubMed Abstract»Rezk M, Omar Z. Deleterious impact of maternal hepatitis-C viral infection on maternal and fetal outcome: a 5-year prospective study. Arch Gynecol Obstet. 2017;296:1097-1102.
PubMed Abstract»Terrault NA, Levy MT, Cheung KW, Jourdain G. Viral hepatitis and pregnancy. Nat Rev Gastroenterol Hepatol. 2020 Oct 12. [Online ahead of print]
PubMed Abstract»Wijarnpreecha K, Thongprayoon C, Sanguankeo A, Upala S, Ungprasert P, Cheungpasitporn W. Hepatitis C infection and intrahepatic cholestasis of pregnancy: A systematic review and meta-analysis. Clin Res Hepatol Gastroenterol. 2017;41:39-45.
PubMed Abstract»Effect of Pregnancy on Chronic HCV
Conte D, Fraquelli M, Prati D, Colucci A, Minola E. Prevalence and clinical course of chronic hepatitis C virus (HCV) infection and rate of HCV vertical transmission in a cohort of 15,250 pregnant women. Hepatology. 2000;31:751-5.
PubMed Abstract»Di Martino V, Lebray P, Myers RP, et al. Progression of liver fibrosis in women infected with hepatitis C: long-term benefit of estrogen exposure. Hepatology. 2004;40:1426-33.
PubMed Abstract»Fontaine H, Nalpas B, Carnot F, Bréchot C, Pol S. Effect of pregnancy on chronic hepatitis C: a case-control study. Lancet. 2000;356:1328-9.
PubMed Abstract»Hashem M, Jhaveri R, Saleh DA, et al. Spontaneous Viral Load Decline and Subsequent Clearance of Chronic Hepatitis C Virus in Postpartum Women Correlates With Favorable Interleukin-28B Gene Allele. Clin Infect Dis. 2017;65:999-1005.
PubMed Abstract»Hattori Y, Orito E, Ohno T, et al. Loss of hepatitis C virus RNA after parturition in female patients with chronic HCV infection. J Med Virol. 2003;71:205-11.
PubMed Abstract»Lin HH, Kao JH. Hepatitis C virus load during pregnancy and puerperium. BJOG. 2000;107:1503-6.
PubMed Abstract»Interventions to Prevent Mother-to-Child Transmission of HCV
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: HCV in pregnancy
AASLD/IDSA Hepatitis C Guidance»Chappell CA, Scarsi KK, Kirby BJ, et al. Ledipasvir plus sofosbuvir in pregnant women with hepatitis C virus infection: a phase 1 pharmacokinetic study. Lancet Microbe. 2020;1:e200-e208.
PubMed Abstract»Chappell CA. Safety, Tolerability, and Outcomes of SofosbuviR/Velpatasvir in Treatment of Chronic Hepatitis C Virus during Pregnancy: Interim results from the STORC study. AASLD The Liver Meeting; Abstract 0222. San Diego. Nov 15-19; 2024.
The Liver Meeting»European Paediatric Hepatitis C Virus Network. A significant sex--but not elective cesarean section--effect on mother-to-child transmission of hepatitis C virus infection. J Infect Dis. 2005;192:1872-9.
PubMed Abstract»Mast EE, Hwang LY, Seto DS, Nolte FS, Nainan OV, Wurtzel H, Alter MJ. Risk factors for perinatal transmission of hepatitis C virus (HCV) and the natural history of HCV infection acquired in infancy. J Infect Dis. 2005;192:1880-9.
PubMed Abstract»Post JJ. Update on hepatitis C and implications for pregnancy. Obstet Med. 2017;10:157-160.
PubMed Abstract»Resti M, Azzari C, Galli L, et al. Maternal drug use is a preeminent risk factor for mother-to-child hepatitis C virus transmission: results from a multicenter study of 1372 mother-infant pairs. J Infect Dis. 2002;185:567-72.
PubMed Abstract»Schillie SF, Canary L, Koneru A, et al. Hepatitis C Virus in Women of Childbearing Age, Pregnant Women, and Children. Am J Prev Med. 2018;55:633-41.
PubMed Abstract»Society for Maternal-Fetal Medicine (SMFM), Hughes BL, Page CM, Kuller JA. Hepatitis C in pregnancy: screening, treatment, and management. Am J Obstet Gynecol. 2017;217:B2-B12.
PubMed Abstract»Terrault NA, Levy MT, Cheung KW, Jourdain G. Viral hepatitis and pregnancy. Nat Rev Gastroenterol Hepatol. 2020 Oct 12. [Online ahead of print]
PubMed Abstract»Yattoo GN, Shafi SM, Dar GA, et al. Safety and efficacy of treatment for chronic hepatitis C during pregnancy: A prospective observational study in Srinagar, India. Clin Liver Dis (Hoboken). 2023;22:134-9.
PubMed Abstract»Safety of HCV Treatment During Pregnancy and Breastfeeding
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: HCV in pregnancy
AASLD/IDSA Hepatitis C Guidance»Chappell CA, Scarsi KK, Kirby BJ, et al. Ledipasvir plus sofosbuvir in pregnant women with hepatitis C virus infection: a phase 1 pharmacokinetic study. Lancet Microbe. 2020;1:e200-e208.
PubMed Abstract»Chappell CA. Safety, Tolerability, and Outcomes of SofosbuviR/Velpatasvir in Treatment of Chronic Hepatitis C Virus during Pregnancy: Interim results from the STORC study. AASLD The Liver Meeting; Abstract 0222. San Diego. Nov 15-19; 2024.
The Liver Meeting»Freriksen JJM, van Seyen M, Judd A, et al. Review article: direct-acting antivirals for the treatment of HCV during pregnancy and lactation - implications for maternal dosing, foetal exposure, and safety for mother and child. Aliment Pharmacol Ther. 2019;50:738-50.
PubMed Abstract»Kushner T, Lange M, Sperling R, Dieterich D. Treatment of Women With Hepatitis C Diagnosed in Pregnancy: a Co-Located Treatment Approach. Gastroenterology. 2022;163:1454-6.
PubMed Abstract»Terrault NA, Levy MT, Cheung KW, Jourdain G. Viral hepatitis and pregnancy. Nat Rev Gastroenterol Hepatol. 2020 Oct 12. [Online ahead of print]
PubMed Abstract»Yattoo GN, Shafi SM, Dar GA, et al. Safety and efficacy of treatment for chronic hepatitis C during pregnancy: A prospective observational study in Srinagar, India. Clin Liver Dis (Hoboken). 2023;22:134-9.
PubMed Abstract»Monitoring of Pregnant Women with HCV
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: HCV in pregnancy
AASLD/IDSA Hepatitis C Guidance»Society for Maternal-Fetal Medicine (SMFM), Hughes BL, Page CM, Kuller JA. Hepatitis C in pregnancy: screening, treatment, and management. Am J Obstet Gynecol. 2017;217:B2-B12.
PubMed Abstract»Terrault NA, Levy MT, Cheung KW, Jourdain G. Viral hepatitis and pregnancy. Nat Rev Gastroenterol Hepatol. 2020 Oct 12. [Online ahead of print]
PubMed Abstract»Management of Infants and Children Born to Mothers with HCV Infection
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: HCV in children
AASLD/IDSA Hepatitis C Guidance»Bal A, Petrova A. Single Clinical Practice's Report of Testing Initiation, Antibody Clearance, and Transmission of Hepatitis C Virus (HCV) in Infants of Chronically HCV-Infected Mothers. Open Forum Infect Dis. 2016;3:ofw021.
PubMed Abstract»Chappell CA, Hillier SL, Crowe D, Meyn LA, Bogen DL, Krans EE. Hepatitis C Virus Screening Among Children Exposed During Pregnancy. Pediatrics. 2018;141:e20173273.
PubMed Abstract»Hillemanns P, Dannecker C, Kimmig R, Hasbargen U. Obstetric risks and vertical transmission of hepatitis C virus infection in pregnancy. Acta Obstet Gynecol Scand. 2000;79:543-7.
PubMed Abstract»Kuncio DE, Newbern EC, Johnson CC, Viner KM. Failure to Test and Identify Perinatally Infected Children Born to Hepatitis C Virus-Infected Women. Clin Infect Dis. 2016;62:980-5.
PubMed Abstract»Panagiotakopoulos L, Sandul AL, Conners EE, Foster MA, Nelson NP, Wester C. CDC Recommendations for Hepatitis C Testing Among Perinatally Exposed Infants and Children - United States, 2023. MMWR Recomm Rep. 2023;72:1-21.
PubMed Abstract»Polywka S, Pembrey L, Tovo PA, Newell ML. Accuracy of HCV-RNA PCR tests for diagnosis or exclusion of vertically acquired HCV infection. J Med Virol. 2006;78:305-10.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Additional References
AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. HCV testing and linkage to care.
AASLD-IDSA Hepatitis C Guidance»AASLD-IDSA. HCV Guidance: Recommendations for testing, management, and treating hepatitis C. Unique populations: HCV in pregnancy
AASLD/IDSA Hepatitis C Guidance»Ades AE, Gordon F, Scott K, et al. Overall Vertical Transmission of Hepatitis C Virus, Transmission Net of Clearance, and Timing of Transmission. Clin Infect Dis. 2023;76:905-12.
PubMed Abstract»Benova L, Mohamoud YA, Calvert C, Abu-Raddad LJ. Vertical transmission of hepatitis C virus: systematic review and meta-analysis. Clin Infect Dis. 2014;59:765-73.
PubMed Abstract»Ceci O, Margiotta M, Marello F, et al. Vertical transmission of hepatitis C virus in a cohort of 2,447 HIV-seronegative pregnant women: a 24-month prospective study. J Pediatr Gastroenterol Nutr. 2001;33:570-5.
PubMed Abstract»Centers for Disease Control and Prevention (CDC). Hepatitis C Surveillance 2021. Published August 2023.
CDC»Chappell CA, Scarsi KK, Kirby BJ, et al. Ledipasvir plus sofosbuvir in pregnant women with hepatitis C virus infection: a phase 1 pharmacokinetic study. Lancet Microbe. 2020;1:e200-e208.
PubMed Abstract»Checa Cabot CA, Stoszek SK, Quarleri J, et al. Mother-to-Child Transmission of Hepatitis C Virus (HCV) Among HIV/HCV-Coinfected Women. J Pediatric Infect Dis Soc. 2013;2:126-35.
PubMed Abstract»Cottrell EB, Chou R, Wasson N, Rahman B, Guise JM. Reducing risk for mother-to-infant transmission of hepatitis C virus: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;158:109-13.
PubMed Abstract»Ely DM, Gregory ECW. Trends and Characteristics in Maternal Hepatitis C Virus Infection Rates During Pregnancy: United States, 2016–2021. National Vital Statistics Reports. 2023:72(3).
CDC Stacks»European Paediatric Hepatitis C Virus Network. A significant sex--but not elective cesarean section--effect on mother-to-child transmission of hepatitis C virus infection. J Infect Dis. 2005;192:1872-9.
PubMed Abstract»Hashem M, Jhaveri R, Saleh DA, et al. Spontaneous Viral Load Decline and Subsequent Clearance of Chronic Hepatitis C Virus in Postpartum Women Correlates With Favorable Interleukin-28B Gene Allele. Clin Infect Dis. 2017;65:999-1005.
PubMed Abstract»Hattori Y, Orito E, Ohno T, et al. Loss of hepatitis C virus RNA after parturition in female patients with chronic HCV infection. J Med Virol. 2003;71:205-11.
PubMed Abstract»Honegger JR, Kim S, Price AA, et al. Loss of immune escape mutations during persistent HCV infection in pregnancy enhances replication of vertically transmitted viruses. Nat Med. 2013;19:1529-33.
PubMed Abstract»Indolfi G, Resti M. Perinatal transmission of hepatitis C virus infection. J Med Virol. 2009;81:836-43.
PubMed Abstract»Jhaveri R, Hashem M, El-Kamary SS, et al. Hepatitis C Virus (HCV) Vertical Transmission in 12-Month-Old Infants Born to HCV-Infected Women and Assessment of Maternal Risk Factors. Open Forum Infect Dis. 2015;2:ofv089.
PubMed Abstract»Koneru A, Nelson N, Hariri S, et al. Increased Hepatitis C Virus (HCV) Detection in Women of Childbearing Age and Potential Risk for Vertical Transmission - United States and Kentucky, 2011-2014. MMWR Morb Mortal Wkly Rep. 2016;65:705-10.
PubMed Abstract»Kuncio DE, Newbern EC, Johnson CC, Viner KM. Failure to Test and Identify Perinatally Infected Children Born to Hepatitis C Virus-Infected Women. Clin Infect Dis. 2016;62:980-5.
PubMed Abstract»Kushner T, Chappell CA, Kim AY. Testing for Hepatitis C in Pregnancy: the Time has Come for Routine Rather than Risk-based. Curr Hepatol Rep. 2019;18:206-15.
PubMed Abstract»Lin HH, Kao JH. Hepatitis C virus load during pregnancy and puerperium. BJOG. 2000;107:1503-6.
PubMed Abstract»Ly KN, Jiles RB, Teshale EH, Foster MA, Pesano RL, Holmberg SD. Hepatitis C Virus Infection Among Reproductive-Aged Women and Children in the United States, 2006 to 2014. Ann Intern Med. 2017;166:775-782.
PubMed Abstract»Mast EE, Hwang LY, Seto DS, Nolte FS, Nainan OV, Wurtzel H, Alter MJ. Risk factors for perinatal transmission of hepatitis C virus (HCV) and the natural history of HCV infection acquired in infancy. J Infect Dis. 2005;192:1880-9.
PubMed Abstract»Ohto H, Terazawa S, Sasaki N, et al. Transmission of hepatitis C virus from mothers to infants. The Vertical Transmission of Hepatitis C Virus Collaborative Study Group. N Engl J Med. 1994;330:744-50.
PubMed Abstract»Page CM, Hughes BL, Rhee EHJ, Kuller JA. Hepatitis C in Pregnancy: Review of Current Knowledge and Updated Recommendations for Management. Obstet Gynecol Surv. 2017;72:347-355.
PubMed Abstract»Panagiotakopoulos L, Sandul AL, Conners EE, Foster MA, Nelson NP, Wester C. CDC Recommendations for Hepatitis C Testing Among Perinatally Exposed Infants and Children - United States, 2023. MMWR Recomm Rep. 2023;72:1-21.
PubMed Abstract»Plunkett BA, Grobman WA. Routine hepatitis C virus screening in pregnancy: a cost-effectiveness analysis. Am J Obstet Gynecol. 2005;192:1153-61.
PubMed Abstract»Polis CB, Shah SN, Johnson KE, Gupta A. Impact of maternal HIV coinfection on the vertical transmission of hepatitis C virus: a meta-analysis. Clin Infect Dis. 2007;44:1123-31.
PubMed Abstract»Post JJ. Update on hepatitis C and implications for pregnancy. Obstet Med. 2017;10:157-160.
PubMed Abstract»Resti M, Azzari C, Galli L, et al. Maternal drug use is a preeminent risk factor for mother-to-child hepatitis C virus transmission: results from a multicenter study of 1372 mother-infant pairs. J Infect Dis. 2002;185:567-72.
PubMed Abstract»Roberts SS, Miller RK, Jones JK, et al. The Ribavirin Pregnancy Registry: Findings after 5 years of enrollment, 2003-2009. Birth Defects Res A Clin Mol Teratol. 2010;88:551-9.
PubMed Abstract»Rosenberg ES, Rosenthal EM, Hall EW, et al. Prevalence of Hepatitis C Virus Infection in US States and the District of Columbia, 2013 to 2016. JAMA Netw Open. 2018;1:e186371.
PubMed Abstract»Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17.
PubMed Abstract»Tasillo A, Eftekhari Yazdi G, Nolen S, et al. Short-Term Effects and Long-Term Cost-Effectiveness of Universal Hepatitis C Testing in Prenatal Care. Obstet Gynecol. 2019;133:289-300.
PubMed Abstract»Thomas DL, Villano SA, Riester KA, et al. Perinatal transmission of hepatitis C virus from human immunodeficiency virus type 1-infected mothers. Women and Infants Transmission Study. J Infect Dis. 1998;177:1480-8.
PubMed Abstract»US Preventive Services Task Force, Owens DK, Davidson KW, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;323:970-5.
PubMed Abstract»Watts T, Stockman L, Martin J, Guilfoyle S, Vergeront JM. Increased Risk for Mother-to-Infant Transmission of Hepatitis C Virus Among Medicaid Recipients - Wisconsin, 2011-2015. MMWR Morb Mortal Wkly Rep. 2017;66:1136-1139.
PubMed Abstract»Yattoo GN, Shafi SM, Dar GA, et al. Safety and efficacy of treatment for chronic hepatitis C during pregnancy: A prospective observational study in Srinagar, India. Clin Liver Dis (Hoboken). 2023;22:134-9.
PubMed Abstract»Zeng QL, Yu ZJ, Lv J, et al. Sofosbuvir-based therapy for late pregnant women and infants with severe chronic hepatitis C: A case series study. J Med Virol. 2022;94:4548-53.
PubMed Abstract»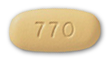 Elbasvir-Grazoprevir Zepatier
Elbasvir-Grazoprevir Zepatier Glecaprevir-Pibrentasvir Mavyret
Glecaprevir-Pibrentasvir Mavyret Ledipasvir-Sofosbuvir Harvoni
Ledipasvir-Sofosbuvir Harvoni Ribavirin Copegus, Rebetol, Ribasphere
Ribavirin Copegus, Rebetol, Ribasphere Sofosbuvir Sovaldi
Sofosbuvir Sovaldi Sofosbuvir-Velpatasvir Epclusa
Sofosbuvir-Velpatasvir Epclusa Sofosbuvir-Velpatasvir-Voxilaprevir Vosevi
Sofosbuvir-Velpatasvir-Voxilaprevir Vosevi